Back to Journals » Vascular Health and Risk Management » Volume 16
Should Bangladeshi Race Be Considered as an Independent Risk Factor for Multi Vessel Coronary Artery Disease?
Authors Vasudev R, Shah P, Patel J, Naranjo M, Hosein K , Rampal U, Patel H, Bu J, Roy J, Guragai N, Bhandari P , Virk H, Shamoon F , Bikkina M
Received 3 October 2019
Accepted for publication 19 March 2020
Published 14 April 2020 Volume 2020:16 Pages 143—147
DOI https://doi.org/10.2147/VHRM.S233303
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Daniel Duprez
Rahul Vasudev,1 Priyank Shah,2 Jaimy Patel,3 Maria Naranjo,1 Kevin Hosein,1 Upamanyu Rampal,1 Hiten Patel,4 Jingnan Bu,1 Justin Roy,1 Nirmal Guragai,1 Pragya Bhandari,5 Hartaj Virk,1 Fayez Shamoon,1 Mahesh Bikkina1
1Department of Cardiology, St Joseph Regional Medical Center, Paterson, NJ, USA; 2Department of Cardiology, Phoebe Putney Memorial Hospital, Albany, GA, USA; 3Department of Internal Medicine, St Michel Medical Center, Newark, NJ, USA; 4Department of Cardiology, Cape Fear Valley Medical Center, Campbell University, Fayetteville, NC, USA; 5Department of Internal Medicine, Manipal College of Medical Sciences, Pokhara, Nepal
Correspondence: Pragya Bhandari
Department of Internal Medicine, Manipal College of Medical Sciences, Pokhara, Nepal
Email [email protected]
Introduction: Coronary Artery Disease (CAD) continues to be on the rise not only in the Western developed world but also affecting the South Asian race, particularly Bangladeshis. The objectives of this study were as follows: To determine whether or not risk factors of Bangladeshis differ from non-Bangladeshis, whether there is any difference in the extent of CAD for both groups, and if there are risk factors that can significantly affect the extent of CAD
Methods: All patients with a diagnosis of CAD admitted to our 800-bed tertiary care hospital between January 2001 and December 2015 were retrospectively analyzed. We reviewed the age, sex, body-mass index (BMI), cardiac risk factors such as family history of CAD, dyslipidemia, hypertension, diabetes and smoking. We also reviewed coronary angiographic findings of these consecutive 150 Bangladeshis and a randomly selected group of 193 non-Bangladeshis.
Results: A total of 343 medical records were evaluated, this included two groups: 193 non-Bangladeshis and 150 Bangladeshi subjects. The Bangladeshi group was older than the non-Bangladeshi group (63.49 vs 59.22, p-value=0.001), and included a larger proportion of males than the non-Bangladeshi group (28.7% vs 15.68%, p-value=0.0116). Bangladeshi subjects are more likely to be smokers than non-Bangladeshi (11.75% vs 6.67%, χ 2=12.7, p-value=0.0004). Non-obstructive, 1-vessel, 2-vessel and 3-vessel accounts for 13.33%, 36.67%, 22%, and 28% for Bangladeshis, and 16.39%, 20.77% 34.43% and 28.42% for non-Bangladeshis, respectively. The difference of extent of CAD is significant between two groups (χ 2 =12.397, p-value=0.0061). The findings suggest that Bangladeshi ethnicity has almost 2 times the likelihood of having 1-vessel CAD at coronary angiography (OR=2.361, 95% CI 1.452– 3.839, p=0.0005).
Conclusion: This study is a pivotal starting point for further evaluating the link between Bangladeshis and CAD. In our study we found that being Bangladeshi increases the risk of having CAD and may be an independent risk factor for multi-vessel CAD.
Keywords: coronary artery disease, Bangladeshi, race
Introduction
Coronary Artery Disease (CAD) is a well-known medical health issue that continues to be on the rise not only in the Western developed world but also in developing countries in the South Asian region, particularly Bangladesh.1 In native Bangladesh, surprisingly there are some studies that demonstrate the link between being Bangladeshi and having CAD. These studies demonstrate a link between native Bangladeshi having not only premature CAD but also higher mortality risk with myocardial infarction (MI) than their non-Bangladeshi counterparts.2,3 More data need to be extrapolated from native Bangladeshis for CAD. One epidemiological study from Bangladesh showed an large rise of cardiovascular disease (CVD) from 1986 to 2006, yet the question still remains about what the more recent data from 2006 to the present time shows, only in Bangladesh but also in the United States (US).
Recent small studies from New York City (NYC) have looked at the above hypothesis of Bangladeshis being predisposed to premature CAD and extensive coronary angiographic two vessel or triple vessel diseases.4,5 We examined a slightly larger cohort of US Bangladeshis within Paterson city, New Jersey. The data shows that Paterson has the second largest Bangladeshi population in the US after NYC. The objectives of this study were as follows: 1) Whether or not the CAD risk factors of Bangladeshis differ from non-Bangladeshis; 2) Whether there is any difference in the extent of CAD between the two groups; and 3) If there are risk factors that can significantly affect the extent of CAD.
Methods
After approval from our institutional review board (IRB) all patients with a diagnosis of CAD admitted in the 800 beds tertiary care hospital in Paterson between January 2001 and December 2015 were retrospectively analyzed. The present study was approved by the IRB at the St Joseph’s Healthcare System, Paterson, New Jersey, USA. Patient consent to review their medical records was not required by the IRB. The study compiled with the Declaration of Helsinki and exemption from full review and patient informed consent due to the anonymized data collection. The main inclusion criteria were age ≥ 35, presenting with ischemic symptoms including acute coronary syndrome, and history of cardiac catheterization during the above time frame. Bangladeshi race was determined based upon nationality or self-declaration by the patient. Non-Bangladeshis population included Caucasians, Hispanics, African Americans but excluded other South Asian countries like India and Pakistan. We reviewed the factors such as age, sex, and body-mass index (BMI). We also reviewed risk factors for CAD such as dyslipidemia, hypertension, diabetes, smoking and family history of CAD. Patients whose race was not possible to document were excluded from the study. There were 150 Bangladeshis and another randomly selected group of 193 non-Bangladeshis included in the study for whose angiographic findings were analyzed. The outcomes we examined were CAD with 4 levels – 0 (non-obstructive), 1 (single vessel), 2 (two vessel), 3 (triple vessel) from which we examined the relationships between the aforementioned risk factors. CAD was defined based upon angiographic findings. No apparent CAD: no stenosis > 20%; non obstructive CAD: ≥1 stenosis ≥ 20% but no stenosis ≥70%; obstructive CAD: any stenosis ≥ 70% or left main (LM) stenosis ≥ 50%. There are mainly three steps in this study: first, we compared the risk factors of both groups. Secondly, the extent of CAD was compared for both groups. Third, logistic regression was performed to estimate the effects of risk factors on CAD. The risk factors of both of these groups were compared using χ2 tests for dichotomous variables and t-tests were conducted for continuous variables. For the extent of CAD, χ2 test was used for comparing these two groups. By using logistic regression, we analyzed the effects of ethnicity and each of the risk factors to estimate the likelihood of having different extents of CAD. Odds Ratio (OR) was used to compare the extent of CAD among each group. A quick data screening showed that some factors received only several responses. For some other factors, all the observations had the same answer. Discussions of these factors were essentially meaningless, and thus not analyzed. Factors that seemed important to be analyzed are mentioned in the results section.
Results
A total of 343 medical records were evaluated, which included two groups: 193 non-Bangladeshis and 150 Bangladeshi subjects. Table 1 shows that the Bangladeshi group was older than the non-Bangladeshi group (63.49 vs 59.22, p-value=0.001), and included a larger proportion of males than the non-Bangladeshi group (28.7% vs 15.68%, p-value=0.0116). Bangladeshi subjects are more likely to be smokers than non-Bangladeshis (11.75% vs 6.67%, χ2=12.7, p-value=0.0004). The BMI between both groups is significantly different. DM and HbA1C do not differ from the two groups.
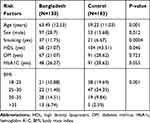 |
Table 1 Showing Demographic Comparisons Between the Bangladeshi and Non-Bangladeshi Population |
Table 2 shows the of CAD for both groups. Non-obstructive, 1-vessel, 2-vessel, and 3-vessel accounts for 13.33%, 36.67%, 22%, and 28% for Bangladeshis, and 16.39%, 20.77% 34.43% and 28.42% for non-Bangladeshis, respectively. The difference of extent of CAD is significant between the two groups (χ2 =12.397, p-value=0.0061). The findings suggested that Bangladeshi ethnicity has almost 2 times the likelihood of having 1-vessel CAD at coronary angiography (OR=2.361, 95% CI, 1.452–3.839, p=0.0005). 3-vessel coronary artery disease was slightly higher in Bangladeshis as compared to non-Bangladeshis (OR 1.054, 95% CI, 0.654–1.700, p 0.827). Meanwhile non-obstructive and 2-vessel Bangladeshis are significantly lower than that of non-Bangladeshis. DM is related to all types of CAD, while the other risk factors are more or less related, ie, age is associated with 2-vessel and 3-vessel CAD, and sex is associated with 1-vessel and 2-vessel CAD.
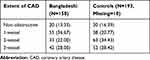 |
Table 2 Shows Extent of CAD for Both Groups |
Discussion
As previously demonstrated, being Bangladeshi, particularly being a Bangladeshi male, predisposes oneself to CAD and extensive coronary angiographic disease. Our study demonstrates that the Bangladeshi group is older than the non-Bangladeshi group and includes more males. This probably leads to more smokers. Non-obstructive and 2-vessel CAD of Bangladeshis are significantly lower than that of non-Bangladeshi, whilst 3-vessel CAD of the former is larger. Logistic regression indicates that Bangladeshi ethnicity is associated with almost 2 times the likelihood of having 2-vessel CAD. DM is related to all the types of CAD, at the same time the other risk factors are more or less related, ie, age is associated with 2-vessel and 3-vessel CAD and sex is associated with 1-vessel and 2-vessel CAD.
The smaller studies that have been performed in the USA have shown links between being Bangladeshi and premature CAD associated with high mortality and morbidity. Possible explanations for this theory are of course multifactorial, which can be either non modifiable or modifiable factors. Non-modifiable factors in this case would be gender, race, sex, genetics. Modifiable factors would be smoking, hypertension, hyperlipidemia and Diabetes Mellitus type 2.3
Studies have shown genetic links to CAD, such as polymorphisms involving genes regulating angiotensin-converting enzyme, apolipoprotein A (apoA), apolipoprotein B (apoB), apolipoprotein E (apoE), adipokine, homocysteine, plasminogen activator inhibitor-1, and fibrinogen.6,7 However, these are examples of those affected in all races. How about the South Asians? The Coronary Artery Disease (C4D) Genetics Consortium performed a meta-analysis of four large genome-wide association studies of CAD, two of European ancestry (PROCARDIS and HPS) and two of South Asian ancestry (PROMIS and LOLLIPOP) and found five new loci, ie, LIPA on 10q23, PDGFD on 11q22, ADAMTS7-MORF4L1 on 15q25, a gene rich locus on 7q22, and KIAA1462 on 10p11 for CAD, that have similar associations in Europeans and South Asians.8 Recently, six novel genetic loci have been identified in South Asians, which are associated with type 2 diabetes mellitus (DM), a major risk factor for CAD.9 However, many CAD genes are presently undiscovered, and it is likely that larger genome wide association studies will map further penetrance and further studies are needed to corroborate these findings; to confirm that findings in Bangladeshis apply to other South Asian groups.10
However, we examined what genetics link Bangladeshis to CAD that could support our current study findings. Dating from 2002, Morshed et al11 found a positive association between angiotensin I-converting enzyme (ACE) gene insertion/deletion (I/D) polymorphism and hypertension in a Bangladeshi population. Among the three ACE (insertion/deletion) I/D variants, the DD genotype was considered more worrisome. Both mean systolic and mean diastolic blood pressure was found to be higher in the population with DD genotype, especially in men. Further research is needed to clarify the issue. Recent studies show links between the modifiable risk factors that can cause CAD such as hypertension or hyperlipidemia but there needs to be more extensive research on Bangladeshis having specific gene polymorphisms that cause CAD and subsequent extensive double or triple coronary artery disease.
Epigenetics has been initially studied in patients with CVD for its prominent role in inflammation and vascular involvement.12 Both DNA methylation, miRNAs and epigenetic mechanisms have been described in atherosclerosis. Genetic variants and metabolomic data also play an important role in atherosclerosis which impacts lipid-related loci and the metabolites as they are primarily linked to lipoproteins.13 These can lead to accelerated atherosclerosis especially in the young population. Several biomarkers have been identified that predicted the incident of atherosclerotic cardiovascular disease (ASCVD) that predicted all-cause mortality.14 Many biomarkers represent regulators of metabolic and adipocyte homeostasis; others are involved in inflammatory pathways. Using a targeted discovery proteomic platform, studies have demonstrated novel biomarker associations with incident CVD events and validate previous genetic associations. All these factors have different predilection to different ethnic subgroup populations, including Bangladeshis.
Inflammatory biomarkers and adipocytokines (IBA) may contribute to atherosclerosis by promoting vascular inflammation. In the MASALA study, IBA did not help identify South Asians to be at risk of subclinical atherosclerosis, although associations with ASCVD events remain unclear.15 In the South Asian population, including Bangladeshi, they may have a distinct pathophysiology independent of inflammation as measured by IBA.
We ultimately are aware that hypertension, hyperlipidemia, Diabetes Mellitus type 2, smoking, diet and exercise all play an interlinked role in increasing the risk of a coronary event, however is there a reason that Bangladeshis have higher incidence of hypertension, diabetes, and smoking compared to their nonBangladeshi counterparts? So far studies strongly document the link between South Asians being known for adopting a high carbohydrate and lipid rich diet stemming from an early age into the older generation,4,16-19 this could consequently lead to metabolic syndrome which includes hypertension and hyperlipidemia causing a greater risk of CAD in South Asians generally. Smoking may be due to stigmata of stress or lower education attainment that may prevent South Asians or Bangladeshis from understanding the risk of smoking when their whole life involved smoking (first hand or second hand) to eating a particular diet as mentioned.
Our study showed that the extent of CAD is significantly higher in the Bangladeshi population as compared to non-Bangladeshis. Our study provides a stronger starting point for those to examine modifiable and non-modifiable risks for CAD in Bangladeshis and why that particular race can have greater than multi-vessel coronary artery disease. Additionally, is race a standalone independent risk factor, equivalent to being a male? If so, studies not only from the USA but also internationally including native Bangladeshis need to examine the pattern closely.
Previous studies across the USA, UK and Bangladesh have been small, ie, less than 100. In our study we almost reached 200 participants to which our data does support the hypothesis that being Bangladeshi not only increases your risk of CAD but increases the extent of CAD angiographically. The main limitation of our study is that it was conducted in one institution and included a population located in the vicinity of Paterson city in New Jersey, USA. This sample might not represent the true Bangladeshi race. In addition, socioeconomic factors, educational status, dietary factors, and approach to health care access play a vital role in clinical outcomes.
However, the future direction of this study will lead to empowering knowledge for the population and highlight the importance of CAD in South Asians, specifically in Bangladeshis. As hypothesized in the discussion the causes to support our findings are multifactorial. That is to say, the rise of metabolic syndrome, genetic predisposition combined with sedentary lifestyle and a high carbohydrate, high lipid and high glucose diet due to consuming ethnic food early on could be potentiating the risk of Bangladeshis having CAD with extensive angiographic evidence.
Conclusion
This study is a pivotal starting point for further evaluating the link between Bangladeshis and CAD. In our study, we found that being Bangladeshi increases the risk of having CAD and may be an independent risk factor for multi-vessel CAD.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yusuf S, Reddy S, Ôunpuu S, Anand S. Global burden of cardiovascular diseases: part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104:2855–2864. doi:10.1161/hc4701.099488
2. Ahsan S, Haque KMHS, Salman M, et al. Detection of ischaemic heart disease with risk factors in different categories of employees of University Grants Commission. Univ Heart J. 2009;5:e20–e23. doi:10.3329/uhj.v5i1.3436
3. Saquib N, Saquib J, Ahmed T, et al. Cardiovascular diseases and type 2 diabetes in Bangladesh: a systematic review and meta-analysis of studies between 1995 and 2010. BMC Public Health. 2012;12:434. doi:10.1186/1471-2458-12-434
4. Silbiger JJ, Ashtiani R, Attari M. Atherosclerotic heart disease in Bangladeshi immigrants: risk factors and angiographic findings. Int J Cardiol. 2011;146:e38–e40. doi:10.1016/j.ijcard.2008.12.175
5. Rahman MM, Haque SS, Rahman F, et al. Coronary angiographic profile in Bangladeshi patients with metabolic syndrome and ischemic heart disease. Mymensingh Med J. 2012;21(4):702–708.
6. Shah A, Hernandez A, Mathur D, et al. Adipokines and body fat composition in South Asians: results of the Metabolic syndrome and Atherosclerosis in South Asians Living in America (MASALA) study. Int J Obes (Lond). 2012;36:e810–e816. doi:10.1038/ijo.2011.167
7. Anand SS, Xie C, Pare ́ G, et al. INTERHEART Investigators. Genetic variants associated with myocardial infarction risk factors in over 8000 individuals from five ethnic groups: the INTERHEART genetics study. Circ Cardiovasc Genet. 2009;2:e16–e25. doi:10.1161/CIRCGENETICS.108.813709
8. Mehta NN. A genome-wide association study in Europeans and South Asians identifies five new loci for coronary artery disease. Circ Cardiovasc Genet. 2011;4:e465–e466. doi:10.1161/CIRCGENETICS.111.960096
9. Kooner JS, Saleheen D, Sim X, et al. Genome-wide association study in individuals of South Asian ancestry identifies six new type 2 diabetes susceptibility loci. Nat Genet. 2011;43:e984–e989. doi:10.1038/ng.921
10. Samani NJ, Sharma P. Coronary heart disease in South Asian populations - the role of genetics. In: Patel KCR, Bhopal RS, editors. The Epidemic of Coronary Heart Disease in South Asian Populations: Causes and Consequences.
11. Morshed M, Khan H, Akhteruzzaman S. Association between angiotensin I converting enzyme gene polymorphism and hypertension in selected individuals of the Bangladeshi population. J Biochem Mol Biol. 2002;35:e251–e254.
12. Khalil CA. The emerging role of epigenetics in cardiovascular disease. TherAdv Chronic Dis. 2014;5(4):178–187. doi:10.1177/2040622314529325
13. Battram T, Hoskins L, Curation D, et al. Coronary artery disease, genetic risk and the metabolome in young individuals, version 2. Welcome Open Res. 2018;3:114. doi:10.12688/wellcomeopenres.14788.1
14. Ho JE, Lyass A, Courchesne P, et al. Protein biomarkers of cardiovascular disease and mortality in the community. J Am Heart Assoc. 2018;7:e008108. doi:10.1161/JAHA.117.008108
15. Mehta A, Patel J, Joshi PH, et al. Inflammation and coronary artery calcification in South Asians: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis. 2018;270:49–56. doi:10.1016/j.atherosclerosis.2018.01.033
16. Fischbacher CM, Hunt S, Alexander L. How physically active are South Asians in the United Kingdom? A literature review. J Public Health (Oxf). 2004;26:250–258. doi:10.1093/pubmed/fdh158
17. Jahan K, Hossain M. Nature and Extent of Malnutrition in Bangladesh, Bangladesh National Nutrition Survey, 1995–1998. Dhaka: Institute of Nutrition and Food Science, Dhaka University, Bangladesh; 1998.
18. Hossain MM. Consumption in Rural Bangladesh: Households, Lifestyles, and Identities [Dissertation]. University of Helsinki; 2011.
19. Gupta M, Brister S, Verma S. Is South Asian ethnicity an independent cardiovascular risk factor? Can J Cardiol. 2006;22:193–197. doi:10.1016/S0828-282X(06)70895-9
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
