Back to Journals » Neuropsychiatric Disease and Treatment » Volume 13
Sleep apnea and the subsequent risk of Parkinson’s disease: a 3-year nationwide population-based study
Authors Chou PS, Lai CL, Chou YH, Chang WP
Received 9 February 2017
Accepted for publication 10 March 2017
Published 30 March 2017 Volume 2017:13 Pages 959—965
DOI https://doi.org/10.2147/NDT.S134311
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Wai Kwong Tang
Ping-Song Chou,1 Chiou-Lian Lai,1–3 Yii-Her Chou,4,5,* Wei-Pin Chang6,*
1Department of Neurology, Kaohsiung Medical University Hospital, 2Department of Neurology, Faculty of Medicine, College of Medicine, 3Department of Neurology, Kaohsiung Municipal Hsiao-Kang Hospital, 4Department of Urology, Faculty of Medicine, College of Medicine, 5Department of Urology, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, 6School of Health Care Administration, Taipei Medical University, Taipei City, Taiwan
*These authors contributed equally to this work
Purpose: Sleep apnea (SA)-induced chronic intermittent hypoxia increases oxidative stress and inflammation, which may contribute to the pathophysiology of Parkinson’s disease (PD). This study evaluated the risk of PD following SA diagnosis.
Patients and methods: This was a 3-year nationwide population-based matched cohort study using claims data from the National Health Insurance Research Database (NHIRD), Taiwan. We analyzed 1,944 patients diagnosed as having SA between 1997 and 2005 and a matched cohort of 9,720 non-SA patients from the NHIRD. Patients with a history of PD were excluded. Each patient was followed up for 3 years to evaluate subsequent PD development.
Results: Of the 11,664 patients, 17 (0.9%) and 38 (0.4%) from the SA and matched non-SA cohorts, respectively, were subsequently diagnosed as having PD during follow-up. After adjustments for potential confounders, the SA cohort had a 1.85-fold higher risk of PD than the non-SA cohort (95% confidence interval [CI] =1.02–3.35; P=0.042). After age and sex stratification, PD development was independently associated with SA only in men (adjusted hazard ratio [HR], 2.26; 95% CI =1.11–4.63; P<0.05) and in patients aged ≥60 years (adjusted HR, 1.93; 95% CI =1.01–3.71; P<0.05).
Conclusion: Our study suggests that patients with SA are at an increased longitudinal risk of PD. Furthermore, age and male sex are independently associated with the risk of PD.
Keywords: cohort study, intermittent hypoxia, National Health Insurance Research Database, population-based study
A Letter to the Editor has been received and published for this article.
Introduction
Parkinson’s disease (PD) is characterized by bradykinesia, tremors, rigidity, and postural instability. A meta-analysis of global data demonstrated an increasing prevalence of PD with age,1 and a higher prevalence of PD was observed in the Chinese male population.2 In addition to age and sex, other potential risk factors for PD, including a family history of PD,3 depression,4 constipation,5 and sleep disorders requiring zolpidem,6 have been reported in epidemiological studies.
The prevalence of sleep disorders in PD is 40%–90%.7 Sleep disorders negatively affect cognitive functions and quality of life in patients with PD. Insomnia, daytime sleepiness with sleep attacks, restless legs syndrome, and rapid eye movement sleep behavior disorder are the most frequent sleep disorders associated with PD.8 Furthermore, snoring was observed in up to 70% of patients with PD,9 and 14.5%–60% of patients with PD were estimated to have an apnea–hypopnea index of >15.10 Therefore, a close association between sleep-disordered breathing and PD can be considered.
Sleep apnea (SA), one of the most common forms of sleep-disordered breathing, is characterized by repeated periods of hypoxia and reoxygenation during sleep. SA may be mild, moderate, or severe, based on the number of apneas and hypopneas occurring per hour.11 The clinical significance of SA in PD has been discussed but remains controversial.12,13 SA-induced chronic intermittent hypoxia increases oxidative stress and inflammation,14 which are involved in PD pathophysiology.15 Experimental data have demonstrated the role of oxidative stress in α-synuclein aggregation and dopaminergic cell death.16 Therefore, SA-induced oxidative stress and inflammation may increase the risk of PD.
The present study investigated the hypothesis that patients with SA are at an increased risk of PD. A nationwide, population-based study was conducted to assess the relationship between SA and subsequent diagnosis of PD within a 3-year follow-up period. In addition, we attempted to determine whether SA is an age- and sex-dependent risk factor for PD.
Materials and methods
Data source
This retrospective cohort study was conducted using claims data from the National Health Insurance Research Database (NHIRD), Taiwan. The National Health Insurance (NHI) program, which was implemented on March 1, 1995, has reimbursed the health care costs of 99.9% of Taiwan’s population as of 2014. The NHI program provides comprehensive health care information, including demographic data of the insured, clinical visit dates, diagnostic codes, and prescription details. Under the NHI program, the National Health Research Institutes (NHRI) established the NHIRD, subsequently managing and auditing it. Several studies using NHIRD data have been published in peer-reviewed journals.
In the present study, data were obtained from the Longitudinal Health Insurance Database (LHID) 2005, a subset of the NHIRD. The LHID 2005 dataset contains historical ambulatory data and inpatient care data for 1 million randomly sampled beneficiaries who enrolled in the NHI program in 2005. Currently, the LHID 2005 allows researchers to explore the medical service utilization data of these 1 million patients during 1996–2012. The NHRI claims that there are no statistically significant differences in the data on age, sex, geographic region, and health care costs from the LHID 2005 and all claims data.
This study was approved by the Institutional Review Board of Kaohsiung Medical University Hospital, Taiwan (KMUHIRB-EXEMPT[II]-20160001). All personal information was eliminated from the secondary database prior to analyses. Therefore, the review board waived the requirement of obtaining written informed consent from the study patients.
Participants
We retrospectively examined the SA and matched non-SA cohorts to investigate the relationship between SA and the risk of PD. The SA cohort included patients aged ≥40 years and diagnosed as having SA (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 780.51, 780.53, 780.57, and 327.23) between January 1, 1997, and December 31, 2005, during inpatient or outpatient care. Patients with a history of SA before January 1, 1997, were excluded from the present study. SA diagnosis was defined according to validated definitions from previous studies.17,18 The date of initial SA diagnosis for each study patient was considered the index date.
The matched non-SA cohort comprised five non-SA patients who were matched to each patient with SA based on age, sex, and index year, and randomly selected from the remaining population in the same database. Patients who were diagnosed as having SA during follow-up were excluded from the present study. Furthermore, patients with a history of PD (ICD-9-CM 332) before enrollment were excluded from the SA and non-SA cohorts. The study patients were individually followed for 3 years from their index date to evaluate PD development.
We identified several comorbidities before the index date as potential confounding factors for PD, including hypertension (ICD-9-CM 401–405), diabetes mellitus (ICD-9-CM 250), hyperlipidemia (ICD-9-CM 272), concussion and head trauma (ICD-9-CM 310.2, 852, and 853), COPD (ICD-9-CM 496), and asthma (ICD-9-CM 493).
Main outcome measures
The outcome of interest was defined as receiving a diagnosis of PD after the index date. PD diagnosis was defined as receiving any outpatient or inpatient care for PD (ICD-9-CM 332). A validation study reported that this definition had favorable diagnostic accuracy.19 To avoid the misdiagnosis of secondary parkinsonism as idiopathic PD, patients diagnosed as having carbon monoxide intoxication (ICD-9-CM 986), major psychiatric diseases (ICD-9-CM 291, 292, 293.0, 293.1, 293.81, 293.82, and 295–299), and dementia (ICD-9-CM 290.11, 290.12, 290.20, 290.3, 290.41, 290.42, 290.8, 290.9, 294.11, and 294.21) before the index date and during follow-up were excluded from the present study.
Statistical analyses
A Pearson chi-squared test was performed to evaluate the differences in the categorical variables, including urbanization level, monthly income, geographic region, and comorbidities, of the SA and non-SA cohorts. A Kaplan–Meier survival test was performed to estimate PD-free survival rates in the SA and non-SA cohorts, and a log-rank test was used to analyze the differences between the survival curves. Cox proportional hazards regression analysis was conducted to examine the crude and adjusted hazard ratios (HRs) for PD in the SA cohort, compared to the non-SA cohort during the 3-year follow-up period, after adjustments for sex, age, urbanization level, geographic region, monthly income, hypertension, hyperlipidemia, diabetes mellitus, asthma, COPD, and head injury. Furthermore, an age- and sex-stratified analysis using the Cox proportional hazards regression model was conducted to evaluate the risk of PD in the SA cohort across different age groups and sex. A two-sided P<0.05 was considered statistically significant.
Results
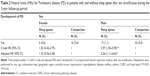
A total of 1,944 and 9,720 patients were included in the SA and non-SA cohorts, respectively. Of the 11,664 patients, 42.6%, 30.2%, and 27.1% belonged to the 40–49, 50–59, and ≥60 years of age groups, respectively; 63.1% of all patients were men. After adjustments for sex, age, and index year, the SA cohort was more likely to reside in urbanized communities and had a higher monthly income than the non-SA cohort. In addition, the SA cohort tended to have more comorbidities, such as hypertension, hyperlipidemia, diabetes mellitus, asthma, COPD, and head injury, than the non-SA cohort. Table 1 presents the demographic data and comorbidities of the SA and non-SA cohorts.
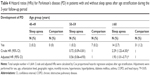
Of the 11,664 patients, 55 (0.5%) patients received a diagnosis of PD during the 3-year follow-up period; 17 (0.9%) and 38 (0.4%) patients in the SA and non-SA cohorts, respectively, developed PD (Table 2). Cox proportional hazards regression analysis demonstrated that the crude HR for PD was 2.25 times higher (95% confidence interval [CI] =1.27–3.98; P<0.01) in the SA cohort than in the non-SA cohort. The risk of PD remained significant after adjustments for potential confounders, including sex, age, urbanization level, geographic region, monthly income, hypertension, hyperlipidemia, diabetes mellitus, asthma, COPD, and head injury (adjusted HR, 1.85; 95% CI =1.02–3.35; P=0.042). Kaplan–Meier analysis demonstrated that the SA cohort had a significantly lower 3-year PD-free survival rate than the non-SA cohort (log-rank P<0.01; Figure 1).
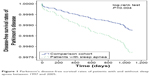  | Figure 1 Parkinson’s disease-free survival rates of patients with and without sleep apnea between 1997 and 2005. |
Table 3 presents the risk for PD between SA and non-SA cohorts after sex stratification. Men with SA had a significantly higher risk of PD than those without SA before (HR, 2.97; 95% CI =1.50–5.90; P<0.01) and after (adjusted HR, 2.26; 95% CI =1.11–4.63; P<0.05) adjustments for potential confounders. In contrast, women did not exhibit a significantly increased risk of PD in the SA cohort compared to those in the non-SA cohort during the 3-year follow-up period (adjusted HR, 1.10, 95% CI =0.36–3.40).
In addition, age stratification demonstrated that only elderly patients (age ≥60 years) in the SA cohort had a significantly higher risk of PD than those in the non-SA cohort before (HR, 2.29; 95% CI =1.22–4.30; P<0.05) and after (adjusted HR, 1.93; 95% CI =1.01–3.71; P<0.05) adjustments for potential confounders (Table 4).
Discussion
Our study demonstrated an association between SA and the risk of PD using NHIRD data during a 3-year follow-up period. The main study finding was that after adjustments for possible confounders, the SA cohort had a 1.85-fold higher risk of PD than the non-SA cohort. Separate analyses revealed that SA is an age- and sex-dependent risk factor for PD. Men and elderly patients (age ≥60 years) were at a particularly high risk of PD. This finding is in accordance with our hypothesis that patients with SA are at an increased longitudinal risk of PD.
Whether SA is an independent risk factor for PD or merely an early symptom during the prodromal phase of PD remains unclear. The cohort design of this study enabled the identification of a temporal association between SA and PD. To clearly demonstrate the temporal association between SA and PD, patients with a history of PD before the index date were excluded from this study. We observed that the SA cohort had an increased risk of PD, indicating that SA may be an independent risk factor for PD.
The pathophysiological mechanisms underlying the association between SA and the risk of PD remain unclear; however, several theories can be discussed. First, SA-induced chronic intermittent hypoxia can activate inflammatory pathways, leading to increased levels of systemic inflammatory markers.20–22 The brains of patients with PD exhibited signs of neuroinflammatory reactions, contributing to a cascade of events and subsequent neuron death.23 Furthermore, increased oxidative stress was previously reported in patients with SA.24 A postmortem study indicated that oxidative stress plays an important role in the pathological processes underlying PD development.25 Therefore, increased oxidative stress and inflammation due to SA may directly contribute to an increased risk of PD.
In this study, men and elderly patients (age ≥60 years) with SA were at a significantly increased risk of PD. The prevalence of severe SA is higher in adult men than in adult women.26 In another study, male sex and age were also independent risk factors for severe SA in the elderly group.27 Moreover, a strong correlation has been reported between SA severity and biomarkers of systemic inflammation and oxidative stress.28,29 Therefore, it is reasonable to conclude that men and elderly patients have an increased risk of PD, assuming inflammation and oxidative stress play key roles in PD pathophysiology.
Furthermore, findings from brain imaging studies in patients with SA have demonstrated that SA is associated with the risk of PD. Diffusion tensor imaging studies in patients with SA revealed decreased mean diffusivity in the basal ganglia.30 Magnetic resonance spectroscopy demonstrated that hypoxia-related metabolites and microstructural changes in the putamen are more pronounced with increasing SA severity.31 Furthermore, decreased cerebral blood flow was reported in the right red nucleus and right midbrain of patients with SA.32 These abnormal findings in the basal ganglia and midbrain of patients with SA may indicate an association between SA and the risk of PD.
Several studies have reported that SA is associated with subsequent PD.33–35 However, the present study findings were different and had stronger implications than those of previous studies. First, we used validated definitions of SA and PD17–19 to maximize case ascertainment. Second, we excluded patients with several conditions that may contribute to secondary parkinsonism, such as carbon monoxide intoxication and neuropsychiatric diseases with psychotic features, to appropriately identify patients with idiopathic PD. Third, we identified and adjusted for common confounding comorbidities, including hypertension, hyperlipidemia, diabetes mellitus, asthma, COPD, and head injury, which may affect the subsequent risk of PD, to minimize their influence on PD development.
Nevertheless, the present study had some limitations. First, the diagnoses of SA and PD were completely based on the diagnostic codes recorded by physicians in the database, but information regarding these specialists was unavailable. In addition, we were unable to distinguish between primary and secondary parkinsonism. To maximize case ascertainment, we adopted validated definitions of SA and PD from previous studies.17–19 Furthermore, we excluded patients who were at a possible risk of secondary parkinsonism, including those who had been diagnosed with carbon monoxide intoxication, major psychiatric diseases, and dementia, before the index date and during follow-up to improve the diagnostic accuracy. Second, the NHIRD does not record data on the apnea–hypopnea index values, respiratory parameters, and treatment status of patients with SA. Therefore, the duration, severity, and treatment status of SA could not be determined. Third, individual patient information, including family history, environmental factors, toxin exposure, and lifestyle factors, were not available from the NHIRD. Fourth, because of the relatively short follow-up period of 3 years, it was difficult to determine whether SA occurred during the prodromal phase of PD before the onset of motor symptoms. Previous studies with longer follow-up periods have supported our findings, despite using different inclusion and exclusion criteria.33–35 Fifth, the actual number of patients with SA who developed PD was small, particularly in women and young patients, thus limiting the statistical power in subgroup analysis based on age and sex. Sixth, we did not stratify SA into obstructive or central types. We assumed that most patients had obstructive SA based on the literature about patients with polysomnography-confirmed SA in Taiwan, which states that only 0.8% of patients have pure central SA.18,36 Further investigation is required to elucidate whether obstructive and central SA differ in the risk of PD.
Finally, despite the temporal relationship between SA and PD, the underlying causal mechanism was not definitively confirmed in this retrospective study. PD may remain asymptomatic for many years, and SA may be regarded as an initial premotor symptom of PD. Therefore, based on our study results, we cannot obviate the possibility that SA may be an early symptom of PD. Moreover, future studies considering these indices must evaluate the association between SA and the risk of PD and investigate the longitudinal effect of treatment on continuous positive airway pressure.
Conclusion
The present study demonstrated a possible relationship between SA and the risk of PD. The SA cohort had a higher longitudinal risk of PD than the non-SA cohort, particularly elderly people and men. Further prospective studies are warranted to evaluate the causality and underlying mechanisms of the association between SA and the risk of PD.
Acknowledgment
This study was supported by grants from the Taipei Medical University (TMU105-AE1-B05 and 106-CGH-TMU-02).
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord. 2014;29(13):1583–1590. | ||
Ma CL, Su L, Xie JJ, Long JX, Wu P, Gu L. The prevalence and incidence of Parkinson’s disease in China: a systematic review and meta-analysis. J Neural Transm (Vienna). 2014;121(2):123–134. | ||
Noyce AJ, Bestwick JP, Silveira-Moriyama L, et al. Meta-analysis of early nonmotor features and risk factors for Parkinson disease. Ann Neurol. 2012;72(6):893–901. | ||
Shen CC, Tsai SJ, Perng CL, Kuo BI, Yang AC. Risk of Parkinson disease after depression: a nationwide population-based study. Neurology. 2013;81(17):1538–1544. | ||
Lin CH, Lin JW, Liu YC, Chang CH, Wu RM. Risk of Parkinson’s disease following severe constipation: a nationwide population-based cohort study. Parkinsonism Relat Disord. 2014;20(12):1371–1375. | ||
Yang YW, Hsieh TF, Yu CH, Huang YS, Lee CC, Tsai TH. Zolpidem and the risk of Parkinson’s disease: a nationwide population-based study. J Psychiatr Res. 2014;58:84–88. | ||
Suzuki K, Miyamoto M, Miyamoto T, Iwanami M, Hirata K. Sleep disturbances associated with Parkinson’s disease. Parkinsons Dis. 2011;2011:219056. | ||
Schrempf W, Brandt MD, Storch A, Reichmann H. Sleep disorders in Parkinson’s disease. J Parkinsons Dis. 2014;4(2):211–221. | ||
Braga-Neto P, da Silva-Júnior FP, Sueli Monte F, de Bruin PF, de Bruin VM. Snoring and excessive daytime sleepiness in Parkinson’s disease. J Neurol Sci. 2004;217(1):41–45. | ||
da Silva-Júnior FP Jr, do Prado GF, Barbosa ER, Tufik S, Togeiro SM. Sleep disordered breathing in Parkinson’s disease: a critical appraisal. Sleep Med Rev. 2014;18(2):173–178. | ||
Mannarino MR, Di Filippo F, Pirro M. Obstructive sleep apnea syndrome. Eur J Intern Med. 2012;23(7):586–593. | ||
Maria B, Sophia S, Michalis M, et al. Sleep breathing disorders in patients with idiopathic Parkinson’s disease. Respir Med. 2003;97(10):1151–1157. | ||
Cochen De Cock V, Abouda M, Leu S, et al. Is obstructive sleep apnea a problem in Parkinson’s disease? Sleep Med. 2010;11(3):247–252. | ||
Lurie A. Inflammation, oxidative stress, and procoagulant and thrombotic activity in adults with obstructive sleep apnea. Adv Cardiol. 2011;46:43–66. | ||
Taylor JM, Main BS, Crack PJ. Neuroinflammation and oxidative stress: co-conspirators in the pathology of Parkinson’s disease. Neurochem Int. 2013;62(5):803–819. | ||
Xiang W, Schlachetzki JC, Helling S, et al. Oxidative stress-induced posttranslational modifications of alpha-synuclein: specific modification of alpha-synuclein by 4-hydroxy-2-nonenal increases dopaminergic toxicity. Mol Cell Neurosci. 2013;54:71–83. | ||
Lee YC, Hung SY, Wang HK, et al. Sleep apnea and the risk of chronic kidney disease: a nationwide population-based cohort study. Sleep. 2015;38(2):213–221. | ||
Su VY, Liu CJ, Wang HK, et al. Sleep apnea and risk of pneumonia: a nationwide population-based study. CMAJ. 2014;186(6):415–421. | ||
Lee YC, Lin CH, Wu RM, et al. Discontinuation of statin therapy associates with Parkinson disease: a population-based study. Neurology. 2013;81(5):410–416. | ||
Nadeem R, Molnar J, Madbouly EM, et al. Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med. 2013;9(10):1003–1012. | ||
Priou P, Gagnadoux F, Tesse A, et al. Endothelial dysfunction and circulating microparticles from patients with obstructive sleep apnea. Am J Pathol. 2010;177(2):974–983. | ||
McNicholas WT. Obstructive sleep apnea and inflammation. Prog Cardiovasc Dis. 2009;51(5):392–399. | ||
Hunot S, Hirsch EC. Neuroinflammatory processes in Parkinson’s disease. Ann Neurol. 2003;53(Suppl 3):S49–S58; discussion S58–S60. | ||
Ntalapascha M, Makris D, Kyparos A, et al. Oxidative stress in patients with obstructive sleep apnea syndrome. Sleep Breath. 2013;17(2):549–555. | ||
Jenner P, Dexter DT, Sian J, Schapira AH, Marsden CD. Oxidative stress as a cause of nigral cell death in Parkinson’s disease and incidental Lewy body disease. The Royal Kings and Queens Parkinson’s Disease Research Group. Ann Neurol. 1992;32(Suppl):S82–S87. | ||
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. | ||
Hongyo K, Ito N, Yamamoto K, et al. Factors associated with the severity of obstructive sleep apnea in older adults. Geriatr Gerontol Int. Epub 2016 June 1. | ||
Oyama J, Nagatomo D, Yoshioka G, et al. The relationship between neutrophil to lymphocyte ratio, endothelial function, and severity in patients with obstructive sleep apnea. J Cardiol. 2016;67(3):295–302. | ||
Guo Q, Wang Y, Li QY, Li M, Wan HY. Levels of thioredoxin are related to the severity of obstructive sleep apnea: based on oxidative stress concept. Sleep Breath. 2013;17(1):311–316. | ||
Kumar R, Chavez AS, Macey PM, Woo MA, Yan-Go FL, Harper RM. Altered global and regional brain mean diffusivity in patients with obstructive sleep apnea. J Neurosci Res. 2012;90(10):2043–2052. | ||
Alkan A, Sharifov R, Akkoyunlu ME, et al. MR spectroscopy features of brain in patients with mild and severe obstructive sleep apnea syndrome. Clin Imaging. 2013;37(6):989–992. | ||
Yadav SK, Kumar R, Macey PM, et al. Regional cerebral blood flow alterations in obstructive sleep apnea. Neurosci Lett. 2013;555:159–164. | ||
Sheu JJ, Lee HC, Lin HC, Kao LT, Chung SD. A 5-year follow-up study on the relationship between obstructive sleep apnea and Parkinson disease. J Clin Sleep Med. 2015;11(12):1403–1408. | ||
Yeh NC, Tien KJ, Yang CM, Wang JJ, Weng SF. Increased risk of Parkinson’s disease in patients with obstructive sleep apnea: a population-based, propensity score-matched, longitudinal follow-up study. Medicine (Baltimore). 2016;95(2):e2293. | ||
Chen JC, Tsai TY, Li CY, Hwang JH. Obstructive sleep apnea and risk of Parkinson’s disease: a population-based cohort study. J Sleep Res. 2015;24(4):432–437. | ||
Shiao TH, Liu CJ, Luo JC, et al. Sleep apnea and risk of peptic ulcer bleeding: a nationwide population-based study. Am J Med. 2013;126(3):249–255, 255.e1. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.