Back to Journals » International Journal of Women's Health » Volume 14
Slightly Elevated Progesterone on HCG Trigger Day Has an Impact on Pregnancy Outcomes of Fresh Single Blastocyst Transfer Cycles Under an Early Follicular Phase Prolonged Protocol Cycle
Authors Wei L, Zhao Y, Xu C , Zhang C
Received 7 August 2022
Accepted for publication 6 December 2022
Published 19 December 2022 Volume 2022:14 Pages 1761—1768
DOI https://doi.org/10.2147/IJWH.S385362
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Longlong Wei,1,2 Yan Zhao,2 Chunyu Xu,1,2 Cuilian Zhang1,2
1Zhengzhou University People’s Hospital, Zhengzhou, People’s Republic of China; 2Department of Reproductive Medicine Center, Henan Provincial People’s Hospital, Zhengzhou, People’s Republic of China
Correspondence: Cuilian Zhang, Department of Reproductive Medicine Center, Henan Provincial People’s Hospital, Zhengzhou, People’s Republic of China, Email [email protected]
Background: The effect of premature progesterone elevation on assisted reproductive technology has been debated. In different ovarian stimulation protocols, ovarian responses, and embryos transferred, conflicting results reside regarding the impact of elevated progesterone on pregnancy outcomes, according to previous studies. In addition, most studies have focused on significantly elevated progesterone levels, eg, above 1.5ng/mL, 1.75ng/mL, 2ng/mL. However, studies focusing on levels that are just slightly elevated are lacking, and some have concluded that such levels have no adverse effects on pregnancy outcomes.
Methods: Clinical data of patients who underwent early follicular phase prolonged protocol cycle in vitro fertilization/intracytoplasmic sperm injection treatment were collected. Patients were divided into two groups according to progesterone level on the trigger day of human chorionic gonadotropin (HCG): Group 1: < 1.0ng/mL and Group 2: 1.0– 1.5ng/mL. Differences in baseline characteristics, ovulation promotion, and embryo culture, along with clinical pregnancy outcomes, were compared between the two cohorts.
Results: A total of 743 participants were included in this study, of which 587 were included in Group 1 and 156 were included in Group 2. In terms of pregnancy outcomes, Group 2 had a significantly lower clinical pregnancy rate and live birth rate per cycle than Group 1 (64.1% vs 75.7%, p < 0.05; 63.5% vs 72.7%, p < 0.05). After correction for maternal age, maternal body mass index, infertility duration, basal follicle-stimulating hormone, anti-Müllerian hormone, antral follicle count, total dose of gonadotropin, days of stimulation, and estradiol level on HCG trigger day, slightly elevated progesterone levels (P > 1.0ng/mL) remained a risk factor for pregnancy failure in fresh single D5 blastocyst transfer under an early follicular phase prolonged protocol cycle.
Conclusion: Slightly elevated progesterone levels on HCG trigger day may negatively affect pregnancy outcomes in early follicular phase prolonged protocol cycles.
Keywords: progesterone, IVF-ET, early follicular phase prolonged protocol, perinatal outcome
Introduction
In women who undergo ovarian stimulation, the incidence of progesterone elevation on the HCG trigger day fluctuates at 38%, although the application of gonadotropin-releasing hormone (GnRH) analogs could significantly reduce the incidence of premature luteinization.1
There is no uniform standard for the definition of elevated progesterone levels on HCG trigger day, and it may vary according to ovarian response, developmental stage of embryo at transfer, and type of GnRH analog used for the prevention of a spontaneous surge of luteinizing hormone (LH).2 Although the cut-off values for the possible adverse effects of progesterone level on pregnancy outcomes range from 0.8 to 2.5ng/mL, according to the literature,2–5 most studies suggest that the clinical pregnancy rate is reduced and a “freeze-all” strategy is recommend when the progesterone level is above 1.5ng/mL.6–9 More refined studies are urgently needed regarding possible progesterone thresholds. These should include several identification parameters (eg, patient characteristics, type of ovarian response, stimulation protocol).2 Answering this question will facilitate a reliable assessment of the prognosis of each subfertile couple.
The objective of this study was to evaluate whether a slightly elevated progesterone level (1.0–1.5ng/mL) on HCG trigger day has an adverse effect on clinical pregnancy under an early follicular phase prolonged protocol cycle.
Materials and Methods
Study Population and design
This retrospective study collected data from 743 cycles of fresh in vitro fertilization/intracytoplasmic sperm injection and embryo transfer (IVF/ICSI-ET) under an early follicular phase prolonged protocol from January 2017 to October 2020 at a single reproductive center. This study was reviewed and approved by the Institutional Review Board and Ethics Committee of Henan Provincial People’s Hospital, China (approval number: SYSZ-LL-2021091501). This study was conducted in accordance with the Declaration of Helsinki, as revised in 1983.
The inclusion criteria were as follows: (1) 20–40 years old; (2) single D5 blastocyst transfer; (3) endometrial thickness on trigger day was greater than 6 mm; (4) progesterone level was ≤ 1.5ng/mL on trigger day. The exclusion criteria were as follows: (1) endometrial polyp, uterine anomaly, endometriosis, adenomyosis, and hydrosalpinx; (2) incomplete data; (3) time of egg retrieval ≥ 3; (4) chromosomal abnormalities in any of the couples (including chromosome polymorphisms); and (5) testicular sperm retrieval.
Patient-related clinical data that strictly met the inclusion criteria were retrieved from the software database of the Clinical Assisted Reproductive Technology Management System in the department. Here, 743 women were divided into two groups according to progesterone level: Group 1: P < 1.0ng/mL (n = 587); Group 2: 1.0 ≤ P ≤ 1.5ng/mL (n = 156).
Progesterone Measurement
Serum progesterone levels were measured on the day of the HCG trigger. Samples were tested using a microparticle enzyme immunoassay Axsym System (Abbott Cientifica S.A., Madrid, Spain), and the lower limit of detection for the assay was 0.05ng/mL. In addition to the internal quality control checks performed daily by the institution laboratory, the assays were calibrated whenever a new reactive batch was used or when an outcome outside the normal range was observed.
Ovarian Stimulation and Embryo Culture
Long-acting GnRH-a 3.75 mg (Triptorelin Acetate for injection, IPSEN PHARMA BIOTECH, H20140298) was administered intramuscularly on days 2–4 of the menstrual cycle. Blood hormone levels and ultrasound were measured 28 to 30 days later to determine whether the criteria for down-regulation were met. The criteria for down-regulation were as follows: serum follicle-stimulating hormone (FSH) < 5mIU/mL, LH < 5mIU/mL, estradiol (E2) < 50pg/mL, progesterone (P) < 1ng/mL, endometrial thickness < 5mm, ovarian follicles < 10mm in diameter, and no luteal cysts. After downregulation was achieved, ovarian stimulation was initiated with a starting dose of 75–300 IU, depending on the age of the patient, antral follicle count (AFC), basal sex hormone, anti-Müllerian hormone (AMH), body mass index (BMI), and previous ovarian responsiveness. When follicles ≥ 18 mm in diameter accounted for 50–60% of the dominant follicles, the HCG trigger was administered at a dose of 4000–12000IU.
Depending on the quality of male semen, IVF or ICSI techniques were selected for fertilization, followed by transfer to a culture medium for embryo culture. Embryonic oocyte cleavage was observed 70–72h after fertilization, and blastocyst scoring was performed using the Gardner scoring system.
Luteal Phase Support
Routine luteal support was performed from the day of egg retrieval, with 30mg oral dydrogesterone tablets (Duphaston, Abbott Biologicals B. V., H20170221) and progesterone sustained-release vaginal gel (Fleet Laboratories Limited, H20140552) 90mg placed vaginally. On day 5 after egg retrieval, high-scoring blastocysts were selected for embryo transfer according to embryo status and the patient’s specific condition.
Peripheral blood was collected from the patient 14 days after embryo transfer to measure the β-hCG levels. Transvaginal ultrasound was performed to evaluate embryo implantation after day 28–35 of fresh single blastocyst transfer (SBT), and the presence of a pregnancy sac was identified as a clinical pregnancy. If clinical pregnancy was confirmed, luteal support was continued until approximately 12 weeks gestation. If embryo loss or loss of fetal heartbeat occurred, it was marked as an abortion.
Statistical Analysis
Continuous variables of normal distribution were expressed as mean ± standard deviation (mean ± SD), and the t-test was used to conduct the statistical analyses. Variables of non-normal distribution were presented as median ± quartile range (median ± QR), and the Mann–Whitney U-test was used to conduct the statistical analyses. Categorical variables are expressed in frequency and percentage (%), and the chi-square test was used to compare the percentages. A multivariate logistic regression model was used to examine the preferential effects of progesterone on pregnancy outcomes. Maternal age, maternal BMI, infertility duration, basal FSH, AMH, AFC, total dose of gonadotropin (Gn), days of stimulation, and E2 level on the day of HCG trigger were included in the multivariable regression model. SPSS 23.0 was implied to carry out the statistical analysis, and p < 0.05 was considered as statistically significant.
Results
In this study, we analyzed 743 fresh SBT cycles under an early follicular phase prolonged protocol and compared clinical outcomes between the two groups. Demographic data such as age, infertility duration, BMI, and AMH are summarized in Table 1. The baseline information was similar across the two groups, except for BMI. BMI decreased as progesterone levels increased on trigger day.
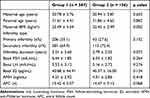 |
Table 1 Baseline Characteristics of Two Groups |
When performing controlled ovarian stimulation (COS) under the prolonged protocol, Group 2 had a higher total dose of Gn (2608.29 ± 969.91 vs 2301.12 ± 914.51, p = 0.001). And the days of stimulation were higher in Group 2(12.39 ± 3.14 vs 11.68 ± 2.29, p = 0.001). E2 levels on the day of trigger were higher in Group 2 (2216.01 ± 932.93 vs 1732.49 ± 763.99, p = 0.001) (Table 2).
 |
Table 2 Controlled Ovarian Hypersimulation Procedure |
The laboratory results showed that Group 2 had higher number of retrieved oocytes, double pronuclear (2PNs) and MII oocytes (13.78 ± 4.36 vs 12.41 ± 4.26, 9.28 ± 3.15 vs 8.41 ± 3.13, 12.21 ± 3.87 vs 11.05 ± 3.86; p < 0.001) (Table 3). Comparison of the grades of blastocyst cavity expansion, inner cell mass, and trophoblastic layer showed no significant differences. Blastocyst cavity expansion was almost the 4th degree in the two groups.
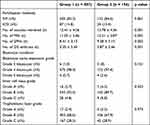 |
Table 3 Laboratory Outcomes of the Two Groups |
Although both cohorts showed fairly good pregnancy outcomes, the group with slightly elevated progesterone levels still had significantly lower clinical pregnancy and live birth rates than those with normal progesterone levels (64.1% vs 75.5%, 63.5% vs 72.7%, respectively; all p < 0.05) (Table 4).
 |
Table 4 Clinical Outcomes of the Two Groups |
A multivariate logistic regression model was used to examine the effects of slightly elevated progesterone levels on pregnancy outcomes. After correction for maternal age, maternal BMI, infertility duration, basal FSH, AMH, AFC, total dose of Gn, days of stimulation, and E2 level on the day of HCG trigger, slightly elevated progesterone levels remained a risk factor for lower clinical pregnancy and live birth rates (Table 5).
 |
Table 5 Logistic Regression Analysis Focused on Pregnancy Outcomes Under Different Levels of Progesterone on HCG Trigger Day |
Discussion
Most studies strongly support the idea that a premature rise in progesterone levels on HCG trigger days during ovarian stimulation is associated with reduced implantation and pregnancy rates following fresh embryo transfers. However, there is no uniform standard for the definition of elevated progesterone level on HCG trigger days. Premature progesterone rise is defined as serum progesterone ≥ 1.0ng/mL.10–12 A meta-analysis including over 60,000 cycles also showed that progesterone seems to have a detrimental effect on the probability of pregnancy achievement in women undergoing fresh IVF cycles, with progesterone concentrations of 0.8ng/mL.2 However, many clinicians are doubtful of this low progesterone threshold. Bosch defined 1.5ng/mL as the threshold of elevated progesterone and concluded that the pregnancy outcome was negatively affected above this value and that fresh embryo transfer should be cancelled. This is also the most widely accepted threshold.6–8,13–15 However, few studies have analyzed whether just a slight elevation in progesterone level (1.0–1.5ng/mL) has a detrimental effect on the outcomes. In clinical practice, we observed that progesterone levels between 1.0 and 1.5 seem to have an adverse effect on pregnancy outcome, and we determined these two thresholds according to the literature and clinical practice. For the first time, this study compared the clinical outcomes of slightly elevated progesterone—progesterone at 1.0–1.5ng/mL—with those of normal progesterone—progesterone less than 1.0ng/mL—in an early follicular phase prolonged protocol.
The mechanism causing elevated progesterone on the trigger day during COS is unclear but is currently believed to be related to the following factors:3–5,9,15 (1) excess mature follicles; (2) high Gn dose (Bosch et al found that for every 75 U increase in FSH, the risk of elevated progesterone on HCG trigger days increased 1.44-fold); (3) high LH; (4) prolonged ovarian stimulation; and (5) different ovulation promotion protocols. GnRH agonist protocols were most associated with extreme elevations of progesterone. In the present study, total dose of Gn, days of stimulation, E2 levels on HCG trigger day, and number of oocytes retrieved in Group 2 were all higher than those in Group 1, which is consistent with the results of most of the above studies. In addition, the women in Group 1 (P < 1.0ng/mL) had a higher BMI, and there was a statistical difference between the two groups (23.49 ± 3.54 vs 22.45 ± 2.99, p = 0.002), suggesting that women with low BMI are more likely to have elevated progesterone. It is possible that a higher BMI corresponds to higher aromatase expression and, consequently, greater estrogen production, which could impact progesterone production.16 Although the “freeze-all” strategy can avoid the effects of high progesterone levels on pregnancy outcomes, there is no consensus regarding the safety and long-term prognosis of this strategy. Therefore, careful selection of the dose of ovulation-stimulating drugs and reduction of the duration of stimulation time are particularly important for preventing premature elevated progesterone on HCG trigger days and improving the transplantation rate of fresh cycles.
In this study, both cohorts showed fairly good pregnancy outcomes, and it was assumed that this may be related to the advantages of D5 single blastocyst transfer and early follicular phase prolonged protocol. Many studies have shown that blastocysts have better developmental potential than cleavage embryos and can significantly increase the implantation, clinical pregnancy, and live birth rate.17–23 Gonadotropin-releasing hormone agonists can improve clinical pregnancy rates by harvesting high-quality oocytes and increasing endometrial tolerance.19,24,25 The group with slightly elevated progesterone levels still had significantly lower clinical pregnancy and live birth rates than those with normal progesterone levels (64.1% vs 75.5%, 63.5% vs 72.7%, respectively; all p < 0.05). Elevated progesterone levels may affect assisted reproductive technology (ART) outcomes in several ways. Huang et al found that elevated progesterone levels on HCG trigger days had a significant negative effect on the rate of high-quality embryos (p < 0.05).26 However, some studies have taken the opposite approach. Based on various markers of oocyte and embryo quality, the data strongly support that premature progesterone elevation does not negatively influence oocyte and embryo quality.2,26,27 Therefore, this conclusion is yet to be confirmed in a large prospective study. In this study, there was no significant difference in embryo quality between the two populations, and both populations were dominated by high-quality blastocysts.
Elevated progesterone levels may affect endometrial tolerance. By examining the transcriptome profile of the peri-implantation window endometrium, Liu et al found that with high progesterone levels on HCG trigger day, the expression profile of genes in the endometrium, related to the natural killer cell-mediated cytotoxic pathway, was significantly different from the normal levels in the endometrium.28
It has been suggested that a good ovarian response might moderate the negative influence of high progesterone levels on the probability of pregnancy.29,30 A meta-analysis showed that for high responders, such an effect was exhibited only when the level of progesterone on HCG trigger day reached 1.9–3.0ng/mL.2 Furthermore, this study suggested that in the normo-response patients and in poor responders, a detrimental effect of PE is present for progesterone levels of 0.8 to 1.1ng/mL, which was consistent with this study. The present study analyzed the data including maternal age (30.78 ± 3.76, 30.94 ± 3.87), AMH (4.21 ± 2.92, 4.01 ± 2.85), AFC (15.42 ± 5.57, 14.47 ± 5.13), Basal FSH (6.44 ± 1.85, 6.55 ± 1.82), and number of oocytes retrieved (12.41 ± 4.26, 13.78 ± 4.36), suggesting that the vast majority of women in both cohorts could be classified as normo-response patients. However, a slight increase in progesterone (P > 1.0ng/mL) on the day of HCG trigger still had a negative impact on pregnancy outcome. This result suggests that an increased oocyte yield might compensate for the detrimental effect of progesterone on the endometrium.
Some studies have proposed that one strategy to eliminate the adverse effect of high progesterone levels on pregnancy outcomes is to transfer blastocysts, considering that the evidence suggests that high progesterone does not decrease pregnancy rates in day 5 single blastocyst transfer cycles. It was assumed that the endometrium had already significantly recovered from the impairment caused by supraphysiological steroid concentrations on the fifth luteal day.3 However, the reliability of these results has not been confirmed, and some researchers have found that high progesterone levels can impair IVF outcomes, even in blastocyst transfers.26,29,31,32 Another large meta-analysis did not detect a significant moderating effect of the developmental stage of the embryo at transfer (cleavage versus blastocyst stage) on the association between progesterone elevation and probability of pregnancy achievement.2 In this study, D5 single blastocyst transfer was used in all these women; yet, the high progesterone group (P > 1.0ng/mL) still had lower clinical pregnancy and live birth rates. The results of this study suggest that on the fifth luteal day, the endometrium has not recovered from the effects of high progesterone, and its impact on pregnancy outcome still persists.
An important strength of the present study was that it is the first study to have compared the ART outcomes between women with P < 1.0ng/mL and those with 1.0 < P < 1.5ng/mL under an early follicular phase prolonged protocol. In addition, both groups used the same COS protocol, and all underwent D5 single blastocyst transfer, avoiding the influence of relevant confounding factors. In addition to comparing implantation and early pregnancy rates, an extended comparison of the differences in live birth rates between the two groups was also performed. Another significant factor to consider when assessing any study on the progesterone level is the accuracy and precision of the assay.20 Internal and external quality control of the assays utilized in our laboratory ensured that these standards were maintained. However, this study has some limitations. The limitations of this study include its retrospective design and small sample size.
Conclusion
This study suggests that a slightly elevated progesterone level on HCG trigger day may have a negative effect on the clinical outcomes of SBT cycles under an early follicular phase-prolonged protocol.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was reviewed and approved by the Institutional Review Board and Ethics Committee of Henan Provincial People’s Hospital, China (approval number: SYSZ-LL-2021091501). Patient consent to review their medical records was waived by the Institutional Review Board and the Ethics Committee of Henan Provincial People’s Hospital, owing to the retrospective nature of this study. We pledge to respect the privacy of all participants, and all data involved in this study were anonymous and kept confidential. This study was conducted in accordance with the Declaration of Helsinki, as revised in 1983.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, or interpretation, or in all these areas. They took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Henan Provincial Medical Science and Technology Tackling Program Provincial–Ministerial Co-construction Project (SBGJ202001002).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yang S, Pang T, Li R, et al. The individualized choice of embryo transfer timing for patients with elevated serum progesterone level on the HCG day in IVF/ICSI cycles: a prospective randomized clinical study. Gynecol Endocrinol. 2015;31(5):355–358. doi:10.3109/09513590.2014.995620
2. Venetis CA, Kolibianakis EM, Bosdou JK, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: a systematic review and meta-analysis of over 60 000 cycles. Hum Reprod Update. 2013;19(5):433–457. doi:10.1093/humupd/dmt014
3. Papanikolaou EG, Kolibianakis EM, Pozzobon C, et al. Progesterone rise on the day of human chorionic gonadotropin administration impairs pregnancy outcome in day 3 single-embryo transfer, while has no effect on day 5 single blastocyst transfer. Fertil Steril. 2009;91(3):949–952. doi:10.1016/j.fertnstert.2006.12.064
4. Lawrenz B, Long J, Stoop D, Missou I, Fatemi H. Impact of stimulation duration and gonadotropin type on the incidence of premature progesterone elevation - a retrospective analysis of the Ensure data. Gynecol Endocrinol. 2018;34(12):1044–1047. doi:10.1080/09513590.2018.1480710
5. Tsai YR, Lin YJ, Lin YC, Hsu TY, Lan KC. Factors associated with extremely high progesterone concentrations on the day of HCG administration. J Gynecol Obstet Hum Reprod. 2020;49(8):101720. doi:10.1016/j.jogoh.2020.101720
6. Connell MT, Patounakis G, Healy MW, et al. Is the effect of premature elevated progesterone augmented by human chorionic gonadotropin versus gonadotropin-releasing hormone agonist trigger? Fertil Steril. 2016;106(3):584–589.e1. doi:10.1016/j.fertnstert.2016.04.024
7. Lee CI, Chen HH, Huang CC, Lin PY, Lee TH, Lee MS. Early progesterone change associated with pregnancy outcome after fresh embryo transfer in assisted reproduction technology cycles with progesterone level of >1.5 ng/mL on human chorionic gonadotropin trigger day. Front Endocrinol (Lausanne). 2020;11:653. doi:10.3389/fendo.2020.00653
8. Robati S, Saab W, Durán-Retamal M, et al. The association between elevated progesterone level on day of hCG trigger and live birth rates in ART cycles: a single centre observational study. J Reprod Infertil. 2020;21(4):283–290. doi:10.18502/jri.v21i4.4333
9. Shufaro Y, Sapir O, Oron G, et al. Progesterone-to-follicle index is better correlated with in vitro fertilization cycle outcome than blood progesterone level. Fertil Steril. 2015;103(3):669–74.e3. doi:10.1016/j.fertnstert.2014.11.026
10. Eldstein MC, Seltman HJ, Cox BJ, et al. Progesterone level on the day of human chorionic gonadotropin administration in cycles with gonadotropin releasing hormone agonist suppression are not predictive of pregnancy outcome. Fertil Steril. 1990;54:853–857. doi:10.1016/S0015-0282(16)53945-4
11. Kably Ambe A, Medez Epinosa G, Barron vallejo J. A new parameter for the evaluation of premature luteinization: the preovulatory molecular relation between serum concentrations of progesterone and estradiol. Ginecol Obstet Mex. 1998;66:208–213.
12. Saleh HA, Omran MS, Draz M. Does subtle progesterone rise on the day of HCG affect pregnancy rate in long agonist ICSI cycles? J Assist Reprod Genet. 2009;26(5):239–242. doi:10.1007/s10815-009-9309-7
13. Tokgoz VY, Ekici GC, Tekin AB. The efficiency of progesterone/estradiol and progesterone/follicle ratio without elevated trigger-day progesterone levels on the reproductive outcomes of GnRH antagonist IVF/ICSI cycles. Gynecol Endocrinol. 2021;1:1–6. doi:10.1080/09513590.2021.1878137
14. Huang Y, Wang EY, Du QY, et al. Progesterone elevation on the day of human chorionic gonadotropin administration adversely affects the outcome of IVF with transferred embryos at different developmental stages. Reprod Biol Endocrinol. 2015;13:1–10. doi:10.1186/s12958-015-0075-3
15. Bosch E, Labarta E, Crespo J, et al. Circulating progesterone levels and ongoing pregnancy rates in controlled ovarian stimulation cycles for in vitro fertilization: analysis of over 4000 cycles. Hum Reprod. 2010;25(8):2092–2100. doi:10.1093/humrep/deq125
16. Wawrzkiewicz-Jałowiecka A, Lalik A, Soveral G. Recent update on the molecular mechanisms of gonadal steroids action in adipose tissue. Int J Mol Sci. 2021;22(10):5226. doi:10.3390/ijms22105226
17. Glujovsky D, Farquhar C, Quinteiro Retamar AM, et al. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology[CD]. Cochrane Database Syst Rev. 2016;(6):CD002118. doi:10.1002/14651858.CD002118.pub5
18. Kwek LK, Saffari SE, Tan HH, et al. Comparison between single and double cleavage-stage embryo transfers, single and double blastocyst transfers in a South East Asian in vitro fertilisation centre. Ann Acad Med Singap. 2018;47(11):451–454. doi:10.47102/annals-acadmedsg.V47N11p451
19. Fernández-Shaw S, Cercas R, Braña C, Villas C, Pons I. Ongoing and cumulative pregnancy rate after cleavage-stage versus blastocyst-stage embryo transfer using vitrification for cryopreservation: impact of age on the results. J Assist Reprod Genet. 2015;32:177–184.
20. Li Y, Liu S, Lv Q. Single blastocyst stage versus single cleavage stage embryo transfer following fresh transfer: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2021;267:11–17. doi:10.1016/j.ejogrb.2021.10.004
21. Thomas MR, Sparks AE, Ryan GL, et al. Clinical predictors of human blastocyst formation and pregnancy after extended embryo culture and transfer. Fertil Steril. 2010;94(2):543–548. doi:10.1016/j.fertnstert.2009.03.051
22. Styer AK, Wright DL, Wolkovich AM, et al. Single blastocyst transfer decreases twin gestation without affecting pregnancy outcome. Fertil Steril. 2008;89(6):1702–1708. doi:10.1016/j.fertnstert.2007.05.036
23. Sundaram V, Ribeiro S, Noel M. Multi-chorionic pregnancies following single embryo transfer at the blastocyst stage: a case series and review of the literature. J Assist Reprod Genet. 2018;35(12):2109–2117. doi:10.1007/s10815-018-1329-8
24. Ren J, Sha A, Han D, et al. Does prolonged pituitary downregulation with gonadotropin-releasing hormone agonist improve the live-birth rate in in vitro fertilization treatment? Fertil Steril. 2014;102(1):75–81. doi:10.1016/j.fertnstert.2014.03.030
25. Kang J, Park J, Chung D, et al. Comparison of the clinical outcome of frozen-thawed embryo transfer with and without pretreatment with a gonadotropin-releasing hormone agonist. Obstet Gynecol Sci. 2018;61(4):489–496. doi:10.5468/ogs.2018.61.4.489
26. Huang B, Ren X, Wu L, et al. Elevated progesterone levels on the day of oocyte maturation may affect top quality embryo IVF cycles. PLoS One. 2016;11(1):e0145895. doi:10.1371/journal.pone.0145895
27. Adda-Herzog E, Poulain M, de Ziegler D, Ayoubi JM, Fanchin R. Premature progesterone elevation in controlled ovarian stimulation: to make a long story short. Fertil Steril. 2018;109(4):563–570. doi:10.1016/j.fertnstert.2018.02.132
28. Liu L, Zhao L, Li TC, et al. Comparison of progesterone measurement on day of, and day after, HCG administration in IVF-embryo transfer cycles. Reprod Biomed Online. 2015;30(2):157–165. doi:10.1016/j.rbmo.2014.10.017
29. Fanchin R, Hourvitz A, Olivennes F, Taieb J, Hazout A, Frydman R. Premature progesterone elevation spares blastulation but not pregnancy rates in in vitro fertilization with coculture. Fertil Steril. 1997;68(4):648–652. doi:10.1016/S0015-0282(97)80464-5
30. Xu B, Li Z, Zhang H, et al. Serum progesterone level effects on the outcome of in vitro fertilization in patients with different ovarian response: an analysis of more than 10,000 cycles. Fertil Steril. 2012;97(6):1321–7.e1–4. doi:10.1016/j.fertnstert.2012.03.014
31. Corti L, Papaleo E, Pagliardini L, et al. Fresh blastocyst transfer as a clinical approach to overcome the detrimental effect of progesterone elevation at hCG triggering: a strategy in the context of the Italian law. Eur J Obstet Gynecol Reprod Biol. 2013;171(1):73–77. doi:10.1016/j.ejogrb.2013.08.017
32. Ochsenkuhn R, Arzberger A, von Schonfeldt V, et al. Subtle progesterone rise on the day of human chorionic gonadotropin administration is associated with lower live birth rates in women undergoing assisted reproductive technology: a retrospective study with 2555 fresh embryo transfers. Fertil Steril. 2012;98(2):347–354. doi:10.1016/j.fertnstert.2012.04.041
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
