Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 12
Shear Bond Strength of Bulk-Fill Composites to Resin-Modified Glass Ionomer Evaluated by Different Adhesion Protocols
Authors Bin-Shuwaish MS
Received 24 July 2020
Accepted for publication 27 August 2020
Published 16 September 2020 Volume 2020:12 Pages 367—375
DOI https://doi.org/10.2147/CCIDE.S273842
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Christopher E. Okunseri
Mohammed S Bin-Shuwaish
Department of Restorative Dental Sciences, College of Dentistry, King Saud University, Riyadh, Kingdom of Saudi Arabia
Correspondence: Mohammed S Bin-Shuwaish
Department of Restorative Dental Sciences, College of Dentistry, King Saud University, Kingdom of Saudi Arabia
Tel +966-11-467-7420
Email [email protected]
Objective: The aim of this study was to investigate the shear bond strengths (SBS) of different nano-resin-based composites (RBCs) to resin-modified glass-ionomer cement (RMGIC) after the application of different adhesion protocols.
Material and Methods: Three RBCs (Filtek One Bulk Fill [FOBF], Tetric N-Ceram Bulk Fill [TNCBF], and Filtek Z350 XT [Z350XT]) were used as layering materials over GC Fuji II LC RMGIC. Three adhesive systems — Total-etch (OptiBond Solo Plus [OB]), self-etch (CLEAR FIL SE Bond 2 [CFSE]), and a universal bond (Single Bond Universal [SBU]) — were used. In total, 160 RMGIC blocks were prepared. Ten samples (n = 10) were layered with the same material to form a reference-cohesive control group. The remaining samples were distributed among the following groups: No treatment [NT]; Total-etch [OB]; Self-etch [CFSE]; Universal bond in the “total-etch” mode [SBU-TE]; and Universal bond in the “self-etch” mode [SBU-SE]. Samples were stored, and aged by thermocycling (5000 cycles at 5 °C / 55 °C, 30 s) and then prepared for SBS testing. Fracture modes were examined by stereomicroscopy. Data were collected and analyzed statistically at a significance level of P< 0.05.
Results: The highest mean SBS (14.30± 1.08 MPa) was reported in the OB group with the TNCBF material, while the lowest was in the NT group (5.05± 0.69 MPa) with FOBF. Samples in the NT group showed SBS statistically significantly lower than those of samples in all other groups (P< 0.0001). Bulk-fill materials had significantly higher SBS than Z350XT in OB, CFSE, and SBU-SE (P< 0.0001). SBU-TE produced SBS statistically significantly lower than those of other groups for FOBF (P< 0.0001), and lower than that of OB for TNCBF (P=0.027).
Conclusion: OB, CFSE, and SBU-SE are reliable adhesion protocols for bonding bulk-fill RBCs to RMGIC when the “sandwich technique” is used for restorations. However, SBU-TE may not be effective in such procedures.
Keywords: composite resins, bulk-fill, resin-reinforced glass ionomer, universal bond adhesive, bond strength
Introduction
Since the introduction of glass-ionomer cements (GICs) — later known as “conventional” GICs — in the early 1970s by Wilson and Kent,1 they have become popular among dental practitioners for use in dental restorations because of their documented advantages of fluoride release, superior biocompatibility, and chemical bonding to tooth structures compared with resin-based composites (RBCs).2,3 However, because of their relatively weak physical properties, these materials have been improved by the addition of a water-soluble methacrylate monomer, hydroxyl-ethyl methacrylate (HEMA), to the cement to form resin-modified GICs (RMGICs).4
RMGICs possess important improvements over their predecessors.5 However, they are still considered inferior in physical and esthetic properties compared with RBCs. Therefore, the procedure of using GICs to line and replace dentin, then overlay them with stronger and more esthetic materials like RBCs, is used in clinical dentistry.6,7 This “sandwich technique” procedure was first described in 1985 by McLean et al.8
The sandwich technique with RMGIC in Class II restorations has been reported to relieve the stresses caused by RBC.9 In a three-year follow-up study, Van Dijken et al reported the Class II open sandwich technique with RMGIC restorations to be a good alternative to amalgam restorations.10 However, one of the critical factors enabling these restorations to survive the functional challenges in the oral environment is a reliable bond between the RBC and the GIC substrate. This bond is believed to be micromechanical by virtue of the resin-based bonding system. However, for RMGICs, a chemical bond between the resin on the RMGIC and that of the adhesive system is also present.11 Although limited data have been found in the literature describing the bond strength of RMGICs to RBCs, it has been reported to be higher than that of the conventional GICs.7 The bond between RBC and GIC may be affected by several factors, including tensile strength of the base material, the viscosity and wetting ability of the bonding agent, as well as the polymerization shrinkage and adaptability of an overlay RBC material,12 in addition to the differences between the two materials in chemistry and composition.13 Zhang et al reported that bonding a conventional GIC to RBC using the total-etch adhesive yielded a less stable bond compared with that created using self-etch adhesives.14
The term “bulk-fill composite” refers to the RBC class of material that is placed and light-cured in “bulk” layers of 4 mm or more.15 These materials were developed to overcome some of the drawbacks of conventional composites, including polymerization shrinkage stress and limited depth-of-cure, which may lead to failure of the bond between the RBC and tooth structures or to another material.16,17 It has been documented that these materials possess reliable mechanical properties in bulk increments of 4 mm in thickness,18,19 with a greater degree of conversion (DC)20 and similar microhardness and polymerization shrinkage to those of conventional RBCs.21
Multiple studies have evaluated the bond strength of GICs to conventional RBCs in “total-etch” and “self-etch” adhesive systems.11–14,22,23 However, evaluation of the bond strength of RMGICs to newly developed bulk-fill composites by the currently available adhesion protocols has not been well-documented. Knowledge of the bond characteristics of these materials to RMGICs is considered vital for the clinical success of final restorations.
Therefore, the aim of this study was to evaluate the shear bond strengths (SBS) of nano-based composite materials, two bulk-fill and one conventional, to RMGICs after the application of different adhesion protocols, and to compare the results between and among the different adhesion techniques used during the bonding procedures.
When RBCs were bonded to RMGICs by different adhesion protocols, the null hypotheses were that:
- there would be no significant differences in SBS between and among the different adhesion protocol groups for each RBC material; and
- there would be no significant differences in SBS between and among different RBCs within each adhesion protocol, and between bulk-fill materials and conventional material.
Materials and Methods
In this study, the bond strength between a RMGIC (GC Fuji II LC®, GC Corp., Tokyo, Japan) and composite resin-based materials was evaluated based on the following: (1) composite materials used for layering — two bulk-fill (Filtek™ One Bulk Fill [FOBF], 3M ESPE, St. Paul, MN, USA; Tetric®N-Ceram Bulk Fill [TNCBF], Ivoclar Vivadent AG, Schaan, Liechtenstein) and one conventional (Filtek™ Z350 XT [Z350XT], 3M ESPE); and (2) adhesive systems at four levels — a total-etch system (OptiBond™ Solo Plus [OB], Kerr Dental, Orange, CA, USA), a self-etch system (CLEAR FIL SE Bond 2 [CFSE], Kuraray Corp., Tokyo, Japan), and a universal bond system (3M™ Single Bond Universal, 3M ESPE) in total-etch [SBU-TE] and self-etch [SBU-SE] modes. Two groups, one without any adhesive protocol application, and a reference group for evaluation of the cohesive strength of the RMGIC, were also included. Table 1 lists the materials used.
 |
Table 1 List of Materials Used in the Study |
Sample Preparation
Cylindrical acrylic molds with central holes 8 mm in diameter and 4 mm in height were used to fabricate 160 RMGIC (Fuji II LC, shade A1) cylindrical blocks. Ten samples were randomly selected and immediately layered with the same material (Fuji II LC, shade A3) with the use of transparent split acrylic molds with 4 mm x 4 mm central holes, to form the reference-cohesive control group.
The RMGIC samples were built in two layers, 2-mm thickness each, and light-cured according to the manufacturer’s instructions.
The rest of the RMGIC blocks were randomly divided among five adhesion protocol groups, 30 blocks for each group, and further subdivided into 10 blocks for each RBC (n = 10).
Study Groups
- Group 1 (Cohesive control): RMGIC blocks were layered immediately with two layers of the same RMGIC material, shade A3.
- Group 2 (NT): RMGIC blocks were immediately layered, without any treatment, with RBCs.
- Group 3 (Total-etch): RMGIC blocks were treated with 35% phosphoric acid (Ultra-Etch®, Ultradent, South Jordan, UT, USA) for 15 s, rinsed for 15 s, and gently air-dried for 5 s, after which the OB adhesive system was applied.
- Group 4 (Self-etch): RMGIC blocks were treated with the CFSE adhesive system.
- Group 5 (SBU-TE): RMGIC blocks were acid-etched with 35% phosphoric acid for 15 s, rinsed for 15 s, and gently air-dried for 5 s, after which a universal bond adhesive system (SBU) was applied.
- Group 6 (SBU-SE): RMGIC blocks were treated with SBU without prior application of acid etchant.
In all groups, applications of adhesion protocols and light-curing procedures were performed according to the manufacturers’ instructions by means of a light-emitting-diode (LED) curing system, EliparS10 (3M ESPE), at 1200 mW/cm2. The light efficiency was measured by means of an LED radiometer (Demetron, Kerr Dental, USA). During light-curing, the tip of the LED unit was in direct contact with the surface of the material. RBCs were built over the RMGICs with shade A2, in 4-mm diameters and 4-mm thicknesses, with the use of the same split acrylic molds that were used to fabricate the cohesive samples. For the bulk-fill materials, a single layer of 4-mm thickness was used and light-cured for 40 s. Conventional composite was a build-up of two layers of 2-mm thickness each, and light-cured for 20 s.
Shear Bond Strength Testing
Specimens were then cleaned and stored at 37 °C in distilled water for 24 h, then aged by thermocycling for 5000 cycles between 5 and 55 °C with a dwell time of 30 s and a transfer time of 5 s.
Samples were prepared for shear bond strength (SBS) testing. They were mounted on a universal testing machine (Model 5965, Instron Corp., Norwood, MA, USA). Force was applied at the interface between the two bonded materials by means of a notched chisel at a speed of 0.5 mm/min until failure of the RMGIC and composite (or between the two layers of the RMGIC for the cohesive control) occurred, and the force required for debonding was measured and recorded in megapascals (MPa).
Modes of Failure
Failure modes were examined under a digital stereomicroscope at 50x magnification (HIROX KH-7700 Digital Microscope, Tokyo, Japan) for evaluation of the fracture patterns.
Failure modes were classified as follows:
• Adhesive failure (A): failure at the bond interface.
• Cohesive failure (Cb): failure within the base material (RMGIC).
• Cohesive failure (Cc): failure within the composite material.
• Mixed failure (M): failure that was partially adhesive and partially cohesive.
Statistical Analysis
Data were analyzed with SPSS software version 25.0 (IBM Inc., Chicago, IL, USA). Descriptive statistics (means, standard deviations, frequencies, and percentages) were used to describe the quantitative and categorical outcome variables. One-way analyses of variance (ANOVA) followed by Tukey’s multiple-comparisons test were used to compare the mean values of SBS in relation to different types of treatments and different types of materials. Kruskal–Wallis H and Mann–Whitney U-tests were used for modes of failure analysis. A P-value of <0.05 was used to report the statistical significance of the results.
Results
Shear Bond Strength
Material Comparisons
Mean SBS values of the tested RBCs to RMGIC within each adhesion protocol are presented in Table 2.
 |
Table 2 Mean Values of Shear Bond Strength for the Resin-Based Composite Materials Within Each Adhesion Protocol Group |
The one-way ANOVA analysis showed significant differences between different RBCs across all the tested adhesion protocols: NT (F=13.14, P=0.0001), OB (F=70.37, P<0.0001), CFSE (F=12.42, P<0.0001), SBU-TE (F=8.54, P=0.001), and SBU-SE (F=6.62, P=0.005).
Pair-wise comparisons showed no statistically significant difference between FOBF and TNCBF in all adhesion protocol groups (P>0.13) except in the SBU-TE group, where TNCBF showed significantly higher SBS mean values (P<0.002).
In the OB, CFSE, and SBU-SE groups, FOBF and TNCBF were significantly higher in SBS mean values compared with Z350XT (P<0.03). However, in the NT group, Z350XT showed mean SBS values significantly higher than those of both FOBF and TNCBF (P=0.01 and P=0.000, respectively).
In the SBU-TE group, Z350XT showed SBS mean values significantly lower than those of TNCBF (P=0.013), but no different from those of FOBF (P=0.65).
Adhesion Protocol Comparisons
In comparisons of different adhesion protocol groups for each RBC, there were highly significant differences between and among groups for all RBCs: FOBF (F=266.87, P<0.0001), TNCBF (F=173.16, P<0.0001), and Z350XT (F=103.64, P<0.0001).
In all RBC groups, the mean SBS values for NT were significantly lower than those of all other adhesion protocols (P<0.0001).
For FOBF, there were no significant differences among the OB, CFSE, and SBU-SE groups (P>0.73). However, these adhesion protocols showed mean SBS values significantly higher than those of the SBU-TE group (P<0.0001).
For TNCBF, pair-wise comparison indicated no significant differences between the pairs of adhesive system groups (P>0.05), except between OB and SBU-TE, since the latter had significantly lower mean SBS values (P=0.027).
For Z350XT, the mean SBS values of the OB group were significantly lower than those of the CFSE and SBU groups, (P<0.0001), but not significantly different among the last three treatment groups (P>0.3).
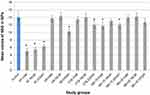
Cohesive Control vs Adhesion Protocol Groups
When the cohesive control group was compared with other groups (Figure 1), the control group showed significantly higher mean SBS (13.97±1.78 MPa) than all RBCs in the NT group (P<0.0001), than Z350XT in the OB, CFSE, and SBU-TE groups (P<0.001), and than FOBF in the SBU-TE group (P=0.01). However, pair-wise comparisons indicated no significant differences between the cohesive control group and other pairs of materials and adhesion protocols (P>0.05).
Modes of Failure
The modes of failure were assessed across the five adhesion protocols (Figure 2), where 100% adhesive failures in all materials were recorded with NT. However, cohesive failures within the RMGIC material were predominant in three groups: from 60% to 100% in OB, from 70% to 100% in CFSE, and from 80% to 100% in the SBU-SE group. However, in the SBU-TE group, 80% of the FOBF samples showed adhesive failure, while cohesive failure within the RMGIC was assessed in 70% of the TNCBF and 80% of the Z350XT. No cohesive failures within the composite materials were assessed in the tested samples.
 |
Figure 2 Stacked bar chart that displays the distribution of modes of failure in adhesion protocol groups. |
Kruskal–Wallis analysis showed no statistically significant differences between RBCs in the distribution of failures across all adhesion protocols (P>0.1), except in the SBU-TE group (P=0.023), where the Mann–Whitney test showed significant differences between FOBF and TNCBF (P=0.026), and between FOBF and Z35XT (P<0.027).
Discussion
Tooth surface treatment is critical to the establishment of a successful bond with an RBC restoration.24 However, preparation of the surface of a tooth-colored restoration, like RMGIC, to be bonded to newly improved RBCs remains controversial.
The use of a “sandwich technique” restoration for layering GIC material with RBC is favorable for deep cavity preparations and has been recommended to promote successful adhesion to dentin with a glass ionomer, therefore securing margins with a good seal.6 RMGIC rather than a conventional GIC was used in this study as the base material, because RMGICs exhibit better bonding to RBCs than do conventional GICs, since the HEMA group in the RMGIC bonds chemically to the adhesive interface and RBC.25 Furthermore, RMGIC materials have the advantage of reduced sensitivity to moisture compared with conventional GICs, making them easier to handle during the adhesion procedures.11 During the layering procedure, in this study, both bulk-fill RBCs were light-cured in a single 4-mm increment with a 1200 mW/cm2 LED unit, since the use of a LED with ≥ 1000 mW/cm2 to achieve acceptable depth-of-cure in bulk-fill RBCs at 4-mm depth has been recommended in the literature.26
Immediate layering of the RMGIC restoration with RBC without any adhesive system resulted in a bond strength that was significantly lower than that in all other adhesion protocols regardless of the type of RBC. Therefore, the null hypothesis that there would be no significant difference between and among different adhesion protocols was rejected for all RBC groups. These results were in agreement with those of Becci et al.27 When RBC was applied over the RMGIC base, the reduced bond strength between the two materials may be explained by the low cohesive strength of the RMGIC compared to the RBC and by the absence of an adhesive bond in the RBC/RMGIC interface, which is responsible for creation of the required mechanical bond between the two materials.12 Furthermore, the differences in the chemistry and reactions between these materials may play important roles in the failure of adhesion without a bonding agent.13
During immediate layering of RMGIC with RBCs in the absence of an adhesive system, all RBCs showed very weak bonds to the RMGIC base; however, Z350XT showed significantly higher bond strength compared with that of the FOBF and TNCBF materials. A possible explanation for the difference between the materials is the higher filler content and larger size fillers of Z350XT, which may render the surface rough for better direct bonding with RMGIC compared with FOBF and TNCBF, with lesser filler contents. Therefore, Mangum et al suggested creating roughness of the conventional GIC surface with a diamond point in addition to acid-etching before application of the adhesive system.28
In this study, the best SBS mean values for bulk-fill materials were reported for OB followed by SBU-SE, then CFSE. However, no statistically significant differences were found among these groups for both bulk-fill materials. When the SBU-TE was used, FOBF produced SBS significantly weaker than those produced by the three previously mentioned adhesion protocols.
In all adhesion protocols, FOBF and TNCBF produced similar results except in the SBU-TE group, where TNCBF produced bonds significantly stronger than those of FOBF. Therefore, the null hypothesis that there would be no significant difference in SBS between and among bulk-fill materials was rejected in the SBU-TE group only. TNCBF composite contains translucent fillers, which enable light to pass through the 4-mm thickness.29 It also uses a benzoyl-germanium-based photoinitiator (Ivocerin) that does not require a co-initiator to produce free radicals, and possesses high reactivity to the wavelength of the light, more than does camphoroquinone, which may assist the polymerization of large increments,26,30 and therefore may explain the differences between the bulk materials, which were significant only in the SBU-TE group.
Compared with bulk-fill RBCs, Z350XT presented significantly lower bond strength in the OB, CFSE, and SBU-SE groups. Therefore, the null hypothesis that there would be no significant difference in SBS between bulk-fill materials and Z350XT was rejected for these groups. The low SBS strength of Z350XT may be explained by the high concentration of TEGDMA diluent monomer in Z350XT, which may have increased its shrinkage, therefore decreasing the bond strength,18 since Kim et al reported high volumetric shrinkage with Z350XT compared with that in several bulk-fill RBCs.31
In the current study, although the OB group showed mean SBS values slightly higher than those of the CFSE group for both bulk-fill materials, these differences were not significant. It has been reported that the etching process did not significantly improve the bond strength between RBCs and GICs.32 In contrast, the SBS mean value for Z350XT was significantly higher in the CFSE group compared with the OB group. These results were in agreement with those of Arora et al and Hinoura et al.33,34 However, in this study, there were no significant differences between the CFSE and SBU groups for the Z350XT material.
In contrast to our results, Pamir et al found that using the “total-etch” adhesive system with RMGIC significantly improved the bond between conventional composite (Filtek Z250) and RMGIC compared with the “self-etch” treatment. However, the acid-etching period where they reported improvement in the bond was 30 s.25 The period of acid-etching for GIC surfaces before bonding to conventional RBCs is controversial. Acid-etching for 30 s has been recommended by some authors,14,34 while others recommended 60 s for a successful bond.8,25 However, deterioration of GIC surfaces when exposed to an acid etchant for longer than 15 s has been reported, and therefore, acid-etching the GIC surface for no longer than 15 s has been recommended.7,11,28
Self-etch adhesive systems have been recommended to be used on initially set material, like GICs, to improve SBS, due to the reported ability of self-etch adhesives to bond with calcium silicate materials by penetrating the material.35 The bonding effectiveness of a two-step “self-etch” adhesive system, such as Clearfil SE Bond 2, can be attributed to the separation of the acidic monomer in the primer from the adhesive agent. Furthermore, the monomer methacryloxydecyl phosphate (MDP) is capable of producing ionic chemical bonds.36
In this study, treating the RMGIC surface with the SBU-TE protocol decreased the bond strength in bulk-fill RBCs compared with that in the SBU-SE and OB groups. This was significant for both materials compared with the OB adhesive system, and only for FOBF in the “non-etchant” mode of the universal bond group. This may be explained by exposure of the RMGIC surface to the acidic monomer in the primer of the universal system, in addition to the separate prior surface-etching with 35% phosphoric acid, which may have affected the surface of the RMGIC and therefore may negatively affect the bond between the bulk-fill materials and the RMGIC.7
The single-bond universal adhesive system utilizes phosphorylated monomers in an aqueous solution that provides acidity to facilitate bonding to tooth structure without the use of separate phosphoric-acid-etching, and therefore is itself considered self-etching. The additional etch step followed by thorough rinsing has been documented to improve the micromechanical bonds between the composite resin and the highly mineralized enamel.37 However, this may not be beneficial for treating surfaces like dentin or bonding to another restorative material like RMGIC. Since the universal bond system is ethanol- and water-based with MDP, when acid-etching is added as a separate step, the bond strength may be reduced, depending on the material used with it.38
In the current study, 100% adhesive failure was assessed with the group that was not treated with any adhesive system. However, in the OB, CFSE, and SBU-SE groups, the majority of samples had cohesive failures within the RMGIC material (80%, 83.3%, and 86.7%, respectively). For the SBU-TE group, only 53.3% failed cohesively within the RMGIC layer. Similar results were reported by Becci et al, since 80% of their samples had adhesive failures in the “total-etch” adhesive system.27 Therefore, the results of this study confirmed those of Becci et al, who reported that the bond among RBC, the adhesive, and RMGIC material was stronger than the cohesive strength of the glass-ionomer base.27
Regardless of the type of composite material used in this study, there was a relatively high percentage of adhesive failure (43.3%) when acid etchant was used combined with a universal bonding system, which confirms that additional acid-etching of the RMGIC in such adhesion systems may weaken the bond and cause adhesive failure between the RBC and the RMGIC.
Conclusions
Within the limitations of this study, the following can be concluded:
- In sandwich technique restorations, immediate layering of RMGIC with bulk-fill or conventional RBCs without any adhesive system yielded a very weak bond. However, when the total-etch, self-etch, or universal bond protocol was used in the “self-etch” mode, reliable bonds were achieved that were significantly higher with bulk-fill composites.
- Universal bonding adhesive in the “total-etch” mode may not be effective in such procedures.
Acknowledgment
The author thanks the College of Dentistry Research Center and Deanship of Scientific Research at King Saud University, Saudi Arabia, for funding this research project (Ref No. FR 0408).
Disclosure
The author reports no conflicts of interest in this work.
References
1. Wilson A, Kent B. A new translucent cement for dentistry. The glass ionomer cement. Br Dent J. 1972;132(4):133–135. doi:10.1038/sj.bdj.4802810
2. Ngo H. Glass-ionomer cements as restorative and preventive. Mater Clin North Am. 2010;54(3):551–563.
3. Sidhu SK. Clinical evaluations of resin-modified glass-ionomer restorations. Dent Mater. 2010;26:7–12. doi:10.1016/j.dental.2009.08.015
4. Nicholson JW, Sidhu SK, Czarnecka B. Enhancing the mechanical properties of glass-ionomer dental cements: a review. Mater (Basel). 2020;13(11):2510. doi:10.3390/ma13112510
5. Burgess JO, Barghi N, Chan DC, Hummert T. A comparative study of three glass ionomer base materials. Am J Dent. 1993;6(3):137–141.
6. Mount GJ, Tyas MJ, Ferracane JL, et al. A revised classification for direct tooth-colored restorative materials. Quintessence Int. 2009;40(8):691–697.
7. Farah CS, Orton VG, Collard SM. Shear bond strength of chemical and light-cured glass ionomer cements bonded to resin composites. Aust Dent J. 1998;43(2):81–86. doi:10.1111/j.1834-7819.1998.tb06095.x
8. McLean JW, Powis DR, Prosser HJ, Wilson AD. The use of glass-ionomer cements in bonding composite resins to dentin. Br Dent J. 1985;158(11):410–414. doi:10.1038/sj.bdj.4805621
9. Andersson‐Wenckert IE, Van Dijken JWV, Hörstedt P. Modified Class II open sandwich restorations: evaluation of interfacial adaptation and influence of different restorative techniques. Eur J Oral Sci. 2002;110:270–275. doi:10.1034/j.1600-0447.2002.11210.x
10. Van Dijken J, Kieri C, Carlén M. Longevity of extensive Class II open sandwich restorations with a resin-modified GIC-composite. J Dent Res. 1999;78:1319–1325. doi:10.1177/00220345990780070601
11. Gopikrishna V, Abarajithin M, Krithikadatta J, Kandaswamy D. Shear bond strength evaluation of resin composite bonded to GIC using three different adhesives. Oper Dent. 2009;34(4):467–471. doi:10.2341/08-009-L
12. Gupta R, Mahajan S. Shear bond strength evaluation of resin composite bonded to GIC using different adhesives. J Clin Diagnost Res. 2015;9(1):ZC27–ZC29.
13. Liu LJ, Liu YY, Sundström SRF. Flexure strength of resin-modified glass ionomer cements and their bond strength to dental composites. Acta Odontol Scand. 1996;54(1):55–58. doi:10.3109/00016359609003510
14. Zhang Y, Burrow MF, Palamara JEA, Thomas CDL. Bonding to glass ionomer cements using resin-based adhesives. Oper Dent. 2011;36(6):618–625. doi:10.2341/10-140-L
15. Ilie N, Hickel R. Investigations on a methacrylate-based flowable composite based on the SDR™ technology. Dent Mater. 2011;27(4):348–355. doi:10.1016/j.dental.2010.11.014
16. Gonçalves F, Campos LMP, Rodrigues-Júnior EC, et al. A comparative study of bulk-fill composites: degree of conversion, post-gel shrinkage and cytotoxicity. Braz Oral Res. 2018;32:e17. doi:10.1590/1807-3107bor-2018.vol32.0017
17. Gonçalves F, Azevedo CL, Ferracane JL, Braga RR. BisGMA/TEGDMA ratio and filler content effects on shrinkage stress. Dent Mater. 2011;27(6):520–526. doi:10.1016/j.dental.2011.01.007
18. Van Dijken JW, Pallesen U. Posterior bulk-filled resin composite restorations: a 5-year randomized controlled clinical study. J Dent. 2016;51:29–35. doi:10.1016/j.jdent.2016.05.008
19. Bayraktar Y, Ercan E, Hamidi MM, Çolak H. One-year clinical evaluation of different types of bulk-fill composites. J Invest Clin Dent. 2017;8(2):1–9. doi:10.1111/jicd.12210
20. Fronza BM, Ayres A, Pacheco RR, Rueggeberg FA, Dias C, Giannini M. Characterization of inorganic filler content, mechanical properties, and light transmission of bulk-fill resin composites. Oper Dent. 2017;42(4):445–455. doi:10.2341/16-024-L
21. Pereira R, Giorgi MCC, Lins RBE, et al. Physical and photoelastic properties of bulk-fill and conventional composites. Clin Cosmet Invest Dent. 2018;10:287–296. doi:10.2147/CCIDE.S184660
22. Smith GE. Surface deterioration of glass-ionomer cement during acid etching: an SEM evaluation. Oper Dent. 1988;13(1):3–7.
23. Knight GM, McIntyre JM. Bond strengths between composite resin and auto cure glass ionomer cement using the co-cure technique. Aust Dent J. 2006;51(2):175–179. doi:10.1111/j.1834-7819.2006.tb00423.x
24. Inoue S, Abe Y, Yoshida Y, et al. Effect of conditioner on bond strength of glass-ionomer adhesive to dentin/enamel with and without smear layer interposition. Oper Dent. 2004;29(6):685–692.
25. Pamir T, Şen BH, Evcin Ö. Effects of etching and adhesive applications on the bond strength between composite resin and glass-ionomer cements. J Appl Oral Sci. 2012;20(6):636–642. doi:10.1590/S1678-77572012000600008
26. Lima RBW, Troconis CCM, Moreno MBP, Murillo-Gómez F, De Goes MF. Depth of cure of bulk fill resin composites: a systematic review. J Esthet Restor Dent. 2018;30(6):492–501. doi:10.1111/jerd.12394
27. Becci ACO, Benetti MS, Domingues NB, Giro EMA. Bond strength of a composite resin to glass ionomer cements using different adhesive systems. Rev Odontol UNESP. 2017;46(4):214–219. doi:10.1590/1807-2577.01717
28. Mangum FI, Berry EA
29. Jang J-H, Park S-H, Hwang I-N. Polymerization shrinkage and depth of cure of bulk-fill resin composites and highly filled flowable resin. Oper Dent. 2015;40(2):172–180. doi:10.2341/13-307-L
30. Ilie N, Bucuta S, Draenert M. Bulk-fill resin-based composites: an in vitro assessment of their mechanical performance. Oper Dent. 2013;38(6):618–625. doi:10.2341/12-395-L
31. Kim RJ, Kim YJ, Choi NS, Lee IB. Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J Dent. 2015;43(4):430–439. doi:10.1016/j.jdent.2015.02.002
32. Bona AD, Pinzetta C, Rosa V. Effect of acid etching of glass ionomer cement surface on the microleakage of sandwich restorations. J Appl Oral Sci. 2007;15(3):230–234. doi:10.1590/S1678-77572007000300014
33. Arora V, Kundabala M, Parolia A, Thomas MS, Pai V. Comparison of the shear bond strength of RMGIC to a resin composite using different adhesive systems: an in vitro study. J Conserv Dent. 2010;13(2):80–83. doi:10.4103/0972-0707.66716
34. Hinoura K, Suzuki H, Onose H. Factor influencing bond strengths between unetched glass ionomer and resins. Oper Dent. 1991;16:90–95.
35. Ha H‑T. The effect of the maturation time of calcium silicate‑based cement (Biodentine™) on resin bonding: an in vitro study. Appl Adhes Sci. 2019;7:1. doi:10.1186/s40563-019-0118-7
36. Yoshida Y, Nagakane K, Fukuda R, et al. Comparative study on adhesive performance of functional monomers. J Dent Res. 2004;83(6):454–458. doi:10.1177/154405910408300604
37. Muñoz MA, Luque-Martinez I, Malaquias P, et al. In vitro longevity of bonding properties of universal adhesives to dentin. Oper Dent. 2015;40:282–292. doi:10.2341/14-055-L
38. Cardoso GC, Nakanishi L, Isolan CP, Jardim PS, Moraes RR. Bond stability of universal adhesives applied to dentin using etch-and-rinse or self-etch strategies. Braz Dent J. 2019;30(5):467–475. doi:10.1590/0103-6440201902578
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.