Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
Significance of Nuclear Factor-Kappa B (NF-κB) and Survivin in Breast Cancer and Their Association with Radiosensitivity and Prognosis
Authors Cao Q, Ai XQ, Mushajiang M
Received 2 December 2022
Accepted for publication 10 February 2023
Published 9 March 2023 Volume 2023:15 Pages 175—188
DOI https://doi.org/10.2147/BCTT.S399994
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Pranela Rameshwar
Qian Cao, Xiu-Qing Ai, Munire Mushajiang
Department of Breast Radiotherapy, The Third Affiliated Teaching Hospital of Xinjiang Medical University (Affiliated Cancer Hospital), Urumqi, Xinjiang, 830011, People’s Republic of China
Correspondence: Munire Mushajiang, Department of Breast Radiotherapy, The Third Affiliated Teaching Hospital of Xinjiang Medical University (Affiliated Cancer Hospital), No. 789, Suzhou East Street, Xinshi District, Urumqi, Xinjiang, 830011, People’s Republic of China, Tel +86 1389 9983 611, Fax +86 0991 7819 502, Email [email protected]
Purpose: Analyze the expression of NF-κB and survivin genes and mRNAs in breast cancer, and evaluate their impact on prognosis. Investigate their association with radiosensitivity in breast cancer.
Methods: The expression levels of NF-κB and survivin genes in breast cancer were analyzed by bioinformatics, NF-κB and survivin mRNA was verified by RTRCR, and their association with prognosis were assessed. Knockdown of survivin by siRNA was used to analyze its association with radiosensitivity in breast cancer.
Results: The gene expression of NFKB1 and BIRC5 are differentially expressed in a variety of tumours and their corresponding normal tissue species. In breast cancer tissues, NFKB1 expression levels were reduced compared to normal tissue, while BIRC5 expression levels were increased (P< 0.05). In different molecular subtypes of breast cancer, NFKB1 and BIRC5 were differentially expressed (P< 0.05), NFKB1 was highly expressed in the luminal subtype and BIRC5 was highly expressed in the TNBC subtype. In TNBC subtype, NFKB1 expression is higher in IM subtype than other subtypes (P< 0.05), and BIRC5 expression is higher in BL-2 than other subtypes (P< 0.05). NFKB1 was not associated with tumour size, lymph node stage and distant metastasis (P≥ 0.05), while BRIC5 was associated with these clinical features (P< 0.05). NF-κB and survivin genes were negatively correlated (R = - 0.193, P< 0.05). The mRNA levels of NF-κB and survivin are expressed in the same trend in breast cancer patients. NF-κB and survivin were not significantly different in recurrent and non-recurrent patients (P≥ 0.05). The mRNA levels of the both were not correlated with breast cancer subtypes (P≥ 0.05). The mRNA expression of NF-κB and survivin correlated with distant metastasis. NF-κB and survivin mRNAs were positively correlated (R=0.903, P< 0.05). Gene and mRNA expression of NF-κB and survivin were not associated with patients’ survival overall survival (OS) (P≥ 0.05). Down-regulation of survivin has little effect on the proliferation rate of breast cancer cells (P≥ 0.05), but increase the apoptosis rate of breast cancer cells (P< 0.05).The proliferation rate of cells decreased and the apoptosis rate increased significantly (P< 0.05) after the implementation of radiotherapy, and this technique could improve the radiosensitivity of breast cancer cells.
Conclusion: NF-κB and survivin interact at the gene and mRNA levels. Regulation of mRNA expression of NF-κB or survivin may help to improve the radiosensitivity of breast cancer cells, more experiments are needed to verify this in the future.
Keywords: breast cancer, nuclear factor-kappa B, survivin
Introduction
Breast cancer is one of the most prevalent cancers affecting women,1 and in terms of morbidity and mortality, is the most prevalent malignant tumor in women.2,3 Breast cancer interventions including surgery, chemoradiotherapy, endocrine therapy, and immunotherapy,4 which can benefit some patients, but in other cases, do not achieve the intended outcome due to the high heterogeneity of breast cancer.5–7 Consequently, understanding the molecules and signaling pathways related to breast cancer patient survival and enhancing treatment sensitivity are crucial tasks in contemporary biomedical research.
Several studies have identified nuclear factor-κB (NF-κB) as one of the molecules involved in the progression of breast cancer.8 NF-κB plays a crucial role in physiological and pathological processes, including cell proliferation, apoptosis, inflammatory response, immunological response, and tumor growth. Nuclear factor kappa B subunit 1 (NFKB1) is the gene encoding the P50 subunit of the NF-κB protein complex.9,10 Survivin is a member of the family of apoptotic proteins and regulates the physiological functions of cell mitosis, apoptosis, and cell cycle regulation, baculoviral IAP repeat- (BIRC5) is the gene encoding survivin.11 It has been demonstrated that tumor patients are more responsive to radiotherapy when survivin expression is inhibited;12 hence NF-κB and survivin has now become highly desirable target for anti-tumor therapy.13
The above studies suggest that NF-κB and survivin are associated with tumor growth and apoptosis, but the precise mechanistic activities and interactions between them are difficult to understand.14 The relationship between NF-κB and survivin has rarely been studied, and for physician reasons, our group analyzed the expression of NF-κB and survivin genes, mRNAs, and proteins in breast cancer and their clinical features, such as subtypes and tumor TNM stage to determine their impact on radiosensitivity and patient prognosis. Subsequently, we analyzed the relationship between NF-κB and survivin and downregulated survivin using siRNA to examine breast cancer radiosensitivity in order to develop a treatment for breast cancer patients.
Study Participants
The study protocol was approved by the Ethics Committee of The Affiliated Cancer Hospital of Xinjiang Medical University . Approval number is K-2021070. We selected 30 patients with breast cancer who presented to our hospital in December 2021 by the simple random sampling (SRS) method. Patients who refused to provide samples and those with unstable disease were excluded. We screened 26 female breast cancer patients who had relapsed. For this study. All patients were obtained informed consent before the experiment. We have summarized the clinical information of these patients at first diagnosis, included the patient age, TNM stage, maximum tumor diameter, number of axillary lymph node metastases, presence of distant metastases, expression levels of estrogen receptor (ER), progesterone receptor (PR) and expression of human epidermal growth factor receptor-2 (Her-2), and investigation of patient overall survival(OS). Blood from breast cancer patients was selected for measuring the mRNA expression levels of NF-κB and survivin. The human breast cancer cell line MDA-MB-231 was selected for the siRNA interference assay and was purchased from Procell Life Science & Technology (Wuhan, China) and correctly identified.
Methods
NF-κB and Survivin Gene Expression
In this study, we analyzed the data of NFKB1 and BIRC5 in normal tissues and tumor tissues from the TCGA database and an interactive web resource, the university of ALabama at Birmingham Cancer data analysis Portal (UALCAN)to assess the relationship between gene expression and molecular subtypes of tumors.15,16 The interrelationship between NFKB1 and BIRC5 genes was investigated by Pearson correlation analysis.17
NF-κB and Survivin mRNA Expression
We analyzed NF-κB and survivin mRNA expression in the blood of breast cancer patients by RT-PCR. RNA was extracted from each group of cells using a Trizol reagent. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as an internal parameter and the 2−ΔΔCt method was used to analyze the expression of relevant genes.18 The primer sequences used for gene testing are listed in Table 1. The relationship between NF-κB and survivin and the clinical characteristics of the patients was investigated by Chi-square test.19 The relationship between NF-κB and survivin mRNA expression levels was investigated by Spearman rank correlation analysis.17
 |
Table 1 The Primer Sequences |
Statistical Analysis
Gene analysis was performed using Wilcoxon rank test20 to assess the expression of NFKB1 and BIRC5 in breast cancer tissues and normal tissues, denoted by ns for P ≥ 0.05, * for P < 0.05, ** for P < 0.01 and *** for P < 0.001.In the TCGA database, we analyzed the relationship between NFKB1 and BIRC5 and indicators related to breast cancer prognosis.The indicators related to breast cancer prognosis including maximum tumor diameter, number of axillary lymph node metastases, presence of distant metastases, expression levels of ER and PR and expression of Her-2. Correlations between clinical characteristics and NFKB1 and BIRC5 expression were assessed using logistic regression and P<0.05 was considered statistically significant.Since not all items had control groups, samples without controls and duplicate samples were excluded, and valid clinical information was retained. We used Chi-squared test to investigate the relationship between blood expression of NF-κB and survivin mRNA and clinical characteristics, including tumor stage and molecular subtype, in 26 breast cancer patients screened.Kaplan-Meier and Log rank tests were used for survival analysis to investigate the association of NF-κB and survivin with OS of the patients.
Therapeutic Value
Survivin expression was down-regulated using siRNA and its effects on proliferation and apoptosis of breast cancer cells were investigated.21 We follow the siRNA design principles to identify three target sequences that match the siRNA profile, and additionally synthesized missense RNAs as a negative control group. The siRNA oligonucleotide sequences used in this study are shown in Table 2. The screened siRNA oligonucleotide sequences were transfected into MDA-MB-231 cells in good growth condition for culture. The cells were divided into control and siRNA transfected groups. The proliferation rate of each group of cells was measured using the CCK-8 reagent in accordance with the manufacturer’s instructions and the AnnexinV-APC/7-AAD Apoptosis Kit was used to measure the apoptosis rate in each group of cells disturbed. The Varian X-ray irradiation system was used to irradiate the cells.22 Irradiation was performed at room temperature using an external pre-filter. Each group of cells was radiated with 2 Gy of X-rays. All experiments were conducted three times for replication.
 |
Table 2 The Oligonucleotide siRNA Sequences |
Results
NF-κB and Survivin Gene (NFKB1 and BIRC5) Expression
We analyzed 113 normal human tissues and 1099 tissues from tumor patients From the TCGA databases. The results revealed significant differences in the expression levels of NF-κB1 and BIRC5 in normal and cancerous tissues, as depicted in Table 3. NFKB1 expression was lower in tumor tissues of BLCA, BRCA, COAD, HNSC, LUAD, LUSC, PRAD, THCA, UCEC, and KICH than in normal tissues (P < 0.05); higher in tumor tissues of CHOL, ESCA, GBM, KIRC, and STAD than in tissues (P < 0.05). The expression of BIRC5 was differentially expressed in all tumors and normal tissues. (P < 0.05). NFKB1 was expressed higher in normal tissues than in breast cancer tissues, and BIRC5 was expressed higher in breast cancer tissues than in normal tissues (P < 0.05).(Figure 1a and b).
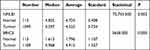 |
Table 3 NFΚB1 and BIRC5 Expression in Pan Carcinoma |
Molecular subtypes of breast cancer are classified based on the presence or absence of hormone receptors and Her-2, including hormone receptor positive and HER2 negative (LuminalA), hormone receptor positive and HER2 positive (LuminalB), hormone receptor negative and HER2 positive (HER2), and hormone receptor negative and HER2 negative (basal-like or triple negative breast cancers (TNBC)). We used UALCAN to assess the relationship between gene expression and molecular subtypes of breast cancer. We found that NFKB1 was highly expressed in the luminal subtype and BIRC5 was highly expressed in the TNBC subtype (Figure 2a and b). TNBC breast cancers can be further subdivided into six subtypes: luminal androgen receptor (LAR), basal-like-1 (BL-1), basal-like-2 (BL-2), immunomodulatory (IM), mesenchymal (M), and mesenchymal stem (MSL). We further analyzed the expression of NFKB1 and BIRC5 in TNBC, and the results indicate that NFKB1 expression is higher in IM subtype than other subtypes (P<0.05), and BIRC5 expression is higher in BL-2 than other subtypes (P < 0.05)(Figure 2c and d).
In this study, we analysed the relationship between NFKB1 and BIRC5 in the TCGA database and the clinical characteristics of breast cancer patients. The expression of NFKB1 in breast cancer tissues was not associated with tumour size, number of axillary lymph node metastases or distant metastases in breast cancer patients (P≥0.05), while the expression of BIRC5 was associated with all these clinical characteristics (P<0.05), as depicted in Figure 3a and b.
 |
Figure 3 NFKB1 and BIRC5 with clinical features of breast cancer. (a) NFKB1 with clinical features of breast cancer. (b) BIRC5 with clinical features of breast cancer. |
The NF-κB family has five members, including the proto-oncogenes c-Rel, NFKB1 (p50/p105), NFKB2 (p50/p100), RelA (p65), and RelB.23 Based on Pearson correlation analysis, we found that NFKB1 and BIRC5 were negatively correlated and the difference was statistically significant (R=−0.193, P<0.05), NFKB2 and RelA were positively correlated with BIRC5 (R=0.075, P<0.05;R=0.067, P<0.05), and RelB was not associated with BIRC5 (P≥0.05).
NF-κB and Survivin mRNA Expression
We investigated the mRNA expression levels of NF-κB and survivin and defined < 1 as negative expression and ≥ 1 as positive expression. The positive expression of NF-κB was 53.85% (14/26) and that of survivin was 73.08% (19/26). In relapsed patients, it was 47.62% (10/21), while that of survivin was 71.43% (15/21). The average of NF-κB was 1.515/1.116 in non-relapsed and relapsed patients, respectively; P = 0.284, and the average of survivin was 1.712/1.781 in non-relapsed and relapsed patients, respectively; P =0. 894.The mRNA expression of both was not related to recurrence. (Table 4) (Figure 4a and b).
 |
Table 4 NF-κB and Survivin mRNA Expression in Relapsed and Non-Relapsed Patients |
The relationship between NF-κB and survivin and the molecular subtypes of the patients suggest that the NF-κB and survivin was not related to LuminalA, LuminalB, HER2, and TNBC subtype (P ≥0.05), as depicted in Table 5.
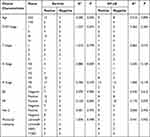 |
Table 5 mRNA Expression of NF-κB and Survivin in BRCA Patients with Clinical Characteristics |
The relationship between NF-κB and survivin and the clinical characteristics of the patients suggest that the expression of NF-κB and survivin was not related to the age at first, tumour size (T stage), number of axillary lymph node (N stage) or distant metastases (M stage) breast cancer (P ≥0.05), as depicted in Table 5.
Based on Spearman correlation analysis, NF-κB expression was positively correlated with survivin mRNA expression (R=0.903, P < 0.05).
Survival Analysis
We analyzed the relationship between NF-κB1 and BIRC5 with the prognosis of breast cancer patients in the TCGA database and found that there were no significant associations between NF-κB1 and BIRC5 and overall survival (OS) of breast cancer patients (HR=0.68, P=0.11; HR=1.53, P=0.05). (Figure 5a and b). There were 14 patients with high NF-κB expression, of whom 5 died, and 12 patients with low NF-κB expression, of whom 2 died. There were 19 patients with high survivin expression, of whom 7 died, and 7 patients with low survivin expression, all of whom survived. There was a statistically significant difference in patient mortality in the NF-κB and survivin high expression group compared to the low expression group (P<0.05). Similar to the results for genes and prognosis in the TCGA database, positive expression of NF-κB and survivin was not associated with OS of patients (χ2 = 2.996, P = 0.083, χ2 = 2.426, P = 0.119) (Figure 6a and b).
 |
Figure 5 The relationship between NFKB1 and BIRC5 and OS. (a) The relationship between NFKB1 and OS. (b) The relationship between BIRC5 and OS. |
 |
Figure 6 The relationship between NF-κB and Survivin and OS. (a) The relationship between NF-κB and OS. (b) The relationship between Survivin and OS. |
Therapeutic Value
We selected the triple negative breast cancer MDA-MB-231 cell line and used RT-PCR to detect the expression of the survivin gene after silencing its mRNA level and selected three small interfering RNAs—survivin-homo-110, survivin-homo-308, and survivin-homo-404.The sequences of each siRNA are shown in detail in Table 2. Breast cancer cells were divided into the control group and survivin-siRNA group. mRNA expression was calculated according to 2−ΔΔCt. The results suggest that survivin-homo-404 had the most significant inhibitory effect on survivin compared to the control group (P<0.05) (Figure 7a). Survivin-homo-404 was eventually selected for subsequent experiments. After transfecting MDA-MB-231 cells with this RNA interference sequence, the relative expression of survivin mRNA was measured, and the results suggest that survivin mRNA was significantly decreased after using siRNA interference. (Figure 7b)
The CCK-8 kit and AnnexinV-APC/7-AAD Apoptosis Detection Kit were used to measure cell proliferation and apoptosis rates before and after survivin interference. When unirradiated, cell proliferation rates were decreased and significantly different between the control and survivin-siRNA groups (P < 0.05). After X-ray irradiation, there was no significant difference between the control and survivin-siRNA groups in the proliferation rate (P ≥ 0.05) and the apoptosis rate increased (P < 0.05) compared to before irradiation. The results indicate that siRNA had little effect on cell proliferation but had a greater effect on apoptosis (Figure 8a and b).
 |
Figure 8 Proliferation and apoptosis rates of each group. (a) Proliferation rates of each group. (b) Apoptosis rates each group. |
Discussion
Worldwide, breast cancer is the main cause of cancer-related deaths among women.2 After tumor removal, a substantial proportion of breast cancer patients experience recurrence and have a poor prognosis.24 With the advancement of bioinformatics, identifying the appropriate biomarkers is important for the survival of breast cancer patients.
NF-κB is the generic name for a family of transcription factors that regulate genes linked with immunity, inflammation, and cell survival by functioning as dimers. The translocation of activated NF-κB into the nucleus increases the expression of genes involved in various biological processes. Inappropriate activation of NF-κB is associated with several inflammatory diseases, while its effect on tumour cells is unclear. We analyzed the expression of NF-κB gene in pan-cancer based on TACG databases and their relevance to prognosis of breast cancer patients and found that the genes for NF-κB (NFKB1) were expressed at significantly different levels in normal and cancerous tissues.In different molecular subtypes of breast cancer, NFKB1 was highly expressed in the luminal subtype. In TNBC subtype, NFKB1 expression is higher in IM subtype than other subtypes. Survivin is a potent inhibitor of apoptosis, it has been demonstrated that patients with high survivin expression are more responsive to radiotherapy.12 We investigated the expression of the gene encoding survivin, BIRC5, in pancytopenia, and found that BIRC5 was more highly expressed in breast cancer tumor tissues than in normal tissues. Subgroup analysis studies have found that BIRC5 was highly expressed in TNBC subtypes, and was expressed higher in BL-2 than in other subtypes.
The regulatory roles of NF-κB and survivin in cell cycle and cell death pathways make them prospective targets for tumor control, but their precise molecular activities and interrelationships remain unknown.14 To our knowledge, we are the first group to study NF-κB and survivin together. When validated in blood specimens from breast cancer patients, we found that NF-κB was found to be positively correlated with survivin mRNA expression. This may be related to the following factors:Firstly, NF-κB is a dimer composed of NFKB1 (p50) and RelA(p65). In the cytoplasm, NF-κB binds to IκBα in an inhibited state, which can be degraded by p-IKKα/β via the ubiquitination pathway, leaving NF-κB in a free state, leading to activation of the NF-κB signaling pathway. Improper regulation of NF-κB is associated with cancer, inflammatory and autoimmune diseases, infectious shock, viral infections and improper immune development.9 Research reported that YM155, a small molecule inhibitor of survivin, inhibited the NF-κB signaling pathway in renal clear cell carcinoma and reduced the level of p65 phosphorylation expression and attenuated the transcriptional capacity of the p65/p50 heterodimer.24 Therefore, inhibition of survivin may be involved in suppressing NF-κB signaling pathway and promoting apoptosis. Secondly, Zeng’s research demonstrated that regulation of survivin expression was accompanied by regulation of p65 and its upstream genes IKKα and IKKβ at the transcriptional level.25 Our study confirmed at the mRNA level that NF-κB was positively correlated with survivin expression, which is in line with the above study.
As for the gene level, we found that NFkB1 was negatively correlated with survivin expression, while it is positively correlated with the rest of the NF-κB family members. Therefore, the inner-relationship between NF-κB and survivin-encoding genes requires more experimental studies.
NF-κB and survivin were not significantly associated with OS of breast cancer patients at mRNA levels. At gene levels, compared to the low expression group, high survivin (BIRC5) expression group is associated with patient prognosis. Hseu suggested that aberrant activation of NF-κB signaling is associated with the development of various cancers, including breast cancer.26 Sirotkin demonstrated that NF-κB can influence the expression of Wnt-related genes through its interaction with β-catenin, thus having an impact on the ability of tumors to recur and metastasize.27 Our results are similar to those of other studies, suggested that NF-κB and survivin may be associated with signaling pathways in breast carcinogenesis, and both may suggest poor prognosis in breast cancer.
In this study, we utilized RNA interference technology(siRNA) to examine the effects of down-regulation of survivin on the proliferation and apoptosis of breast cancer MDA-MB-231 cells. The results shows that the proliferation rate decreased and apoptosis rate increased, while after X-ray irradiation, the apoptosis rate increased significantly. We have validated blood specimens from breast cancer patients and found that the expression trends of NF-κB and survivin are approximately the same, therefore, interfering with survivin may inhibit the NF-κB and thus enhance the radiosensitivity of cells.The development of co-inhibitors of survivin and NF-κB may be considered in the future for the treatment strategy of breast cancer patients.
There are several limitations to this study. First, validation of down- or up-regulated genes needs to be performed in multiple cell lines of breast cancer. Second, we evaluated gene expression of NF-κB and survivin in the TCGA database, but differences in mRNA expression levels of both in healthy populations and in studies and tissues from tumour patients should also be evaluated, and more fresh tissues need to be collected for future experiments. In addition, NF-κB and survivin are not cell membrane surface molecules, thus suitable carrier molecules should be selected to overcome these limitations in the future.
Conclusion
In this study, we analysed the expression of NF-κB and survivin between pan-cancer, breast cancer and their molecular subtypes using the TACG database and the Ualcan website. It is suggested that NF-κB and survivin were correlated at the gene and mRNA levels. Gene and mRNA expression of NF-κB was not associated with clinical features of breast cancer or with prognosis. Gene expression of survivin was associated with clinical features of breast cancer and with prognosis, mRNA expression of survivin was not associated with clinical features or with prognosis. Regulation of mRNA expression levels of survivin may help to improve radiosensitivity in breast cancer patients. In the future, the development of inhibitors of NF-κB or survivin may be an effective measure for the treatment of breast cancer.
Data Sharing Statement
We confirm that our article contains a Data Availability Statement. All the data in this study are available from TCGA database (https://portal.gdc.cancer.gov).
Ethics Approval and Consent to Participate
The study protocol was approved by the Ethics Committee of The Affiliated Cancer Hospital of Xinjiang Medical University . Approval number is K-2021070. The study was conducted in accordance with the Declaration of Helsinki. We promote and ensure respect for human subjects and the protection of their health and rights. The modification study was approved by the Ethics Committee, patient privacy was treated confidentially and without apparent harm, and some of the results of this study may be used to treat patients in the future. All patients were obtained informed consent before the experiment.
Acknowledgments
We thank the members of the Affiliated Cancer Hospital of Xinjiang Medical University. And Q.C received funding for the project from the Natural Science Foundation of Xinjiang Uygur Autonomous Region.
Funding
This work was supported by the Natural Science Foundation of Xinjiang Uygur Autonomous Region (Grant number:2021D01C417).
Disclosure
No potential conflict of interest was reported by the authors.
References
1. Mokdad AH, Dwyer-Lindgren L, Fitzmaurice C, et al. Trends and patterns of disparities in cancer mortality among US counties, 1980–2014. JAMA. 2017;317(4):388–406.PMID: 28118455; PMCID: PMC5617139. doi:10.1001/jama.2016.20324
2. Wapnir IL, Khan A. Current strategies for the management of locoregional breast cancer recurrence. Oncology. 2019;33(1):19–25. PMID: 30731014.
3. Yap KM, Sekar M, Seow LJ, et al. Mangifera indica (Mango): a promising medicinal plant for breast cancer therapy and understanding its potential mechanisms of action. Breast Cancer. 2021;13:471–503. PMID: 34548817; PMCID: PMC8448164. doi:10.2147/BCTT.S316667
4. Nagini S. Breast cancer: current molecular therapeutic targets and new players. Anticancer Agents Med Chem. 2017;17(2):152–163.PMID: 27137076. doi:10.2174/1871520616666160502122724
5. Ferlay J, Colombet M, Soerjomataram I, et al. Cancer statistics for the year 2020: an overview. Int J Cancer. 2021;149:778–789. PMID: 33818764. doi:10.1002/ijc.33588
6. Subramaniyan V, Fuloria S, Gupta G, et al. A review on epidermal growth factor receptor’s role in breast and non-small cell lung cancer. Chem Biol Interact. 2022;351:109735. PMID: 34742684. doi:10.1016/j.cbi.2021.109735
7. Rabbani F, Yazdiniapour Z, Ghanadian M, Zolfaghari B, Maleki M, Shafiee F. Cytotoxicity and apoptosis assay of novel cyclomyrsinol diterpenes against breast cancer cell lines. World J Tradit Chin Med. 2022;8:273–277. doi:10.4103/wjtcm.wjtcm_6_21
8. Zhu G, Cheng Z, Lin C, et al. MyD88 regulates LPS-induced NF-ĸB/MAPK cytokines and promotes inflammation and malignancy in colorectal cancer cells. Cancer Genomics Proteomics. 2019;16(6):409–419.PMID: 31659096; PMCID: PMC6885359. doi:10.21873/cgp.20145
9. Chamanara M, Abdollahi A, Rezayat SM, et al. Thymol reduces acetic acid-induced inflammatory response through inhibition of NF-kB signaling pathway in rat colon tissue. Inflammopharmacology. 2019;27(6):1275–1283.PMID: 30903350. doi:10.1007/s10787-019-00583-8
10. Sharma N, Zahoor I, Sachdeva M, et al. Deciphering the role of nanoparticles for management of bacterial meningitis: an update on recent studies. Environ Sci Pollut Res Int. 2021;28(43):60459–60476.PMID: 34545518;PMCID: PMC8452126. doi:10.1007/s11356-021-16570-y
11. Li F, Ambrosini G, Chu EY, et al. Control of apoptosis and mitotic spindle checkpoint by survivin. Nature. 1998;396(6711):580–584.PMID: 9859993. doi:10.1038/25141
12. Cheung CH, Cheng L, Chang KY, Chen HH, Chang JY. Investigations of survivin: the past, present and future. Front Biosci. 2011;16(3):952–961.PMID: 21196211. doi:10.2741/3728
13. Yap KM, Sekar M, Fuloria S, et al. Drug delivery of natural products through nanocarriers for effective breast cancer therapy: a comprehensive review of literature. Int J Nanomedicine. 2021;16:7891–7941. PMID: 34880614; PMCID: PMC8648329. doi:10.2147/IJN.S328135
14. Ali S, Mondal N, Choudhry H, et al. Current management strategies in breast cancer by targeting key altered molecular players. Front Oncol. 2016;6:45. PMID: 26973813; PMCID: PMC4771739. doi:10.3389/fonc.2016.00045
15. Blum A, Wang P, Zenklusen JC. SnapShot: TCGA-Analyzed Tumors. Cell. 2018;173(2):530.PMID: 29625059. doi:10.1016/j.cell.2018.03.059
16. Chandrashekar DS, Bashel B, Balasubramanya SAH, et al. UALCAN: a portal for facilitating tumor subgroup gene expression and survival analyses. Neoplasia. 2017;19(8):649–658.PMID: 28732212; PMCID: PMC5516091. doi:10.1016/j.neo.2017.05.002
17. Bishara AJ, Hittner JB. Testing the significance of a correlation with nonnormal data: comparison of Pearson, Spearman, transformation, and resampling approaches. Psychol Methods. 2012;17(3):399–417.PMID: 22563845. doi:10.1037/a0028087
18. Nunes BTD, de Mendonça MHR, Simith DB, et al. Development of RT-qPCR and semi-nested RT-PCR assays for molecular diagnosis of hantavirus pulmonary syndrome. PLoS Negl Trop Dis. 2019;13(12):e0007884.PMID: 31877142; PMCID: PMC6932758. doi:10.1371/journal.pntd.0007884
19. Shen C, Panda S, Vogelstein JT. The chi-square test of distance correlation. J Comput Graph Stat. 2022;31(1):254–262.PMID: 35707063; PMCID: PMC9191842. doi:10.1080/10618600.2021.1938585
20. Lin T, Chen T, Liu J, Tu XM. Extending the Mann-Whitney-Wilcoxon rank sum test to survey data for comparing mean ranks. Stat Med. 2021;40(7):1705–1717.PMID: 33398899. doi:10.1002/sim.8865
21. Rao DD, Vorhies JS, Senzer N, Nemunaitis J. siRNA vs. shRNA: similarities and differences. Adv Drug Deliv Rev. 2009;61(9):746–759.PMID: 19389436. doi:10.1016/j.addr.2009.04.004
22. Glide-Hurst CK, Lee P, Yock AD, et al. Adaptive Radiation Therapy (ART) strategies and technical considerations: a state of the ART review from NRG oncology. Int J Radiat Oncol Biol Phys. 2021;109(4):1054–1075.PMID: 33470210; PMCID: PMC8290862. doi:10.1016/j.ijrobp.2020.10.021
23. Malviya R, Raj S, Fuloria S, et al. Evaluation of Antitumor Efficacy of Chitosan-Tamarind Gum Polysaccharide Polyelectrolyte Complex Stabilized Nanoparticles of Simvastatin. Int J Nanomedicine. 2021;16:2533–2553. PMID: 33824590; PMCID: PMC8018389. doi:10.2147/IJN.S300991
24. Sim MY, Yuen JSP, Go ML. Anti-survivin effect of the small molecule inhibitor YM155 in RCC cells is mediated by time-dependent inhibition of the NF-κB pathway. Sci Rep. 2018;8(1):10289.PMID: 29980758; PMCID: PMC6035265. doi:10.1038/s41598-018-28213-3
25. Zeng W, Li H, Chen Y, et al. Survivin activates NF‑κB p65 via the IKKβ promoter in esophageal squamous cell carcinoma. Mol Med Rep. 2016;13(2):1869–1880.PMID: 26718331. doi:10.3892/mmr.2015.4737
26. Hseu YC, Lin YC, Rajendran P, et al. Antrodia salmonea suppresses invasion and metastasis in triple-negative breast cancer cells by reversing EMT through the NF-κB and Wnt/β-catenin signaling pathway. Food Chem Toxicol. 2019;124:219–230. PMID: 30529123. doi:10.1016/j.fct.2018.12.009
27. Sirotkin AV, Alexa R, Kišová G, et al. MicroRNAs control transcription factor NF-kB (p65) expression in human ovarian cells. Funct Integr Genomics. 2015;15(3):271–275. PMID: 25403593. doi:10.1007/s10142-014-0413-0
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




