Back to Journals » Clinical Ophthalmology » Volume 16
Short-Term Fit Assessment of a Novel Daily Disposable, Toric, Silicone Hydrogel Contact Lens
Authors Gustafson B, Whaley S, Giedd B, Montaquila S, Edwards B, Subbaraman LN
Received 13 April 2022
Accepted for publication 19 October 2022
Published 14 November 2022 Volume 2022:16 Pages 3721—3730
DOI https://doi.org/10.2147/OPTH.S370151
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Britt Gustafson,1 Susan Whaley,2 Bradley Giedd,3 Stephen Montaquila,4 Brenda Edwards,5 Lakshman N Subbaraman6
1The Eye Doctors Inc, Eden Prairie, MN, USA; 2Tallahassee Eye Center, Tallahassee, FL, USA; 3Maitland Vision Center, Maitland, FL, USA; 4West Bay Eye Associates, Warwick, RI, USA; 5Heart of America Eye Care, Overland Park, KS, USA; 6Alcon Research, LLC, Johns Creek, GA, USA
Correspondence: Lakshman N Subbaraman, Alcon Research, LLC, Clinical Development & Medical Affairs, Johns Creek, GA, 30097, USA, Tel +1 678 415 5316, Email [email protected]
Purpose: The development of new contact lens materials and designs are necessary to minimise patient dropout. A lens material with water surface technology was recently developed to incorporate toric design. The on-eye stability of a toric contact lens is critical to a successful toric lens fitting. In an effort to establish if the new daily disposable verofilcon A toric silicone hydrogel lens provides fast stability for ease of fit, this study assessed the initial and short-term on-eye stability of this new lens.
Patients and Methods: Habitual full-time wearers of soft contact lenses, aged 18 or over, were enrolled and fit with the verofilcon A toric lens. Study endpoints included lens settling time, axis orientation at specific time-points within 10 minutes after insertion, lens oscillation with blink, lens movement and centration, and scribe mark visibility.
Results: Thirty-nine subjects completed the study; 67% were female and mean age was 34.1 ± 10.8 years (range 18 to 61). The majority of verofilcon A toric lenses (98.7%) settled on average within 60 seconds. Average lens orientation was 3° from six o’clock position within two minutes of insertion. The lenses showed minimal oscillation with blink; 98.7% of the eyes demonstrated ≤ 5° oscillation with blink. All lenses showed optimal/acceptable lens movement and centration and the scribe mark was reported as easily visible in 96% of eyes. Practitioners reported a 99% first lens fit success rate.
Conclusion: The novel verofilcon A toric lens was highly successful with the first lens, had excellent on-eye stability and good fit characteristics. These qualities make this new lens a good option for lens wearers. Furthermore, it fulfills the needs of practitioners who want a toric lens that is easy and predictable to fit.
Keywords: verofilcon A, easy to fit, settling time, orientation, surface technology
Introduction
There is a discrepancy between the prevalence of astigmatism in the population and the prevalence of toric contact lens prescribing. A survey of optometry records, mainly from the United States, revealed that 41% of patients presented with at least −0.75D astigmatism in one or both eyes.1 In the United Kingdom, 47% of patients seeking soft contact lens wear were estimated to have −0.75D or greater of astigmatism in at least one eye.2 However, toric soft contact lenses account for about 30% of all soft contact lens fittings.3 This discrepancy between the need for a toric lens and the type of lenses Eye Care Practitioners (ECPs) actually fit is possibly due to the perception that ECPs may have about toric lenses being complicated and time-consuming to fit.4 Global contact lens markets are seeing an increased uptake in the fitting of silicone hydrogel (SiHy) materials compared to hydrogels and a trend to fitting more daily disposable lenses compared to reusable lenses.3
Although new contact lens materials and designs have been released over the years, discomfort and poor vision continue to be leading causes of why people discontinue lens wear.5–7 Good vision and comfort that can last throughout the day are dependent on having a stable tear film.8 One advancement in lens technology has been the creation of a new daily disposable silicone hydrogel lens material with water surface technology. The spherical lens design has good clinical acceptance,9 fits well,10 provides a more stable tear film compared to other lenses,11,12 and has good comfort and vision.13–15 The spherical lens design has recently been modified to incorporate toric prescriptions. The first step in testing the new toric lens requires assessment of the fit and toric properties of the lens to investigate whether the lens performs well.
The on-eye stability of a toric contact lens is critical to a successful toric lens fitting and the resulting visual acuity. There are several lens stabilization designs available to keep the cylinder correction power aligned with the axis of astigmatic error. These designs include prism ballasts, periballasts, back-surface toricity, thin zones (double slab-off), truncations and combinations of multiple designs into one lens.16,17 Prism ballast designs incorporate base-down prism, using the thicker bottom portion of the lens to weigh it down to maintain lens orientation.18 Periballast lenses use a similar prism concept, but the prism does not extend to the middle of the lens, therefore keeping the lens thinner and allowing more oxygen permeability.16 Back toric designs stabilize lenses by matching corneal toricity.16 Thin zone designs have thinner superior and inferior regions intended to sit under the upper and lower eyelids respectively, utilizing blinking to stabilize any lens rotation.16 Truncation designs truncate the lower part of the lens such that the lower straight edge aligns with the lower lid margin to maintain stability.18 Some newer toric lens designs combine multiple toric stability designs into one lens. To be successful, toric lenses must orient to a predictable and repeatable position for an individual each time the lenses are inserted. Furthermore, toric lenses must attain that stable orientation quickly after insertion such that clear vision is achieved promptly. Toric lenses can settle quickly with 77% of lenses oriented within 5° of the ideal location within a minute19 and between 80% to 93% rotated up to 10°.19–21 A toric lens is more likely to become the lens of choice of ECPs if it orients predictably and settles quickly at every fitting. Poor lens orientation has been reported with as few as 26% of the lenses within 10° of its ideal position, and rotation of 56.6° to 78.6° after 20 minutes of settling.22 However, other toric lenses can orient well after they have settled with 50% to 100% orientated within 10°.19,21–25
The new SiHy verofilcon A toric lens investigated in this study utilizes a modified prism ballast stabilization design (PRECISION BALANCE 8|4®).12,26 This design is engineered to work with the eye’s blinking mechanism by stabilizing the lens at eight and four o’clock and providing a thinner region at six o’clock to reduce lower lid interaction while maintaining a wide optic zone. The scribe mark at six o’clock allows for quick and easy orientation identification during fittings.
Orientation is the major factor affecting vision through a toric lens,27 but the success of a lens also relies on comfort which is heavily influenced by the material properties and surface characteristics of a lens.28 Verofilcon A is a new SiHy material that has a high Dk 90×10−11 barrers, a high centre oxygen transmissibility (Dk/t) of 100 barrers/cm at –3.00 D and a low modulus of elasticity of 0.6 MPa.29 The lens offers a high water content surface technology (SMARTSURFACE® Technology)30 which provides a micro-thin hydrogel surface layer of 80% water that encases the 51% water content core.31 This high water content surface is designed to enhance comfort32 and support an optically precise tear film.33
This study was conducted to assess the initial and short-term on-eye stability of this new daily disposable verofilcon A toric lens.
Materials and Methods
Study Design
This was a prospective, open label, single-arm, bilateral, multicenter, non-dispense clinical study conducted across five clinical practice sites in the US. Ethics approval was attained from Sterling Independent Services Inc. – Institutional Review Board for all sites involved. Written informed consent was obtained from all subjects prior to enrolment in the study and prior to any data collection. The ClinicalTrials.gov identifier number is NCT04464044 (registered July 7, 2020) and the study results are available at https://clinicaltrials.gov/ct2/show/NCT04464044. Due to the varying rights of individuals and contractual rights of parties involved, Alcon does not make a practice of sharing datasets. All procedures adhered to the tenets of the Declaration of Helsinki. The ECPs were all trained on their clinical investigator tasks. All subjects attended a single non-dispensing study visit and wore test lenses for approximately 1 hour. There was no control group.
Cohort
Subjects were included in the study if they were: 18 years or older; habitual wearers of soft contact lenses in both eyes for a minimum of 5 days a week and 8 hours per day during the last 3 months. Because of the restricted lens powers available for this study, subjects were required to achieve acuity of 20/25 or better in each eye with their manifest refraction, and to have a cylindrical correction of –0.75 or –1.25 D at axis 90° or 180° and a sphere component of –1.00 or –3.00 D (allowing a tolerance of ±0.50 D in sphere, ±0.25 D in cylinder power and ±5° in axis from manifest refraction).
Subjects were excluded from the study if: their habitual contact lens modality in the last 3 months was extended wear (ie, sleeping in lenses at least once per week); they were found to have on biomicroscopy screening ≥Grade 3 corneal neovascularization (>1.5 mm vessel penetration as defined by the International Organization for Standardization (ISO) 11980:2012(E): Ophthalmic optics – Contact lenses and contact lens care products – Guidance for clinical investigations),34 any infiltrates, or irregular corneas. Subjects were also excluded if they had any history of eye injury or eye surgery within the previous 12 months; current or history of herpetic keratitis in either eye; or any anterior segment infection, inflammation, or disease (including systemic) or use of any systemic or ocular medications where contact lens wear would be contraindicated.
Study Materials
The contact lens fit to all eyes was the verofilcon A toric lens (PRECISION1® for Astigmatism, Alcon). The material has a light blue handling tint and provides Class 1 UV filtration. The parameters were 8.5 mm base curve and 14.5 mm diameter. The following lens powers were available in this study:
 |
|
Assessments
Subjects were fit with the toric study lenses and the lens fit was immediately evaluated using a slit-lamp biomicroscope. The following endpoints were assessed:
Lens Settling Time
Lens settling time was defined as the amount of time taken (in seconds) for the scribe mark orientation to reach its resting (settled) position based on the ECP’s clinical judgement. Lens settling time was assessed for a maximum of 10 minutes.
Lens Scribe Orientation
Lens scribe orientation was evaluated relative to the six o’clock position (in degrees) by aligning a thin slit beam over the scribe mark. The amount of rotation was assessed using the protractor scale on the slit lamp and measured at 1, 2, 3, 5, and 10 minutes after lens insertion. The orientation degrees were analyzed as absolute values, meaning they were not assigned a negative or positive value depending on whether the orientation was nasal or temporal.
Lens Oscillation with Blink
The amount of rotational swing exhibited by the lens due to blinking (in degrees) was reported as one of four categories: no oscillation, <3°, 3–5° or >5°. Lens oscillation was assessed at least 10 minutes after insertion.
Lens Fit Evaluation
Lens fit was evaluated by lens movement and lens centration after the lenses were worn for more than 10 minutes. Lens movement with a blink was graded using the ISO 11980:2012(E)34 five-point descriptive scale (unacceptably tight, acceptably tight, optimal, acceptably loose or unacceptably loose). Lens centration was evaluated using the ISO 11980:2012(E)34 three-point descriptive scale (optimal, acceptable decentration, unacceptable decentration).
Toric Scribe Mark Visibility
The ECPs judged the ease of scribe visibility with the biomicroscope when the lens was on eye using a three-point descriptive scale (not visible, somewhat visible or easily visible). Scribe mark visibility was assessed more than 10 minutes after lens insertion.
Statistical Analysis
Statistical analysis was performed with SAS software (SAS Institute Inc, Cary, NC). Data are presented as mean, standard deviation, median, minimum and maximum values. In some cases, percentages were also calculated. All 78 eyes of the 39 subjects were included in the data analysis.
Results
Cohort
Informed consent was obtained from 40 enrolled subjects. One subject failed screening, resulting in 39 subjects (78 eyes) being exposed to the study lenses, all of which completed the study and were included in the safety and analysis set. Subjects were generally of white race (92.3% White, 2.6% Black, 2.6% Asian, 2.6% Other) and not of Hispanic of Latino ethnicity (84.6% not Hispanic or Latino, 15.4% Hispanic or Latino). Subjects had a mean ± SD age of 34.1 ± 10.8 years (range 18 to 64 years) and 67% were female.
Safety
There were no adverse events, device deficiencies, or clinically relevant worsening in biomicroscopy findings reported in the study.
Lens Settling Time
With the exception of one contact lens that failed to settle within a 10-minute period, the remaining lenses (n=77) settled quickly and on average took less than 60 seconds to settle (mean ± SD 40.1 ± 56.8 seconds, range 0 to 300 seconds) (Table 1).
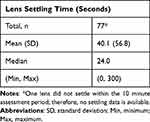 |
Table 1 Lens Settling Time (Seconds); Judgement of When Lens Orientation Has Settled After Insertion |
Lens Orientation
The mean ± SD lens orientation values at each timepoint (n=78) are shown in Figure 1. The mean ± SD primary gaze orientation was 2.7° ± 3.6° from the six o’clock position within 2 minutes. The range of lens orientation values varied by 30° at 1 minute post insertion, 10° at 5 minutes post insertion, and 15° at all other timepoints. In order to better describe the spread of these results more clearly, the lens orientation data was converted to counts that fell within clinically relevant buckets from the intended six o’clock orientation; within ±20°, ±10°, and ±5°. These were calculated for all the timepoints: at 1, 2, 3, 5 and 10 minutes after insertion (Table 2). One minute after insertion, 97.4% of the lenses were oriented within ±20° from the six o’clock position. At 2 minutes after insertion, 100% of the lenses were oriented within ±20° of the intended position. At 10 minutes, 98.7% of the lenses were oriented within ±10° from the intended 90° axis. The majority of lenses (52.6%) were perfectly aligned after 10 minutes, with 42.3% rotated in the nasal direction and 5.1% towards the temporal direction. At all time points, at least 94.9% of the lenses were within ±10° from the intended orientation (Figure 2).
 |
Table 2 Frequency Distribution of Lens Orientation at the Assessment Timepoints |
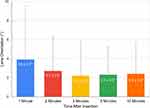 |
Figure 1 Mean (and standard deviation) lens orientation of the scribe mark relative to six o’clock position (n=78). |
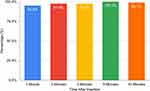 |
Figure 2 Percentage of lenses within 10 degrees of intended orientation (n=78). |
Lens Oscillation with Blink
More than half of lenses (71.8%) exhibited <3° or no oscillation upon blinking (n=78), and 98.7% of the eyes experienced ≤5° of oscillation (Figure 3).
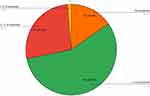 |
Figure 3 Distribution of lens oscillation with blink; count (percentage) (n=78). |
Lens Fit Assessments
None of the lenses (n=78) presented with unacceptably tight or loose movement and 88.5% were graded as optimal (Figure 4).
 |
Figure 4 Distribution of lens movement grades (n=78). |
None of the lenses (n=78) presented with unacceptable centration and 97.4% were graded as optimal centration (Figure 5).
 |
Figure 5 Distribution of lens centration grades (n=78). |
One hundred percent of the wearers (n=39) demonstrated optimal or acceptable lens movement and centration.
Toric Mark Visibility
Visible toric scribe marks were reported for all lenses (n=78), with 96.2% rated as easily visible (Figure 6).
 |
Figure 6 Distribution of toric scribe mark visibility grades (n=78). |
Discussion
Toric contact lenses accounted for almost one-third of all soft contact lenses prescribed in 2019,35 although the prevalence of astigmatism in the population is higher.1,2 For a patient to be successful in wearing toric soft contact lenses, the lens axis must orient on the eye to a repeatable position for the same individual following each insertion. Visual function can be negatively impacted when lens axis misalignments are greater than 30° from its intended orientation.36 This study showed that 98.7% of the verofilcon A toric lenses oriented within ±10° of the ideal axis at 10 minutes after insertion. Other studies have reported similar success rates with 96% to 100% of toric lenses positioned within ±10° by 10 to 15 minutes.19,21 Most ECPs would likely change the lens prescription in order to modify the cylinder axis for >10° orientation,22,37 meaning that a second trial lens may be required for 1.3% eyes. In other words, this toric lens offered 99% first lens fit success rate. This rate is similar, or better than, other reported success rates of 84% to 99.1%.19–21 In fact, verofilcon A toric lenses orient, on average, 3° from the ideal orientation within 2 minutes of insertion, indicating a practical lens choice for busy clinicians.
Quick settling time allows patients to achieve clear vision in a very short time period, which reduces the amount of time needed to assess the lens and improves ECP office flow.38 For the 77 out of 78 lenses that did settle quickly, they took on average less than 60 seconds to settle following insertion. Practitioners require the scribe mark to orient at, or very close to, the six o’clock position within just a few minutes post-insertion. These lenses were shown to orient and settle rapidly, on average, 3° from their ideal location within 2 minutes. Other toric daily disposable lenses have been reported to rotate on average 5.9° to 14.1° 1 minute after insertion,21 with 85% of the lenses within 5° at 3 minutes post-insertion.19
Not all toric lenses can to be dispensed for different reasons, including poor fit,21 psychological or comfort issues,19 and poor stability of the lens orientation.25 The single lens that did not settle within 10 minutes may have needed additional time to settle. This lens was not included in the mean settling time because settling time was only recorded for a maximum of 10 minutes. Settling of the lens may have been affected by the tension or anatomy of the eyelid,38 in particular the angle of the intercanthus, the central lid angle of the upper lid, or the size of the palpebral aperture.39
There are limitations to this study. The amount of time a lens needed to settle was subjectively decided by the investigator and this could be affected by inter-investigator variability. In addition, lens orientation was assessed using a slit-lamp protractor scale to replicate how ECPs traditionally assess the fit of a lens in everyday practice. Future assessments could investigate the settling time and lens orientation with objective methods, such as with slit-lamp photographs or eye tracking videos in combination with digital image analysis.40
Practitioners evaluate lens fit and lens orientation at every lens fit and follow-up visit, and expect the toric scribe mark to be easy to identify. This study showed 100% of the wearers experienced optimal or acceptable lens movement and centration and also that verofilcon A toric lenses had an easily visible mark during biomicroscopy. In order to become the lens of choice for practitioners, the toric lens must offer a predictable orientation and provide good on-eye stability. The results demonstrate that verofilcon A toric lenses settled on average 40.1 seconds after insertion, had minimal oscillation with blinking, with 98.7% of the lenses demonstrating ≤5° of oscillation with blink, thus providing the on-eye stability astigmatic patients need. All the lenses fit well and had a 99% first-fit success rate. Only one type of contact lens was investigated in this study. Further work is warranted to investigate the subjective fitting characteristics and subjective acceptance of this new lens against other marketed toric contact lenses.
Conclusion
The novel verofilcon A toric lens design demonstrated that it very quickly settles into the proper on-eye position and largely minimizes lens oscillation with blinking. This daily disposable lens offers ECPs and lens wearers a new option for the correction of astigmatism. The rapid settling time, predictable orientation and good fit characteristics of this lens assist the ECP in attaining a fast and accurate toric lens fit.
Acknowledgments
The authors of this study would like to thank the Centre for Ocular Research & Education (CORE) at the University of Waterloo for their contributions to the development of this manuscript.
Funding
This study was funded by Alcon Research, LLC.
Disclosure
Lakshman Subbaraman is an employee of Alcon Inc who manufactures the lens reported in this manuscript. Britt Gustafson, Susan Whaley, Bradley Giedd, Stephen Montaquila, and Brenda Edwards are all optometrists who participated in the clinical trial reported in this manuscript. They received financial compensation for their involvement in this research study from Alcon but the value was insufficient to create bias to influence the results. Susan Whaley also reports personal fees from Johnson & Johnson Vision Care, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Luensmann D, Schaeffer JL, Rumney NJ, et al. Spectacle prescriptions review to determine prevalence of ametropia and coverage of frequent replacement soft toric contact lenses. Cont Lens Anterior Eye. 2018;41(5):412–420. doi:10.1016/j.clae.2018.05.006
2. Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens. 2011;37(1):20–25. doi:10.1097/ICL.0b013e3182048fb9
3. Nichols JJ, Fisher D. Contact lenses 2018. The industry saw slightly higher growth last year due to a continued conversion to daily disposable lenses coupled with a stabilization in patient rebated rates. Contact Lens Spectrum. 2019;34:18–23.
4. Lai N. Take a turn with soft toric lenses for astigmatism. It’s time for practitioners to stop telling patients that they can’t wear contact lenses because of astigmatism. Contact Lens Spectrum. 2019;34:25–28.
5. Dumbleton K, Woods CA, Jones LW, et al. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013;39(1):93–99. doi:10.1097/ICL.0b013e318271caf4
6. Pucker AD, Tichenor AA. A review of contact lens dropout. Clin Optom. 2020;12:85–94. doi:10.2147/OPTO.S198637
7. Sulley A, Young G, Hunt C, et al. Retention rates in new contact lens wearers. Eye Contact Lens. 2018;44(Suppl 1):S273–S282. doi:10.1097/ICL.0000000000000402
8. Craig JP, Willcox MD, Argueso P, et al. The TFOS international workshop on contact lens discomfort: report of the contact lens interactions with the tear film subcommittee. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS123–56. doi:10.1167/iovs.13-13235
9. Chan S, Bickle K, Heinrich C, et al. Clinical subjective performance of two daily disposable soft contact lenses: verofilcon A versus somofilcon A. American Optometric Association Virtual ePoster Session; 2022.
10. Subbaraman L, Gilbert Spear K, Brobst A, et al. Clinical lens fit characteristics of a new silicone hydrogel daily disposable and two commercially available daily disposable contact lenses. Cont Lens Anterior Eye. 2021;44(1):5.
11. Subbaraman L, Tucker B, Leveillee E, et al. Characterizing the surface properties of daily disposable contact lens materials. Cont Lens Anterior Eye. 2021;44:e4. doi:10.1016/j.clae.2020.12.017
12. Mathew J. Importance of rotational stability and tear film stability in toric contact lens wearers [White paper]; 2020.
13. Schulze M, Ng AY, Luensmann D, et al. The subjective response to verofilcon A daily disposable contact lenses during extensive digital device use. Academy at Home; 2020.
14. Miller J, Giedd B, Subbaraman LN. Clinical comparison of a silicone hydrogel and a conventional hydrogel daily disposable contact lens. Clin Ophthalmol. 2021;15:4339–4345. doi:10.2147/OPTH.S332651
15. Fogt JS, Patton K. Long day wear experience with water surface daily disposable contact lenses. Clin Optom. 2022;14:93–99. doi:10.2147/OPTO.S367891
16. Barnett M. Toric lens designs. Contact Lens Spectrum. Newsletter issue April 2018; 2018.
17. Edrington TB. A literature review: the impact of rotational stabilization methods on toric soft contact lens performance. Cont Lens Anterior Eye. 2011;34(3):104–110. doi:10.1016/j.clae.2011.02.001
18. Andrzejewski TM, Pence N. Designs, materials, and fitting of toric silicone hydrogel lenses. A look at what’s available in silicone hydrogel toric lenses as well as fitting tips. Contact Lens Spectrum. 2011;26:32–43.
19. Sulley A, Young G, Lorenz KO, et al. Clinical evaluation of fitting toric soft contact lenses to current non-users. Ophthalmic Physiol Opt. 2013;33(2):94–103. doi:10.1111/opo.12028
20. Straker B, Olivares G, Sulley A. Fitting performance, efficiency and subjective response with a new silicone hydrogel daily disposable toric contact lens. Cont Lens Anterior Eye. 2018;41:S57–S58. doi:10.1016/j.clae.2018.03.049
21. Sulley A, Meyler J. Two unique technologies unite in a new daily lens for astigmatism. Optician. 2010;239(6251):24–27.
22. Tan J, Papas E, Carnt N, et al. Performance standards for toric soft contact lenses. Optom Vis Sci. 2007;84(5):422–428. doi:10.1097/OPX.0b013e318059063b
23. McKinnon C, Tran N, Luensmann D, et al. Consistency and performance of MyDay toric daily disposables. Cont Lens Anterior Eye. 2018;41:S52. doi:10.1016/j.clae.2018.03.030
24. Grzesik M, Sickenberger W, Moest P, et al. Performance evaluation of a toric daily disposable contact lens. Optician. 2005;229(6004):22–24.
25. Morgan PB, Efron SE, Efron N, et al. Inefficacy of aspheric soft contact lenses for the correction of low levels of astigmatism. Optom Vis Sci. 2005;82(9):823–828. doi:10.1097/01.opx.0000177792.62460.58
26. Sonsino J. Comparing two silicone hydrogel toric lenses. Contact Lens Spectrum. 2008;23(9):38–40.
27. McIlraith R, Young G, Hunt C. Toric lens orientation and visual acuity in non-standard conditions. Cont Lens Anterior Eye. 2010;33(1):23–26. doi:10.1016/j.clae.2009.08.003
28. Jones L, Brennan NA, Gonzalez-Meijome J, et al. The TFOS international workshop on contact lens discomfort: report of the contact lens materials, design, and care subcommittee. Invest Ophthalmol Vis Sci. 2013;54(11):TFOS37–70. doi:10.1167/iovs.13-13215
29. Grant T, Tang A. A survey of contact lens wearers and eye care professionals on satisfaction with a new smart-surface silicone hydrogel daily disposable contact lens. Clin Optom. 2020;12:9–15. doi:10.2147/OPTO.S233328
30. Mathew J. Precision1 contact lenses with smartsurface technology [White paper]; 2019.
31. Cummings S, Giedd B, Pearson C. Clinical performance of a novel daily disposable soft contact lens. J Contact Lens Res Sci. 2020;4(2):e23–e30. doi:10.22374/jclrs.v4i1.39
32. Varikooty J, Keir N, Richter D, et al. Comfort response of three silicone hydrogel daily disposable contact lenses. Optom Vis Sci. 2013;90(9):945–953. doi:10.1097/OPX.0b013e31829d8dbf
33. Shi C, Cantu-Crouch D, Sharma V, et al. Characterization of a novel surface modified silicone hydrogel contact lens in fully hydrated environments. Invest Ophthalmol Vis Sci. 2019;60(9):1.
34. International Organization for Standardization. Ophthalmic optics - contact lenses and contact lens care products - guidance for clinical investigations; 2012.
35. Morgan PB, Woods CA, Tranoudis IG, et al. International contact lens prescribing in 2019. Contact Lens Spectrum. 2020;(35):26.
36. Sha J, Fedtke C, Tilia D, et al. Effect of cylinder power and axis changes on vision in astigmatic participants. Clin Optom. 2019;11:27–38. doi:10.2147/OPTO.S190120
37. Hickson-Curran S, Dias L. Toric soft contact lenses: where are we now? Optom Manag. 2005;40(2):83–84, 86–87.
38. Holden BA. Principles and practice of correcting astigmatism with soft contact lenses. Aust J Optom. 1975;58:279–299.
39. Young G, Hunt C, Covey M. Clinical evaluation of factors influencing toric soft contact lens fit. Optom Vis Sci. 2002;79(1):11–19. doi:10.1097/00006324-200201000-00008
40. Zikos GA, Kang SS, Ciuffreda KJ, et al. Rotational stability of toric soft contact lenses during natural viewing conditions. Optom Vis Sci. 2007;84(11):1039–1045. doi:10.1097/OPX.0b013e318159aa3e
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
