Back to Journals » Journal of Inflammation Research » Volume 15
Short- and Mid-Term Survival Prediction in Patients with Acute Type A Aortic Dissection Undergoing Surgical Repair: Based on the Systemic Immune-Inflammation Index
Authors Li Z, Zhang H, Baraghtha S, Mu J, Matniyaz Y, Jiang X, Wang K, Wang D, Xue YX
Received 15 July 2022
Accepted for publication 27 September 2022
Published 10 October 2022 Volume 2022:15 Pages 5785—5799
DOI https://doi.org/10.2147/JIR.S382573
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Zeshi Li,1– 3,* He Zhang,1– 3,* Sulaiman Baraghtha,4,5,* Jiabao Mu,6,* Yusanjan Matniyaz,2 Xinyi Jiang,1– 3 Kuo Wang,2,7 Dongjin Wang,1– 3,7 Yun Xing Xue2
1Department of Cardio-Thoracic Surgery, Nanjing Drum Tower Hospital, Peking Union Medical College & Chinese Academy of Medical Sciences, Graduate School of Peking Union Medical College, Nanjing, People’s Republic of China; 2Department of Cardio-Thoracic Surgery, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing, People’s Republic of China; 3Peking Union Medical College Hospital, Peking Union Medical College & Chinese Academy of Medical Sciences, Beijing, People’s Republic of China; 4Department of Cardio-Thoracic Surgery, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing, People’s Republic of China; 5International School, University of Mannheim, Mannheim, Baden-Württemberg, Federal Republic of Germany; 6School of Data Science, University of Science and Technology of China, Hefei, Anhui, People’s Republic of China; 7Department of Cardio-Thoracic Surgery, Nanjing Drum Tower Hospital, The Affiliated Hospital of XuZhou Medical University, Nanjing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yun Xing Xue; Dongjin Wang, Email [email protected]; [email protected]
Purpose: The postoperative survival of patients with acute type A aortic dissection (aTAAD) remains unsatisfactory. The current study developed an easy-to-use survival prediction model and calculator.
Methods: A total of 496 patients with aTAAD undergoing surgical repair were included in this study. The systemic immune-inflammation index (SII) and other clinical features were collected and subjected to logistic and Cox regression analyses. The survival prediction model was based on Cox regression analyses and exhibited as a nomogram. For convenience of use, the nomogram was further developed into calculator software.
Results: We demonstrated that a higher preoperative SII was associated with in-hospital death (OR: 4.116, p < 0.001) and a higher postoperative overall survival rate (HR: 2.467, p < 0.001) in aTAAD patients undergoing surgical repair. A survival prediction model and calculator based on SII and four other clinical features were developed. The overall C-index of the model was 0.743. The areas under the curves (AUCs) of the 1- and 3-month and 1- and 3-year survival probabilities were 0.73, 0.71, 0.71 and 0.72, respectively. The model also showed good calibration and clinical utility.
Conclusion: Preoperative SII is significantly associated with postoperative survival. Based on SII and other clinical features, we created the first easy-to-use prediction model and calculator for predicting the postoperative survival rate in aTAAD patients, which showed good prediction performance.
Keywords: acute type A aortic dissection, mortality, prediction, systemic immune-inflammation index
Introduction
Acute type-A aortic dissection (aTAAD) is a fatal disease with high mortality.1 Without surgery, the risk of death is 1% to 2% per hour, and 50% of patients die within the first 24 hours after diagnosis. Surgical repair is a life-saving therapy for patients with aTAAD, but the postoperative mortality and prevalence of complications remain high. Multiple databases report that the surgical mortality of these patients ranges from 11% to 25%,2–5 which is still unsatisfactory. Establishing a survival prediction model may help clinicians identify patients at high risk for postoperative death and develop appropriate strategies to improve survival.
Inflammation is related to the pathogenesis and acute stress of aortic dissection.6,7 Immunological-related biomarker changes are observed in the peripheral blood of aTAAD patients, such as white blood cells, C-reactive protein, neutrophils, platelets, and lymphocytes.8–11 Several clinical investigations reported that a high level of inflammatory markers was related to a poor prognosis in aTAAD.10–13 Considering relative small sample size in previous study might be underpowered to confirm the association between elevated inflammation markers and poor outcomes, the true predictive ability of these biomarkers remains controversial. Moreover, we believe that the use of an isolated inflammatory marker might not be competent for predictive outcomes in patients with aTAAD undergoing surgical repair. Because changes in single inflammatory markers might not represent the comprehensive level of the inflammatory response, besides, the neglect of other clinical characteristics of the patient might lead to the prediction model’s lack of accuracy and application value. In our opinion, more representative biomarkers cooperated with more clinical details could be helpful to provide more information for outcomes in patients with aTAAD undergoing surgical repair.
The systemic immune-inflammation index (SII) is a better index of systemic inflammation, and it is based on peripheral lymphocyte (Lym), neutrophil (Ne), and platelet (Plt) counts. Its potential prognostic value has been confirmed in a variety of diseases.14–16 Three recent studies reported that a high SII was associated with short-come mortality and other poor outcomes in aortic dissection.10,17,18 However, there is no study attempt to build a survival prediction model based on SII combined with other clinical information. In our study, we aim to examine the prediction ability of SII in patients with aTAAD undergoing surgical repair and develop a simple prediction model base on SII and other clinical characteristics.
Methods
Patients
This retrospective study enrolled patients who were diagnosed with aTAAD and underwent surgical repair at Nanjing Drum Tower Hospital from January 2016 to December 2018. A total of 496 aTAAD patients undergoing surgical repair were included in our study.
The institutional ethics committee of Nanjing Drum Tower Hospital approved this study. Some of the data were obtained from the database of Jiangsu Commission of Health, and the acquisition of these data required patient authorization. It was not possible to obtain informed consent from all patients. There was no risk to patients in this study. Therefore, the requirement for informed consent was waived by the institutional ethics committee.
The privacy of all medical records and other individually identifiable health information in our study were protected at all times. Information relating to a patient’s health care history, diagnosis, condition, treatment, or evaluation were considered individually identifiable health information. Health information was not used for non-research purposes. This study strictly adhered to the Declaration of Helsinki (seventh revision, 2013)19 and was supervised by the ethics committee.
Surgical Techniques
Combined intravenous–inhalation anesthesia (CIVIA) was commonly used. Routine intraoperative detection included endotracheal intubation, upper and lower extremity arterial puncture monitoring blood pressure, bilateral cerebral oxygen saturation measurement and esophageal ultrasound. Surgical repair was performed via standard median sternotomy, and all patients were cannulated before sternotomy. Right axillary artery and (or) femoral artery cannulation was established directly or through an 8-mm Dacron graft that was anastomosed with the artery. The ascending aorta or aortic arch cannulation under the guidance of esophageal ultrasound was performed in some patients. For venous cannulation, a single venous cannula was placed into the right atrium through the right atrial appendage or superior and inferior vena cava if open-heart surgery was needed. Cardiopulmonary bypass (CPB) was initiated when the whole-blood active clotting time (ACT) was longer than 480 s after heparin infusion, and the patient started to cool to the target temperature. During this period, cold blood cardioplegia was retrogradely perfused routinely through the coronary sinus, then antegrade cardioplegia was administered into the coronary ostia to ensure sufficient cardioprotection. The aortic root and valve were inspected to determine the subsequent root procedure. After reaching the hypothermic circulatory arrest (HCA) temperature, CPB was arrested, and the cerebral tissue was perfused with selected cerebral perfusion (SCP) or retrograde cerebral perfusion (RCP).
The arch was repaired as dictated by the pathology and the surgeon’s preference. For patients with arch dilation (≥45 mm), tears located on the arch and damaged arch structure, total arch replacement with frozen elephant trunk was generally used. Hemi arch replacement or fenestrated arch stent implantation was also selected. Rewarming was started after completion of distal repair. During rewarming, the root procedure and/or supracommissural replacement of the ascending aorta was performed. Generally, supracommissural replacement of the ascending aorta was performed in patients without root involvement and no aortic valve insufficiency. Otherwise, the Bentall procedure or David procedure was performed when root replacement was necessary. The root reconstruction procedure was introduced by our center and called the “double jacket wrapping” technique.20
Data Collection and Definitions
Patient baseline characteristics, laboratory features, operative details, and outcome data were obtained from our electronic medical record database. Follow-up data were assessed from the last medical records or telephone interviews. The complete blood count was collected after admission and analyzed immediately in an auto hematology analyzer (BC-6800Plus, Mindray, China). The last analysis report before surgery was selected when multiple blood samples had been tested.
The SII was calculated using the following formula: SII = platelet count (Plt) × neutrophil to lymphocyte ratio (N/L) (SII = P × N/L ratio). Diagnosis and classification were established using contrast-enhanced computed tomography or magnetic resonance imaging and confirmed during surgery. The type of aortic dissection was defined according to the Stanford classification.21 Acute dissection was defined as symptom onset within 14 days before medical admissions. Limb ischemia was defined as a diminished pulse or pulselessness with pain, pallor, paresthesia, poikilothermia, or paralysis at the involved extremity.22 Isolated radiographic evidence of compromised blood flow in the extremity was not considered limb ischemia.
Statistical Analysis
Statistical analyses were performed using SPSS version 28.0 (IBM, USA) and R version 4.2.1. Continuous variables were compared using Student’s t-test or the Mann–Whitney U-test, and the results are presented as means with standard deviation or medians with interquartile range. The categorical variables were compared using the chi-squared test or Fisher’s exact test and are presented as frequencies with percentages. The receiver operating characteristic (ROC) curve and Youden index23 were used to explore the predictive value of SII for in-hospital death. The formula of the Youden index was sensitivity + specificity – 1. The SII value corresponding to the maximum value of the Youden index was selected as the cut-off point.
Logistic and Cox regression analyses were used to examine the independent risk factors for in-hospital death and postoperative survival. Variables with p < 0.1 in the univariate analysis or that were thought to be important were selected for the multivariate analysis. The Enter method was used to determine independent risk factors in the multivariate analysis. The Kaplan-Meier (KM) method and Log rank test were performed to analyze postoperative survival. The nomogram was constructed using the ‘rms’ R package. The prediction accuracy of the nomogram was tested using the concordance index (C-index) and time-dependent receiver operating characteristic curves with areas under the curves (AUCs). The calibration curve was used to determine consistency between the predicted survival probability of the nomogram with bootstrap resamples. Decision curve analysis (DCA) was used to evaluate the net benefit of the nomogram. Two-sided P <0.05 was considered statistically significant.
Results
Baseline Characteristics
A total of 496 aTAAD patients undergoing surgical repair were included in our retrospective cohort (Figure 1). There were 366 (73.79%) males, and the average age of the patients was 53.61 ± 14.13 years. A total of 379 (76.41%) patients had hypertension. A total of 495 (99.80%) patients received ascending aorta replacement. The most common root surgery option was root reconstruction using the “Double Jacket Wrapping” technique (53.23%), and the most common arch surgery option was total arch replacement with frozen elephant trunk (48.99%). ROC curve analysis was used to examine the predictive value of the preoperative SII for in-hospital death. The area under the curve (AUC) was 0.61 (95% CI, 0.70–0.53) (Figure 2). The optimal cut-off value was 3324.5. Patients were divided into two groups by the cut-off value: SII<3324.5 group (n = 405, 81.65%) and SII≥3324.5 group (n = 91, 18.35%). The baseline characteristics of the two groups are shown in Table 1. Patients in the SII<3324.5 group had higher proportions of cerebral ischemia (40, 9.88% vs 3, 3.30%, p = 0.044) and coronary artery involvement (66, 16.30% vs 25, 25.47%, p = 0.013). The WBC, neutrophil and platelet counts were significantly higher in the SII≥3324.5 group (14.46 ± 3.85×10*9/L vs 11.97 ± 3.89×10*9/L, p<0.001; 13.42 ± 5.55×10*9/L vs 10.16 ± 3.33×10*9/L, p<0.001; 177.00 ± 51.43×10*9/L vs 145.09 ± 60.37×10*9/L, p<0.001). The SII<3324.5 group had higher albumin and lymphocyte counts (38.09 ± 3.19 vs 37.86 ± 3.26, p = 0.044), [0.94 (0.60, 1.20) vs 0.60 (0.40, 0.70), p<0.001]. There were no significant differences in other biomarkers or clinical details between the two groups.
 |
Table 1 Baseline Characteristics |
 |
Figure 1 Flowchart of participant selection. |
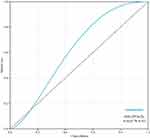 |
Figure 2 Receiver operating characteristic curve (ROC) analysis with the area under the curve, sensitivity and specificity of systemic immune-inflammation index (SII) in predicting in-hospital death. |
Short and Mid-Term Outcomes
Patients’ short- and mid-term outcomes are shown in Table 2. A total of 70 (14.11%) patients died (all-cause deaths) in the hospital. Patients in the SII≥3324.5 group had higher short-term mortality (30, 32.97% vs 40, 9.88%, p<0.001) and postoperative bowel ischemia (5, 5.49% vs 4, 0.99%, p=0.004). Other short-term outcomes, such as reintubation, intracranial hemorrhage, stroke, paraplegia, acute renal failure (ARF), use of continuous renal replacement therapy (CRRT), gastrointestinal (GI) bleeding, and surgical site infection, were similar between the two groups. During a median follow-up period of 23.52 (15.20, 34.23) months, the overall mid-term mortality (all-cause deaths) was 4.38% in the SII<3324.5 group and 4.92% in the SII≥3324.5 group (P=0.852).Six (9.84%) patients in the SII≥3324.5 group needed reintervention, which was similar to the SII<3324.5 group (P = 0.842). The Kaplan–Meier curves showed that the overall survival was significantly different between the two groups (HR: 0.32; 95% CI: 0.21–0.49, p<0.001) (Figure 3).
 |
Table 2 Short- and Mid-Term Outcomes |
 |
Figure 3 Kaplan-Meier survival curve analysis and Log rank test. |
Logistic Regression Analyses and Cox Regression Analyses
We used logistic regression methods to further analyze the independent risk factors for in-hospital deaths for patients with aTAAD undergoing surgical repair. The results of univariate and multivariable logistic regression analyses are shown in Table 3. Univariate logistic regression analyses showed that coronary artery involvement, concomitant CABG, SII≥3324.5, albumin, WBC count, cardiopulmonary bypass (CPB) time, cross-clamp time and neutrophils were potential risk factors for in-hospital deaths. Multivariable logistic analyses showed that SII≥3324.5 was an independent risk factor for in-hospital death (OR: 4.116; 95% CI: 1.13–2.47, p < 0.001, Table 3).
 |
Table 3 Univariate and Multivariable Logistic Regression Analyses of Clinical Parameters |
Cox regression analyses were used to determine the independent predictors of the overall survival rate after surgical repair. SII≥3324.5 and sex, age > 70, hypertension, diabetes mellitus, CAD, COPD, ESRD, preoperative cerebral ischemia, preoperative limb ischemia, preoperative bowel ischemia, postoperative CRRT use, coronary artery involvement, concomitant CABG, CPB time and cross-clamp time were analyzed using univariate Cox regression analyses. Variables with p < 0.1 in the univariate analyses were included in the multivariate analyses. The results showed that SII≥3324.5 (HR: 2.467; 95% CI: 1.573–3.868, p < 0.001, Table 4), age≥70, preoperative limb ischemia, postoperative CRRT use, and concomitant CABG were independent risk factors for the overall survival rate after surgical repair.
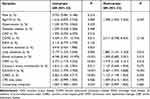 |
Table 4 Univariate and Multivariable Cox Regression Analyses of Clinical Parameters |
Survival Prediction Model and Calculator
To quantitatively predict the survival of patients with aTAAD undergoing surgical repair, we established a nomogram including significant indicators for the overall survival rate (Figure 4). This nomogram showed that the preoperative SII contributed the most to the prognosis, followed by postoperative CRRT use, preoperative limb ischemia, concomitant CABG and age. All of these variables were assigned a score on the points scale. Summation over The variable points were summed, and a total point was obtained and located on the Total Points scale. A line was drawn straight down to the 1-/3-month and 1-/3-year survival probability scales, and the estimated survival probability at each time point is shown.
 |
Figure 4 Nomogram for predicting 1-/3- month and 1-/3- year survival of patients with aTAAD undergoing surgical repair. |
The accuracy of the nomogram was examined. The overall C-index of the nomogram was 0.743 (95% CI: 0.691–0.797, p < 0.001). Time-dependent ROC with AUCs were also used to assess the predictive accuracy of the nomogram. Our model showed good prediction ability in overall survival rate in each time point, as reflected by the AUC of 1-/3- month and 1-/3- year survival probability was 0.73 (95% CI: 0.66–0.79), 0.71 (95% CI: 0.65–0.78), 0.71 (95% CI: 0.65–0.78), 0.72 (95% CI: 0.64–0.79) respectively (Figure 5). The calibration plots showed good consistency between the nomogram predictions and actual observations for the overall survival rate at each time point (Figure 6). Decision curve analysis (DCA) curves were used to examine the clinical usefulness of our model. The results showed good clinical applicability of our model in predicting the 1-/3-month and 1-/3-year survival probability of patients with aTAAD undergoing surgical repair. (Figure 7).
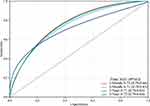 |
Figure 5 Time-independent ROC curves of the nomogram for 1-/3- month and 1-/3- year survival prediction. |
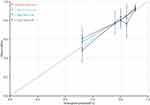 |
Figure 6 Calibration plots of the nomogram for 1-/3- month and 1-/3- year survival prediction. |
 |
Figure 7 DCA of the nomogram for 1-/3- month and 1-/3- year survival prediction (A–D). |
To make our predictive model more convenient for clinicians to use in practice, we developed a calculator based on the nomogram. This calculator was developed in the C# language and may be used on any computer that has the.NET platform. The estimated survival probability across time may be easily shown by inputting and choosing clinical features for the calculator. The calculator version 1.0 was implemented and may be downloaded at https://github.com/GitttttMuMu/calculator.
Discussion
The present study investigated the relationship between the preoperative SII and in-hospital death and postoperative overall survival rates in aTAAD patients undergoing surgical repair. We developed a survival prediction model and a compact calculator based on the SII and other clinical features. Our survival model and calculator provide a useful and simple tool for risk stratification of aTAAD patients undergoing surgical repair.
Acute type A aortic dissection is a life-threatening condition caused by an intimal tear in the aorta that creates a false lumen between the intimal and middle layers of the aortic wall in the ascending aorta.24 Based on the evidences, all patients with aTAAD should be treated by surgery.25 Although mortality after surgical repair has improved over the past decades,26,27 but according to reports from multicenters studies around the world, postoperative mortality still reach up to 11–25%.2–5 Mid- and long-term survival rate of surviving patients was 85% and 68%.28–32 In clinical practice, estimations of an aTAAD patient’s postoperative survival rate often rely on the clinician’s experience. This assessment method lacks accredited standards and cannot provide more precise information to support decision-making. Therefore, the creation of an effective tool to quantitatively improve assessment survival would be helpful for risk stratification and decision-making.
Two previous studies tried to achieve this goal. Sergey Leontyev et al used age, critical preoperative state, and malperfusion syndrome to create an easy-to-use scorecard to predict in-hospital death for patients with aTAAD.33 Martin Czerny et al created the GERAADA score to predict the 30-day mortality rate for patients with aTAAD undergoing surgery and developed a web-based application.34 However, there were some deficiencies in these two studies. First, the evaluation of these preoperative indicators was relatively complex and may be susceptible to subjective factors. Therefore, standard evaluation criteria may be difficult to apply. Second, only the preoperative variables were used in the prediction models in both studies, and there may be unmeasured perioperative confounders that were not accounted for in their analyses. Third, only two-thirds of patients were alive at three years if they survived the initial hospitalization,30 which provides a method of predicting mid-term survival rates that may benefit postoperative treatment and mid-term outcomes. Unfortunately, both models only predicted a short-term survival rate after surgery.
The immune-inflammatory mechanisms that occur in aortic dissection give us ideas to solve the above problems. The main histopathologic change in aTAAD is arterial wall weakening caused by medial degeneration, which consists of degradation of the extracellular matrix (ECM) related to smooth muscle cell (SMC) depletion, elastic fiber fragmentation, and collagen degradation, and immune-inflammatory mechanisms have been proven contribute greatly to aortic wall remodel.35,36 Inflammatory cells have been indicated that are present in the aortic media in aortic dissection, which contribute to smooth muscle cell apoptosis through activation of death-promoting pathways.37,38 What we were most interested in was the systemic inflammatory reaction induced by aTAAD. Although the etiological backgrounds of the systemic inflammatory reaction remain to be clarified, multiple evidences have demonstrated that more intensive systemic Inflammation might be related to unfavorable short-term or mid-term outcomes in patients with aTAAD.9,39–42
The systemic immune-inflammation index (SII) is a novel biomarker to assess patients’ inflammatory and immune status quantitatively. SII is calculated as Platelets count (Plt) × Neutrophil to-Lymphocyte ratio (N/L) (SII = P × N/L ratio). In previous studies, higher SII was associated with poor outcomes in patients with various cancers and had the ability to predict mid-term outcomes.43–45 Platelets, neutrophils, and lymphocytes have an important function in the inflammatory state. False lumen blood flow and tearing vascular tissue surface are powerful activators of the platelets.46 Platelet activation was seen as the “first stress response” in the pathogenesis of aTAAD.47 During this process, activated and aggregated platelets could release inflammatory factors into the blood, which could activate neutrophils and monocytes, promote lymphocyte migration to peripheral lymph nodes, further promote platelet adhesion, aggregation, and break the balance between coagulation and fibrinolytic systems.48,49 Activated neutrophils could release proteolytic enzymes, arachidonic-acid derivatives, and reactive oxygen intermediate, increasing vascular endothelial damage.50 In addition, the interplay between platelets and neutrophils could enhance neutrophil functions, which play an important role in inflammatory responses.51 As opposed to activation of neutrophils representing active inflammation, lymphocyte variation reflects overall physiological stress.52 Lymphopenia was proven to has relevant to poor outcomes in many cardiovascular disease.53–55 As a compositive index, SII combines different biomarkers across the pathobiological axes of system inflammatory response. Thus, we believe that SII could serve as a potential tool for risk stratification for aTAAD patients. Xu et al reported that SII could predict postoperative short-term adverse outcomes in aTAAD patients after surgery.18 Another retrospective study reported that SII is associated with in-hospital and mid-term survival in patients with type B aortic dissection undergoing thoracic endovascular repair.17 Our study also identified similar results. In our study, we demonstrated that high preoperative SII was related to in-hospital death in patients with aTAAD undergoing surgical repair. Furthermore, Kaplan–Meier analysis and multivariable Cox analysis illustrated that high preoperative SII was related to higher short-term and mid-term mortality rates in such patients.
An elevated preoperative SII may represent a special subset of aTAAD patients who are at greater risk of mortality after surgery. In addition, other high-risk factors should not be neglected. In the present study, by using Cox analysis, we identified four other perioperative major independent predictors of depressed postoperative survival: age ≥ 70, preoperative limb ischemia, postoperative CRRT use, and concomitant CABG. Previous studies showed a significant effect of advanced age on mortality and complication rate.56,57 The significantly higher mortality might attribute to more comorbidities before surgery in old patients.56 Peripheral vascular complications were a powerful risk factor for increased postoperative mortality of patients with aTAAD.58 We found that only the preoperative limb ischemia was the independent risk factor of increased postoperative mortality in such peripheral vascular complications. Besides, some studies declared that they found no association between preoperative limb (or extremity) ischemia and poor outcomes,59,60 reported conflicting results with our study. Our findings could be explained by “delayed intervention” because the interval between symptoms onset to definitive diagnosis was significantly longer at our center compared with Massachusetts General Hospital.61 Thus, our patients who were considered with preoperative limb ischemia might actually be more critical because of the primary care and referral systems’ heterogeneity between the United States and China. Moreover, the first and most commonly used method of assessing preoperative limb ischemia is diminished pulses in our clinical practice. This simple method itself has been reported to be useful for identifying a high-risk subgroup of aTAAD patients.62 Therefore, we chose preoperative limb ischemia as a significant independent predictor for the prediction model was reasonable. Evidence from the previous studies reported the incidence of postoperative CRRT use in patients undergoing surgery with aTAAD was 11–27%, and the mortality in such patients was significantly higher than in patients who were not.63–65 Our study confirmed these phenomena. We performed concomitant CABG in two clinical scenarios, type B and type C coronary artery involvement clarified via intraoperative exploration66 and difficult CPB weaning considered to be related to insufficient coronary artery blood flow. This results in most concomitant CABG being unscheduled and rescued. Concomitant CABG significantly prolongs ACC time and CPB time, which leads to an increase in myocardial ischemia period and inflammatory response.67 At the same time, although concomitant CABG was one of the few ways to save patients, it also might expose surviving patients to the potential risks of CABG. Results from two studies supported these theories effectively.67,68 To sum it up, both postoperative CRRT use and concomitant CABG were considered independent risk factors of mortality in aTAAD patients undergoing surgical repair.
Based on results from Cox analysis, we built a survival prediction model for patients with aTAAD undergoing surgical repair. This model was constructed by combining preoperative SII, age, preoperative limb ischemia, postoperative CRRT use, and concomitant CABG. Our model was plotted as a nomogram. The overall C-index of the nomogram was 0.743 (95% CI: 0.691–0.797, p < 0.001). Furthermore, our model showed good prediction ability in overall survival rate at each time point, as reflected by the AUC of 1-/3- month and 1-/3- year survival probability was 0.73 (95% CI: 0.66–0.79), 0.71 (95% CI: 0.65–0.78), 0.71 (95% CI: 0.65–0.78), 0.72 (95% CI: 0.64–0.79) respectively. The calibration and clinical utility of the model were also good. In addition, we developed a calculator based on the nomogram.
The advantages of the present model and calculator are as follows. First, we introduced the SII to reflect the compositive preoperative state of patients, which greater simplified and increased the standardization of the assessment, especially beneficial to non-cardiothoracic surgeons and physicians. Second, we also introduced the perioperative risk factors, which could reflect the variation and actual condition of the patient during the clinical treatment process. In practical using, our model and calculator could implement the dynamic evaluation at different key points in hospitalization. Third, to our knowledge, the present study provided the first assessment method for short- and mid-term survival prediction in patients with aTAAD undergoing surgical repair. Based on the above advantages, our model has optimistic clinical implications. In addition to predicting a clinical outcome, our model will help identifying patients who in the highest risk category. If a high risk patient has a very low estimated survival rate, the alternate therapeutic schedule such as endovascular techniques or more conservative surgical strategies could be considered to improving short-term survival as much as possible. With the exception of assisting decision-making in emergency situations, our model can assist clinical decision-making in the rehabilitation of surviving patients, as well as guide the allocation of healthcare resources and reduce costs. But what needs to be emphasized is our model was not designed to help clinicians determine whether the life-saving surgical intervention was required.
Limitations
The present study was not exempt from limitations. First, this study was a retrospective study, which makes it susceptible to selection bias. It was difficult to evaluate all patients who were not diagnosed or referred to our center with aTAAD during the study start and end times. However, it is an inevitable limitation that has plagued all correlative studies. Second, this study was based on data from a single center. Whether the results of the study are applicable to other centers requires further testing. One preoperative measurement of routine blood tests may not represent an individual’s actual state before surgery. Changes in patients’ condition may have occurred between the blood draw and surgery, which lacks adjusted SII variance over the perioperative period and was not dynamically monitored in this study.
Conclusions
The surgical repair of patients with aTAAD remains a challenge, and the postoperative survival rate is not satisfactory. We provide evidence that the preoperative SII is significantly associated with postoperative survival. Based on the SII in combination with other clinical features, we created the first easy-to-use prediction model and calculator for predicting the postoperative survival rate of these patients, which showed good accuracy and applicability. We recommend the conventional application of this tool for assisting clinical decision-making in aTAAD patients undergoing surgical repair throughout their treatment process.
Supplementary Materials
Supplementary material associated with this article can be found, in the online version, at https://github.com/GitttttMuMu/calculator.
Funding
This work was supported by the National Natural Science Foundation of China (no. 81970401, no. 82100508), Jiangsu Provincial Key Medical Discipline (ZDXKA 2016019) and General project of Nanjing Health Commission (Grant No. YKK21087).
Disclosure
The authors have declared that no conflict of interest exists.
References
1. Evangelista A, Isselbacher EM, Bossone E, et al. Insights from the international registry of acute aortic dissection: a 20-year experience of collaborative clinical research. Circulation. 2018;137(17):1846–1860. doi:10.1161/CIRCULATIONAHA.117.031264
2. Inoue Y, Matsuda H, Uchida K, et al. Analysis of acute type A aortic dissection in Japan Registry of Aortic Dissection (JRAD). Ann Thorac Surg. 2020;110(3):790–798. doi:10.1016/j.athoracsur.2019.12.051
3. Lee TC, Kon Z, Cheema FH, et al. Contemporary management and outcomes of acute type A aortic dissection: an analysis of the STS adult cardiac surgery database. J Cardiac Surg. 2018;33(1):7–18. doi:10.1111/jocs.13511
4. Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of acute aortic dissection. J Am Coll Cardiol. 2015;66(4):350–358. doi:10.1016/j.jacc.2015.05.029
5. Chemtob RA, Fuglsang S, Geirsson A, et al. Stroke in acute type A aortic dissection: the Nordic Consortium for Acute Type A Aortic Dissection (NORCAAD). Eur J Cardio Thorac. 2020;58(5):1027–1034. doi:10.1093/ejcts/ezaa197
6. Del Porto F, Proietta M, Tritapepe L, et al. Inflammation and immune response in acute aortic dissection. Ann Med. 2010;42(8):622–629. doi:10.3109/07853890.2010.518156
7. Cifani N, Proietta M, Tritapepe L, et al. Stanford-A acute aortic dissection, inflammation, and metalloproteinases: a review. Ann Med. 2015;47(6):441–446. doi:10.3109/07853890.2015.1073346
8. Forrer A, Schoenrath F, Torzewski M, et al. Novel blood biomarkers for a diagnostic workup of acute aortic dissection. Diagnostics. 2021;11(4):615. doi:10.3390/diagnostics11040615
9. Suzuki K, Kimura N, Mieno M, et al. Factors related to white blood cell elevation in acute type A aortic dissection. PLoS One. 2020;15(2):e228954. doi:10.1371/journal.pone.0228954
10. Li M, Xu S, Yan Y, et al. Association of biomarkers related to preoperative inflammatory and coagulation with postoperative in-hospital deaths in patients with type A acute aortic dissection. Sci Rep. 2021;11(1):18775. doi:10.1038/s41598-021-98298-w
11. Erdolu B, As AK. C-reactive protein and neutrophil to lymphocyte ratio values in predicting inhospital death in patients with Stanford type A acute aortic dissection. Heart Surg Forum. 2020;23(4):E488–E492. doi:10.1532/hsf.3055
12. Ma M, Shi J, Feng X, Wang J, Liu L, Wei X. The elevated admission white blood cell count relates to adverse surgical outcome of acute Stanford type a aortic dissection. J Cardiothorac Surg. 2020;15(1):48. doi:10.1186/s13019-020-1078-5
13. Chen Z, Huang B, Lu H, et al. Admission white blood cell count predicts short-term clinical outcomes in patients with uncomplicated Stanford type B acute aortic dissection. J Geriatr Cardiol. 2017;14(1):49–56. doi:10.11909/j.issn.1671-5411.2017.01.011
14. Lei H, Xu S, Mao X, et al. Systemic immune-inflammatory index as a predictor of lymph node metastasis in endometrial cancer. J Inflamm Res. 2021;14:7131–7142. doi:10.2147/JIR.S345790
15. Wang Q, Zhu D. The prognostic value of systemic immune-inflammation index (SII) in patients after radical operation for carcinoma of stomach in gastric cancer. J Gastrointest Oncol. 2019;10(5):965–978. doi:10.21037/jgo.2019.05.03
16. Yang Y, Wu C, Hsu P, et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest. 2020;50(5):e13230. doi:10.1111/eci.13230
17. Su S, Liu J, Chen L, et al. Systemic immune-inflammation index predicted the clinical outcome in patients with type-B aortic dissection undergoing thoracic endovascular repair. Eur J Clin Invest. 2022;52(2):e13692. doi:10.1111/eci.13692
18. Xu H, Li Y, Wang H, et al. Systemic immune-inflammation index predicted short-term outcomes in ATAD patients undergoing surgery. J Cardiac Surg. 2022;37(4):969–975. doi:10.1111/jocs.16300
19. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):992–994.
20. Xue Y, Zhou Q, Pan J, et al. ”Double Jacket Wrapping” root reconstruction for acute type A aortic dissection. Ann Thorac Surg. 2020;110(3):1060–1062. doi:10.1016/j.athoracsur.2020.03.081
21. Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thorac Surg. 1970;10(3):237–247. doi:10.1016/S0003-4975(10)65594-4
22. Obara H, Matsubara K, Kitagawa Y. Acute limb ischemia. Ann Vasc Dis. 2018;11(4):443–448. doi:10.3400/avd.ra.18-00074
23. Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35.
24. Elsayed RS, Cohen RG, Fleischman F, Bowdish ME. Acute type A aortic dissection. Cardiol Clin. 2017;35(3):331–345. doi:10.1016/j.ccl.2017.03.004
25. Erbel R, Aboyans V, Boileau C, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(41):2873–2926. doi:10.1093/eurheartj/ehu281
26. Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897–903. doi:10.1001/jama.283.7.897
27. Zhu Y, Lingala B, Baiocchi M, et al. Type A aortic dissection-experience over 5 decades: JACC historical breakthroughs in perspective. J Am Coll Cardiol. 2020;76(14):1703–1713. doi:10.1016/j.jacc.2020.07.061
28. Chiappini B, Schepens M, Tan E, et al. Early and late outcomes of acute type A aortic dissection: analysis of risk factors in 487 consecutive patients. Eur Heart J. 2005;26(2):180–186. doi:10.1093/eurheartj/ehi024
29. Trimarchi S, Nienaber CA, Rampoldi V, et al. Contemporary results of surgery in acute type A aortic dissection: the international registry of acute aortic dissection experience. J Thorac Cardiovasc Surg. 2005;129(1):112–122. doi:10.1016/j.jtcvs.2004.09.005
30. Tsai TT, Evangelista A, Nienaber CA, et al. Long-term survival in patients presenting with type A acute aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation. 2006;114(1 Suppl):I350–I356. doi:10.1161/CIRCULATIONAHA.105.000497
31. Pan E, Gudbjartsson T, Ahlsson A, et al. Low rate of reoperations after acute type A aortic dissection repair from The Nordic Consortium Registry. J Thorac Cardiovasc Surg. 2018;156(3):939–948. doi:10.1016/j.jtcvs.2018.03.144
32. Olsson C, Ahlsson A, Fuglsang S, et al. Medium-term survival after surgery for acute type A aortic dissection is improving. Eur J Cardiothorac Surg. 2017;52(5):852–857. doi:10.1093/ejcts/ezx302
33. Leontyev S, Légaré J, Borger MA, et al. Creation of a scorecard to predict in-hospital death in patients undergoing operations for acute type A aortic dissection. Ann Thorac Surg. 2016;101(5):1700–1706. doi:10.1016/j.athoracsur.2015.10.038
34. Czerny M, Siepe M, Beyersdorf F, et al. Prediction of mortality rate in acute type A dissection: the German registry for acute type A aortic dissection score. Eur J Cardiothorac Surg. 2020;58(4):700–706. doi:10.1093/ejcts/ezaa156
35. Wu D, Shen YH, Russell L, Coselli JS, LeMaire SA. Molecular mechanisms of thoracic aortic dissection. J Surg Res. 2013;184(2):907–924. doi:10.1016/j.jss.2013.06.007
36. Didangelos A, Yin X, Mandal K, et al. Extracellular matrix composition and remodeling in human abdominal aortic aneurysms: a proteomics approach. Mol Cell Proteomics. 2011;10(8):M111–M8128. doi:10.1074/mcp.M111.008128
37. Jia L, Zhang W, Zhang H, et al. Mechanical stretch-induced endoplasmic reticulum stress, apoptosis and inflammation contribute to thoracic aortic aneurysm and dissection. J Pathol. 2015;236(3):373–383. doi:10.1002/path.4534
38. He R, Guo D, Estrera AL, et al. Characterization of the inflammatory and apoptotic cells in the aortas of patients with ascending thoracic aortic aneurysms and dissections. J Thorac Cardiovasc Surg. 2006;131(3):671–678. doi:10.1016/j.jtcvs.2005.09.018
39. Xu Y, Fang H, Qiu Z, Cheng X. Prognostic role of neutrophil-to-lymphocyte ratio in aortic disease: a meta-analysis of observational studies. J Cardiothorac Surg. 2020;15(1):215. doi:10.1186/s13019-020-01263-3
40. Kalkan ME, Kalkan AK, Gündeş A, et al. Neutrophil to lymphocyte ratio: a novel marker for predicting hospital mortality of patients with acute type A aortic dissection. Perfusion. 2017;32(4):321–327. doi:10.1177/0267659115590625
41. Zhang R, Chen S, Zhang H, et al. Biomarkers investigation for in-hospital death in patients with Stanford type A acute aortic dissection. Int Heart J. 2016;57(5):622–626. doi:10.1536/ihj.15-484
42. Mori K, Tamune H, Tanaka H, Nakamura M. Admission values of D-dimer and C-reactive protein (CRP) predict the long-term outcomes in acute aortic dissection. Intern Med. 2016;55(14):1837–1843. doi:10.2169/internalmedicine.55.6404
43. Huang H, Liu Q, Zhu L, et al. Prognostic value of preoperative systemic immune-inflammation index in patients with cervical cancer. Sci Rep. 2019;9(1):3284. doi:10.1038/s41598-019-39150-0
44. Hu B, Yang X, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–6222. doi:10.1158/1078-0432.CCR-14-0442
45. Albany C. Systemic immune-inflammation index in germ-cell tumours: search for a biological prognostic biomarker. Brit J Cancer. 2018;118(6):761–762. doi:10.1038/bjc.2018.7
46. Paparella D, Rotunno C, Guida P, et al. Hemostasis alterations in patients with acute aortic dissection. Ann Thorac Surg. 2011;91(5):1364–1369. doi:10.1016/j.athoracsur.2011.01.058
47. Chen Y, Lin Y, Zhang H, Peng Y, Li S, Huang X. Relationship of platelet counts and inflammatory markers to 30-day mortality risk in patients with acute type A aortic dissection. Biomed Res Int. 2020;2020:1–7.
48. Thomas MR, Storey RF. The role of platelets in inflammation. Thromb Haemostasis. 2015;114(3):449–458. doi:10.1160/TH14-12-1067
49. Totani L, Evangelista V. Platelet-leukocyte interactions in cardiovascular disease and beyond. Arterioscler Thromb Vasc Biol. 2010;30(12):2357–2361. doi:10.1161/ATVBAHA.110.207480
50. Lisman T. Platelet-neutrophil interactions as drivers of inflammatory and thrombotic disease. Cell Tissue Res. 2018;371(3):567–576. doi:10.1007/s00441-017-2727-4
51. Li J, Kim K, Barazia A, Tseng A, Cho J. Platelet-neutrophil interactions under thromboinflammatory conditions. Cell Mol Life Sci. 2015;72(14):2627–2643. doi:10.1007/s00018-015-1845-y
52. Bhat TM, Afari ME, Garcia LA. Neutrophil lymphocyte ratio in peripheral vascular disease: a review. Expert Rev Cardiovasc Ther. 2016;14(7):871–875. doi:10.1586/14779072.2016.1165091
53. Majmundar M, Kansara T, Park H, et al. Absolute lymphocyte count as a predictor of mortality and readmission in heart failure hospitalization. IJC Heart Vasculature. 2022;39:100981. doi:10.1016/j.ijcha.2022.100981
54. Giede-Jeppe A, Bobinger T, Gerner ST, et al. Lymphocytopenia is an independent predictor of unfavorable functional outcome in spontaneous intracerebral hemorrhage. Stroke. 2016;47(5):1239–1246. doi:10.1161/STROKEAHA.116.013003
55. Ommen SR, Hodge DO, Rodeheffer RJ, McGregor CG, Thomson SP, Gibbons RJ. Predictive power of the relative lymphocyte concentration in patients with advanced heart failure. Circulation. 1998;97(1):19–22. doi:10.1161/01.CIR.97.1.19
56. Wang J, Xue Y, Zhu X, et al. The impact of age in acute type A aortic dissection: a retrospective study. J Cardiothorac Surg. 2022;17(1):40. doi:10.1186/s13019-022-01785-y
57. Trimarchi S, Eagle KA, Nienaber CA, et al. Role of age in acute type A aortic dissection outcome: report from the International Registry of Acute Aortic Dissection (IRAD). J Thorac Cardiovasc Surg. 2010;140:784–789. doi:10.1016/j.jtcvs.2009.11.014
58. Fann JI, Sarris GE, Mitchell RS, et al. Treatment of patients with aortic dissection presenting with peripheral vascular complications. Ann Surg. 1990;212(6):705–713. doi:10.1097/00000658-199012000-00009
59. Kristofer MC, Kaji S, Samuel SL, et al. Management of limb ischemia in acute proximal aortic dissection. J Vasc Surg. 2013;57(4):1023–1029. doi:10.1016/j.jvs.2012.10.079
60. Beck CJ, Germano E, Artis AS, et al. Outcomes and role of peripheral revascularization in type A aortic dissection presenting with acute lower extremity ischemia. J Vasc Surg. 2022;75(2):495–503. doi:10.1016/j.jvs.2021.08.050
61. Axtell AL, Xue Y, Qu JZ, et al. Type A aortic dissection in the East and West: a comparative study between two hospitals from China and the US. J Cardiac Surg. 2020;35(9):2168–2174. doi:10.1111/jocs.14766
62. Eduardo B, Vincenzo R, Christoph AN, et al. Usefulness of pulse deficit to predict in-hospital complications and mortality in patients with acute type A aortic dissection. Am J Cardiol. 2002;89(7):513–562, 65, 130–154.
63. Chen X, Zhou J, Fang M, et al. Incidence- and in-hospital mortality-related risk factors of acute kidney injury requiring continuous renal replacement therapy in patients undergoing surgery for acute type A aortic dissection. Front Cardiovasc Med. 2021;8:749592. doi:10.3389/fcvm.2021.749592
64. Helgason D, Helgadottir S, Ahlsson A, et al. Acute kidney injury after acute repair of type A aortic dissection. Ann Thorac Surg. 2021;111(4):1292–1298. doi:10.1016/j.athoracsur.2020.07.019
65. Rice RD, Sandhu HK, Leake SS, et al. Is total arch replacement associated with worse outcomes during repair of acute type A aortic dissection? Ann Thorac Surg. 2015;100(6):2159–2165, 2165–2166. doi:10.1016/j.athoracsur.2015.06.007
66. Neri E, Toscano T, Papalia U, et al. Proximal aortic dissection with coronary malperfusion: presentation, management, and outcome. J Thorac Cardiovasc Surg. 2001;121(3):552–560. doi:10.1067/mtc.2001.112534
67. Zhang K, Dong S, Pan X, et al. Concomitant coronary artery bypass grafting during surgical repair of acute type A aortic dissection affects operative mortality rather than midterm mortality. Asian J Surg. 2021;44(7):945–951. doi:10.1016/j.asjsur.2021.01.031
68. Imoto K, Uchida K, Karube N, et al. Risk analysis and improvement of strategies in patients who have acute type A aortic dissection with coronary artery dissection. Eur J Cardio Thorac Surg. 2013;44(3):419–424, 424–425. doi:10.1093/ejcts/ezt060
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
