Back to Journals » Clinical Ophthalmology » Volume 10
Single flash electroretinograms of mature cataractous and fellow eyes
Authors Yamauchi Y, Mochizuki J, Hirakata A, Uda S
Received 2 August 2016
Accepted for publication 3 September 2016
Published 17 October 2016 Volume 2016:10 Pages 2031—2034
DOI https://doi.org/10.2147/OPTH.S118677
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yasuyuki Yamauchi,1 Jun-ichi Mochizuki,1 Akito Hirakata,2 Shigekazu Uda1
1Nihonmatsu Eye Hospital, Edogawa, Tokyo, Japan; 2Kyorin Eye Center, Kyorin University School of Medicine, Tokyo, Japan
Background: It is generally stated that opacities of the ocular media, including senile cataract, have little effect on the electrical responses of the retina. However, lower amplitudes and longer implicit times are sometimes observed in electroretinograms (ERGs) of patients with mature cataract.
Methods: Single flash ERGs of mature cataractous eyes with decimal visual acuity less than 0.1 were compared with those of the fellow eyes with decimal visual acuity better than 0.5, in 105 senile cataract patients.
Results: The mean amplitudes and implicit times of ERG a-waves were, respectively, 323.6±95.8 µV and 14.7±3.5 ms in the cataractous eyes and 352.3±96.6 µV and 12.0±1.5 ms in the fellow eyes. The mean amplitudes and implicit times of ERG b-waves were, respectively, 390.1±108.7 µV and 63.4±27.9 ms in the cataractous eyes and 415.3±119.1 µV and 59.0±9.3 ms in the fellow eyes. The mean amplitudes of the a- and b-waves were significantly lower and the mean implicit times of the a- and b-wave were significantly longer in the cataractous eyes as compared to those of the fellow eyes. Postoperative visual acuity was similar in cataractous and fellow eyes.
Conclusion: Even though single flash ERG was influenced due to mature cataract, eyes revealed good postoperative visual acuity. Single flash ERG does not always reflect the foveal function and the visual pathway; nevertheless, it remains a reliable guide to evaluate visual prognosis before cataract surgery.
Keywords: single flash ERG, mature cataract
Introduction
It is generally stated that opacities of the ocular media, including senile cataract, have little effect on the electrical responses of the retina.1,2 Single flash electroretinogram (ERG) has been widely used, as a commercially available technology, to examine retinal function prior to cataract surgery, especially when the opacity is so severe that visual acuity (VA) of the patient is extremely poor and fundus condition is not visible. In a previous study with 22 patients with mature cataract, it was observed that single flash ERG values decreased depending on the degree of cataract opacity, even though the difference was not significant3 and Uji showed that the amplitude of ERG b-wave was significantly increased after cataract surgery in comparison to the preoperative result.4 An et al showed that the amplitude of central point multifocal ERG was significantly lower in cataract patients compared with control group, from “hand movement” (HM) to 0.8 of preoperative VA.5 Furthermore, Miura et al reported that the presence of cataracts of Grade 2 or higher affect the amplitude and the implicit time of flicker ERGs.6 However, ERG information in patients with mature cataract is still limited. The goal of this study was to examine whether single flash ERG was different between cataractous and fellow eyes in patients with severe cataract.
Methods
Subjects
A total of 117 patients with a mature cataractous eye was included in this study.
The first group comprised 105 patients with a mature cataractous eye, aged 22–90 years (average age: 64.6±15.4). These patients underwent surgery in the period between September 2011 and November 2015, at Nihonmatsu Eye Hospital, Tokyo, Japan. The decimal VA of cataractous eyes was in the range from “light perception” (LP) to 0.1. The cataractous and fellow eyes did not have any ophthalmic diseases other than cataract. All fellow eyes had a VA higher than 0.5, with average of 0.86±0.27. All cataractous and fellow eyes received an examination that included slit lamp and indirect ophthalmoscope, before and after cataract surgery. However, fundus condition was invisible before surgery in mature cataractous eyes. Cataract surgeries were performed in cataractous eyes of 103 subjects by phacoemulsification with posterior chamber intraocular foldable hydrophobic acrylic lens implantation. Extracapsular cataract extraction and implantation of a sulcus-sutured polymethyl methacrylate lens were performed in 2 subjects. No operative complications were registered.
The second group, comprising 12 subjects aged 53–87 years (average age: 72.2±8.7) with mature cataract in both eyes and VA less than 0.1 who revealed good VA in both eyes after cataract surgery were used to investigate whether ERG differed between severe cataractous eyes. In this group, if the VA was equal, the eye showing less opacity in slit lamp examination was chosen as the fellow eye.
The experimental procedures were approved by the Medical Ethics Committee of the Nihonmatsu Eye Hospital, Tokyo, Japan. Informed consent was obtained from all participants. This research was conducted in accordance with the institutional guidelines and the tenets of the Declaration of Helsinki.
VA test
A Snellen chart was used to test the best-corrected VA of mature cataractous eyes and fellow eyes, whenever a cataract surgery was performed in the latter, before and after cataract surgery. The chart was viewed at a distance of 5 m, and VA was based on the smallest line that could be read. When patients could not see any of the characters for VA 0.1 at 5 m, VA was measured at 4 m, 3 m, 2 m, or 1 m and calculated by the formula:
VA =0.1× distance/5. | (1) |
When patients could not see the character at less than 1 m, VA was measured by the counting fingers, HM, or LP tests at a distance of 30 cm. In this study, for the statistical analysis, HM and counting fingers were considered as 0.005 and LP as 0.001. Statistical analysis of the VA was calculated after conversion to logarithm of the minimum angle of resolution units.
ERG recordings
The subjects’ pupils were maximally dilated with 0.5% tropicamide and 2.5% phenylephrine hydrochloride for all ERG recordings. ERG recording was not started until the pupils were dilated to, at least, 7 mm in diameter. After inducing anesthesia with 1 drop of 0.4% oxybuprocaine hydrochloride, the white light emitting diode electrode was placed on the cornea. A reference electrode was placed on the cheek, and a ground electrode was placed on the earlobe. ERG was recorded using white-flash stimulus (maximal combined response) after 10 minutes of dark adaptation. A commercial system (LE-4000, TOMEY corporation, Nagoya, Japan) was used to measure ERG with a 0.3 to 340 Hz band-pass filter, stimulation luminance set at 200 cd·s·m−2 (20,000 cd·m−2 ×10 ms). Recordings were not averaged.
Statistical analysis
Normality tests (Kolmogorov–Smirnov test and Shapiro–Wilk normality test) were conducted. If the data was not nonnormal (P≥0.05) in both normality tests, paired t-test was used. On the other hand, when the data was nonnormal (P<0.05) in a normality test, Wilcoxon’s signed rank test was used.
Paired t-test was used to compare amplitudes of ERGs in the first and second groups between cataractous and fellow eyes. Wilcoxon’s signed rank test was used to compare implicit times of ERGs in the first and second groups and VA in the first group, between cataractous and fellow eyes. The data are presented as the mean ± standard deviation. Significance was accepted for P<0.05. Data were statistically analyzed using Excel 2010 (paired t-test) and Eazy R software (Kolmogorov–Smirnov test, Shapiro–Wilk normality test and Wilcoxon’s signed rank test).
Results
First group
The mean VA of cataractous and fellow eyes was, respectively, 0.0067±0.02 and 0.86±0.27 before surgery and 1.0±0.23 and 1.0±0.20 after surgery (Table 1). VA before and after surgery was nonnormal in the normality tests. The difference was significant before surgery but not after surgery in the Wilcoxon’s signed rank test.
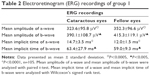
The mean amplitudes and implicit times of ERG a-waves were, respectively, 323.6±95.8 μV and 14.7±3.5 ms in the cataractous eyes and 352.3±96.6 μV and 12.0±1.5 ms in the fellow eyes. The mean amplitudes and implicit times of ERG b-waves were, respectively, 390.1±108.7 μV and 63.4±27.9 ms in the cataractous eyes and 415.3±119.1 μV and 59.0±9.3 ms in the fellow eyes. The amplitudes of a- and b-waves in the cataractous eyes and fellow eyes were not nonnormal in the normality tests. The implicit times of a- and b-waves in the cataractous eyes and fellow eyes were nonnormal in the normality tests. The mean amplitudes of the a- and b-waves were significantly reduced (paired t-test) and the mean implicit time of the a- and b-wave was significantly longer (Wilcoxon’s signed rank test) in the cataractous eyes in comparison with the fellow eyes (Table 2).
Of the 105 subjects, 15 subjects revealed negative pattern ERG (3 of them showed only in the cataractous eye) but no abnormalities, including chorioretinal atrophy with myopia, were found with indirect ophthalmoscopy. In addition, in 20 out of 105 subjects, the amplitude of both ERG a- and b-wave was higher in the mature cataractous eye than in the fellow eye. Of the 20 subjects, 2 subjects had supernormal (more than the mean +1.64* standard deviation of the fellow eyes of 105 subjects; 90% confidence interval) amplitude of ERG a-wave and 1 subject showed supernormal amplitude of ERG b-wave in mature cataractous eye. Four subjects revealed supernormal amplitude of ERG a-wave and 7 subjects had supernormal amplitude of ERG b-wave in the fellow eye of 105 subjects in the first group.
Second group
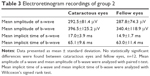
The mean amplitude and the mean implicit time of ERG a-waves were, respectively, 292.5±81.4 μV and 17.0±3.9 ms in cataractous eyes and 287.8±74.3 μV and 14.9±1.7 ms in fellow eyes. The mean amplitude and the mean implicit time of ERG b-waves were, respectively, 396.5±125.2 μV and 65.1±9.6 ms in cataractous eyes and 340.4±118.9 μV and 63.0±10.2 ms in fellow eyes (Table 3).
The amplitudes of a- and b-waves in the cataractous eyes and fellow eyes were not nonnormal in the normality tests. The implicit times of a- and b-waves in the cataractous eyes and fellow eyes were nonnormal in the normality tests.
No statistically significant differences were found between cataractous eyes and fellow eyes in the ERG.
Discussion
In this study, the mean amplitudes of ERG a- and b-waves were statistically lower in mature cataractous eyes than in fellow eyes, which may be due to the light-absorbing effect of the cataract. In fact, in group 2, in which the degree of opacity of cataract did not vary, ERG was not different between both mature cataractous eyes. However, in 20 out of 105 subjects, the amplitude of both ERG a- and b-wave was higher in mature cataractous eyes than in fellow eyes. Therefore, our data do not support that all mature cataractous eyes will show reduced values in ERGs. Of the 20 subjects, 2 subjects had supernormal amplitude of ERG a-wave and 1 subject showed supernormal amplitude of ERG b-wave in mature cataractous eyes. Even though, opacities of cataractous eyes in the slit lamp examination seemed to be severe enough to absorb the stimulation flash light. At the moment, we do not have enough evidence to speculate.
On the other hand, 4 subjects revealed supernormal amplitude of ERG a-wave and 7 subjects had supernormal amplitude of ERG b-wave in fellow eyes of 105 subjects in the first group.
ERG is affected by age. However, in this study, we compared cataractous eyes and fellow eyes in patients. Thus, we thought the influence due to age was limited.
The stimulus luminance in this study was 200 cd·s·m−2, 10 times greater than that recommended by the International Society for Clinical Electrophysiology of Vision.7 Thus, stimulus luminance was probably strong enough to record a single flash ERG of eyes with opacities of optic media.
In recent studies, Miura et al mentioned that the presence of cataracts should be taken into consideration when interpreting flicker ERGs,6 and An et al showed that the amplitude of central point multifocal ERG was significantly lower in cataract patients.5 However, Cruz and Adachi-Usami observed that, in a single flash ERG, the mean amplitudes of the a- and b-waves were slightly reduced in the mature cataractous eyes as compared to those of the fellow eyes, but the difference was not significant.3 In our study, the light-absorbing effect of the cataract, based on the amplitudes of a- and b-waves, was approximately 8% and 6%, respectively, instead of the 0.5 log unit observed by them. We followed a method of analysis similar to that used by Cruz and Adachi-Usami.3 Unfortunately, their study included only 22 subjects, while ours comprised 105. If they had more subjects in the analysis, a statistical difference between cataractous and fellow eyes might have been obtained.
Chorioretinal atrophy was the most common cause of subnormal ERGs. Postoperative VA was shown to be lower in cataractous eyes with subnormal ERGs than in eyes with normal ERGs.3 In our study, 15 out of 105 subjects with negative pattern ERG and good VA after cataract surgery did not show any obvious fundus abnormalities, including chorioretinal atrophy.
Algvere et al stated that preoperative flash ERG and visually evoked cortical potential are not able to safely predict the outcome of vitrectomy in diabetics with very low VA.8 According to our data, even if the retinal function is normal, a single flash ERG result can be decreased by opacity of the ocular media (mature cataract). Therefore, evaluation of visual function with flash ERG of a patient with plural media opacities (corneal opacities, cataract, vitreous hemorrhage, etc.) would be much more difficult.
Conclusion
In conclusion, severe cataract can reduce the amplitude and increase the implicit time of single flash ERG a- and b-waves, in eyes with good visual function.
Acknowledgments
We thank EDITAGE for the professional editing and colleagues of Nihonmatsu Eye Hospital for their efforts and time donated to the study.
Disclosure
The authors report no conflicts of interest in this work.
References
Burian HM, Burns CA. A note on senile cataracts and the electroretinogram. Doc Ophthalmol. 1966;20:141–149. | ||
van Lith GH. Application of electro-ophthalmology. In: Michaelson IC, editor. Textbook of the Fundus of the Eye. 3rd ed. Great Britain: Clark Constable Ltd; 1980:627–632. | ||
Cruz RD, Adachi-Usami E. Quantitative evaluation of electroretinogram before cataract surgery. Jpn J Ophthalmol. 1989;33(4):451–457. | ||
Uji Y. [The effects of absorption of visible light in the human lens on the electroretinography. 2. Comparison of the spectral ERGs recorded before and after cataract surgery (author’s transl)]. Nippon Ganka Gakkai Zasshi. 1977;81(9):1321–1327. Japanese. | ||
An J, Zhang L, Wang Y, Zhang Z. The success of cataract surgery and the preoperative measurement of retinal function by electrophysiological techniques. J Ophthalmol. 2015;2015:401281. Epub 2015 Oct 21. | ||
Miura G, Nakamura Y, Sato E, Yamamoto S. Effects of cataracts on flicker electroretinograms recorded with RETeval™ system: new mydriasis-free ERG device. BMC Ophthalmol. 2016;16:22. | ||
McCulloch DL, Marmor MF, Brigell MG, et al. ISCEV Standard for full-field clinical electroretinography (2015 update). Doc Ophthalmol. 2015;130(1):1–12. | ||
Algvere P, Persson HE, Wanger P. Preoperative electroretinograms and visual evoked cortical potentials for predicting outcome of vitrectomy in diabetics. Retina. 1985;5(3):179–183. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.