Back to Journals » Patient Preference and Adherence » Volume 10
Sexual attitudes, norms, condom use, and adherence of Hispanic and non-Hispanic undergraduate students: a cross-sectional study of three community colleges in southwestern US
Authors Bird Y, Solis L, Mbonu C
Received 17 March 2016
Accepted for publication 28 June 2016
Published 5 August 2016 Volume 2016:10 Pages 1501—1508
DOI https://doi.org/10.2147/PPA.S108688
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Yelena Bird,1 Luis H Solis,2 Chinaedu Anulika Mbonu1
1School of Public Health, University of Saskatchewan, Saskatoon, Canada; 2Department of Metallurgical, Materials and Biomedical Engineering, University of Texas at El Paso, El Paso, TX, USA
Objective: To measure the sexual attitudes, norms, condom use, and adherence of Hispanic and non-Hispanic undergraduate students in three community colleges in the southwestern US.
Methods: A previously validated instrument was used in this study (sexual risk behavior beliefs and self-efficacy survey). Statistical analyses included chi-square and one-way analysis of variance with post hoc multiple comparisons using the Statistical Program for the Social Sciences.
Results: The study participants included 234 first and second year community college students. Nearly 91% of them were sexually active and 95% reported healthy sexual attitudes. However, only 29% reported adhering to consistent condom use. More females believed that condoms should always be used, even if the two people knew each other very well, when compared to males (P=0.04). Hispanic female participants were less confident they could abstain from sex when compared to non-Hispanics (P=0.00). Non-Hispanic females were more confident they could use or explain to their partner how to use a condom correctly and go to the store to buy condoms than their Hispanic female (P=0.01) and male counterparts (P=0.00).
Conclusion: Our study findings indicate that adherence to consistent condom use was low among Hispanic college students. This may help explain why they are more likely to report unwanted pregnancies and sexually transmitted infections. There is a documented need to introduce culturally sensitive health promotion programming specifically designed to meet the needs of this at-risk and understudied population.
Keywords: sexual attitudes, condom use and adherence, Hispanic and non-Hispanic undergraduate students, community colleges, southwestern US
Introduction
In US, sexual behaviors that result in unintended pregnancies and sexually transmitted infections (STIs) are the fourth leading cause of morbidity and mortality among young adults.1 Many of these young people engage in high-risk sexual behaviors, such as multiple number of sexual partners and low adherence to condom use.2 Consequently, the US has one of the highest STIs and unwanted pregnancy rates in the developed world, almost twice as high as the rates observed in England, Wales, and Canada, and about eight times as high as those reported in the Netherlands and Japan.3
The Center for Disease Control and Prevention estimates that nearly 20 million new cases of STIs occur every year in the US. Approximately half of these cases occur among young people aged 18–24 years, accounting for almost $16 billion in direct health care costs.4 Unlike other diseases, STIs are often associated with social stigma, isolation, and feelings of shame, which may result in depression and various degrees of psychological trauma to infected individuals.5 These infections, if not promptly diagnosed and treated, have the potential to negatively impact a young person’s immediate health and long-term well-being as well as place a significant economic burden on the US health care system.4
Despite advances in treatment, STIs remain a significant health concern in the US. This is especially true among its minority populations, particularly Hispanics. In 2010, Hispanics made up ~13% of the total population of the US but accounted for nearly 19% of all new STI cases.4 Specifically, the rate of chlamydia infections among Hispanics (459.0/100,000) was approximately three times higher than the one reported for Whites (152.1/100,000), while their rates of gonorrhea and syphilis infections were twice as high (74.8/100,000 compared to 35.2/100,000 and 3.3/100,000 compared to 1.8/100,000, respectively).4 Finally, Hispanics living with HIV/AIDS accounted for 21% of all people living with HIV/AIDS in the US and by the end of 2010, an estimated 118,783 of them had already succumbed to the disease.6
Globally, the US ranked as the seventh highest nation in teenage pregnancy rates.7 In 2006, it was reported that 49% of all pregnancies in the US were unintended.8 Noticeable disparities in unwanted pregnancy rates also exist among the various US population subgroups. For instance, college-aged Hispanics are nearly three times more likely to become pregnant (132.8 births per 1,000 females) when compared to Whites (45.2 per 1,000).2 The National Campaign for Teen and Unplanned Pregnancy reported that 61% of females who give birth while attending school do not complete their education, a foremost consequence of unwanted pregnancies among college students.9 Furthermore, they are more likely to be single parents and experience higher levels of emotional, social, and financial distress, which may subsequently result in mental health issues and inadequate parenting.9 Overall, teenage childbearing cost US taxpayers $9.4 billion in 2010.10
These findings are significant in scope and have far-reaching implications for the Hispanic community. Over the last couple of decades, the Hispanic population in the US has shown significant increases. Hispanics are the youngest, largest, and fastest growing ethnic or race minority in the US. Hispanics are projected to reach 128.8 million people by 2060, constituting roughly 31% of the US total population.11 Therefore, programs that help prevent STI and unwanted pregnancies are critically important in the Hispanic community, especially among its young adult population, such as college-aged students.
Given this context, one would expect to find a sufficient number of studies discussing the sexual practices and risk behaviors of young Hispanics. Such studies would be helpful in providing insight to the factors that place young Hispanics at increased risk and may help explain their disproportionate STI and unwanted pregnancy rates. However, a thorough review of the literature reveals limited amount of information on this topic. While there are several well-conducted studies on sexual health behaviors of college students in general, the majority involve study populations composed mainly of Whites but not often Hispanics.
Therefore, the objective of the present study was to examine the sexual attitudes, norms, condom use, and adherence of Hispanic and non-Hispanic undergraduate students in three community colleges in southwestern US. Specifically, it aimed to answer three key questions among participant students: 1) What are their attitudes about sexual intercourse and adherence to condom use? 2) What are their norms or standard perceptions about sexual intercourse and adherence to condom use? and 3) What is their self-efficacy in refusing sex, communicating about condoms, and buying and adhering to the use of condoms?
Methods
Study location
The study took place on three community (ie, 2-year) college campuses in the southwestern region of the US. In general, the people residing in this region are predominantly of Hispanic origin and characterized by factors associated with inequitable access to health care services and poor health outcomes.12 Specifically, health indicators, such as the rates of STIs and unwanted pregnancies, show Hispanic college students to be significantly disadvantaged in their health status when compared to Whites within the region or even Hispanics living in other parts of the country.13
The average student populations at the time of the study and key characteristics among the communities of each participating college according to the 2,010 US Census are as follows.
College 1 had 5,000 students. The college offers instruction leading to associate degrees and technical certificates and preparation for further academic work. Community education and adult education are also offered. It is located in a community of more than 200,000 people. Those of Hispanic origin made up 65.7% of the population. Among the households, 37% had children under the age of 18 years, 46.8% were married, and 16% were led by a single parent (mother). The median income for a household was $36,657. Approximately 24.5% of the population was living below the poverty line, including 34.8% of those under the age of 18 years.14
College 2 had 1,200 students. The college offers Associate of Arts degrees, designed for individuals who plan to complete their educational goals with a baccalaureate degree and Associate of Applied Science degrees, designed for those who enter the work force upon graduation. It serves a community of nearly 30,000 people. Those of Hispanic origin made up 53.1% of the population. Among the households, 29.2% have children under the age of 18 years, 46.0% are married, and 14.0% were led by a single parent (mother). The median income for a household was $30,658. Approximately 16.5% of the population was living below the poverty line, including 21.4% of those under the age of 18 years.14
College 3 had 600 students. It is one of the few educational institutions designated by the US federal government as both Hispanic Serving (Title V) and Native American Serving (Title III). It is located in a community of nearly 10,000 people. Those of Hispanic origin made up 52.4% of the population. Among the households, 37.5% had children under the age of 18 years, 49.5% were married, and 17.1% were led by a single parent (mother). The median income for a household was $30,652. Approximately 21.9% of the population was living below the poverty line, including 31.8% of those under the age of 18 years.14
Sample size
A formula developed by Krejcie and Morgan was used in order to determine the total sample size required for this study.15 The sample size was stratified by the number of students needed from each of the three participating community colleges in order to attain a representative sample from each with a 95% confidence interval.
Study participants
The study included 234 students from three community colleges. Overall, the study participants were representative of the student population at their respective campus. Their academic and sociodemographic characteristics are presented in Table 1. The majority were female (63.2%), Hispanic (50%), full-time (82.5%), first year (ie, freshmen) students (58.1%) with an average age of 23.5 years.
  | Table 1 Sociodemographic and academic variables of the participating students |
Measures
The instrument used in the present study was the sexual risk behavior beliefs and self-efficacy (SRBBS) survey developed by Basen-Engquist et al.16 The instrument has been validated in previous studies and used to evaluate the effectiveness of multicomponent, school-based programs in promoting condom use and adherence and preventing STIs, HIV/AIDS, and unwanted pregnancies among students.17,18
Sample selection
The SRBBS survey was administered in randomly selected Basic English courses offered to students at each of the three participating colleges. The classes as identified by their course numbers were then placed into a hat and drawn at random for each campus by one of the investigators.
Procedure
The present study was conducted with the permission of the Campus Academic Officers and Institutional Review Boards of the three participating community colleges. Students attending the Introductory English class were chosen to participate in the study. This class was selected based on the fact that it is a general education requirement, which must be completed by all community college students during their freshman or sophomore years.
A package was mailed to each English class instructor, containing a protocol for the study, a copy of the survey instrument, an informed consent, a copy of the approved ethics letter, and an official letter of request for permission to distribute the survey to students during class time. Once permission was obtained from each instructor, classes were randomly selected for survey distribution. During class time, students were informed about the study and provided with an opportunity to either participate (by signing an informed consent) or opt out. Participation in the study was entirely voluntary. Participation incentives were provided to both faculty and students. All instructors were given a coffee mug in appreciation of their cooperation while participating students were each given a pen for their time.
Survey
The document was written in English, consisted of two sections, and took ~25 minutes to complete. The first section included the consent form, the purpose of the study, procedures in the study, risks, benefits, research standards, and the rights of the participants. The second section included the survey and was divided into two parts; the first part contained demographic questions about the participants’ age, sex, ethnicity, relationship, and enrollment status. The second part contained questions on attitudes about sexual intercourse and adherence to condom use, norms or standard perceptions about sexual intercourse and adherence to condoms, and self-efficacy in refusing sex, communicating about condoms, and buying and adhering to the use of condoms. The responses were scored using 3- or 4-point Likert-type scales. The information obtained from the study participants was anonymous. The Cronbach’s alpha for the pilot study was 0.73, which indicated a strong reliability of the SRBBS survey.
Pilot test
A pilot study was conducted to ensure that the survey was reliable and valid for the study population under consideration. A total of 33 students from a Human Sexuality course at one of the three participating community colleges were given the survey instrument and asked to respond to all of the items. They were also asked to point out to the researchers words or phrases that they did not understand in the consent form, instructions, and the SRBBS survey. All comments and suggestions from the pilot study participants were considered by the researchers, and where appropriate, changes were made to the survey used for the main study. The students in the pilot study were excluded from participating in the main study.
Data analysis
The results of the SRBBS survey were analyzed using the Statistical Program for the Social Sciences Graduate Pack 12.0 for Windows (SPSS Inc., Chicago, IL, USA). The significance level selected for this study was set at P<0.05. The study used the SRBBS Likert scales. Low scores indicated decreased sexual risk-taking and protective practices while high scores indicated increased sexual risk-taking and vulnerable practices. Independent variables, such as the participating community colleges and student age, sex, ethnicity, full-time/part-time status, relationship status, and sexual practices, were compared to each of the dependent variables of the SRBBS scales using descriptive statistics. Chi-square and one-way analysis of variance with post hoc multiple comparisons using Scheffé and Student–Newman–Keuls were used.
Results
Sexual behaviors
Our study results indicate that >91% of the student participants were sexually active and 95% believed that condoms should always be used during sex. However, only 29% reported always adhering to condom use during sexual intercourse. Analyses of the sexual practices of the participating students showed that 86% of them engaged in vaginal intercourse, 20% engaged in anal intercourse, and 61% engaged in oral sex.
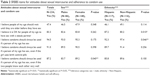
Attitudes about sexual intercourse and adherence to condom use
There were five items in the SRBBS survey that assessed participants’ attitudes about sexual intercourse and adherence to condom use (Table 2). With regard to sexual intercourse, 47.4% of the participants indicated that in general, people of their age should wait until they were older before having sex. However, 83.3% of the participants indicated that it was OK for people of their age to have sex, if they had a steady partner. On this item, there was a statistically significant difference by ethnicity (P=0.01), as Hispanics were more likely to believe that having sex with a steady partner was OK compared to non-Hispanics.
Regarding adherence to condom use, 94.5% of the participants indicated that condoms should always be used by people of their age. There was a statistically significant difference by ethnicity (P=0.04), as non-Hispanics were more likely to believe that condoms should always be used by people of their age compared to Hispanics. This number decreased to 91% when the phrase “even if the girl uses birth control pills” was included, and to 87.2% when the phrase “even if the two people knew each other very well” was used. A statistically significant difference by sex (P=0.04) was observed on this last item as more females believed that condoms should always be used, even if the two people knew each other very well, when compared to males.
Norms and perceptions about sexual intercourse and adherence to condom use
There were five items in the SRBBS survey that assessed participants’ norms and perceptions about sexual intercourse and adherence to condom use (Table 3). Regarding sexual intercourse, 25.6% of the participants indicated that their friends believe people of their age should wait until they were older before having sex. However, 87.7% of the participants indicated that their friends believe it was OK for people of their age to have sex, if they had a steady partner. There was a statistically significant difference by sex (P=0.01) on this item, with more females indicating that their friends believe it was OK for people of their age to have sex, if they had a steady partner, when compared to males.
With regard to adherence to condom use, 79.1% of the participants indicated that their friends believe condoms should always be used by people of their age during sex. However, this number decreased to 70.1% when the phrase “even if the girl uses birth control pills” was included. Finally, 70.6% of the participants indicated that their friends believe condoms should always be used, even if the two people knew each other very well. There were no statistically significant differences by ethnicity and sex on these items.
Self-efficacy in refusing sex, communicating about condoms, and buying and adhering to the use of condoms
There were seven items in the SRBBS survey that assessed participants’ self-efficacy in refusing sex, communicating about using condoms, and buying and adhering to the use of condoms (Table 4). For the first item, 88.1% of the participants indicated that they could abstain from sex, if they wished. Statistically significant differences were observed in this item by ethnicity (P=0.02) and sex (P=0.00). Hispanic female participants were less confident they could abstain from sex when compared to non-Hispanics. Second, 93.1% of the female students indicated that they could abstain from sex, until their partner agreed to use a condom. Interestingly, freshmen female students were more confident than sophomores that they could abstain from sex until their partner agreed to use a condom (P=0.01).
A total of 96.5% of the participants specified that they could tell their partner they wanted to start using condoms and 94% indicated that they could convince their partner to adhere to their request. On the fifth and sixth items, 94.5% of the participants indicated that they could use or explain to their partner how to use a condom correctly, and 94% felt they could go to the store to buy condoms. There were statistically significant differences by sex on these two items as female participants were more confident they could use or explain to their partner how to use a condom correctly (P=0.00) and go to the store to buy condoms (P=0.01) than their male counterparts. Finally, 76.5% of the participants indicated that they were sure they would have a condom with them, whenever they need it.
Discussion
Condoms are known to represent one of the most effective methods of preventing STIs and unwanted pregnancies. However, although 91% of the participating students in our study reported being sexually active and 95% believed that condoms should always be used, only 29% reported consistently adhering to the use of condoms during intercourse. These responses reveal that while participating students are fully aware of the importance of condom use, this knowledge does not necessarily translate into healthier sexual practices. This observation is consistent with Gurman and Borzekowski who found that among sexually active Hispanic college students, fewer than half reported using condoms during their last oral (5%), vaginal (41%), or anal (28%) sexual encounter.19 Previous studies suggest that health education and knowledge are necessary but not sufficient to cause behavioral change.20,21
Furthermore, a number of our study participants erroneously believed that oral contraceptives also protected them against the spread of STIs and, therefore, condoms were not needed. This result is concerning but not entirely surprising. It is possible that as they had heard about the effectiveness of condoms in providing birth control and preventing STIs, they oversimplified this information and generalized it to also include oral contraceptives. For some study participants, birth control and disease control were viewed as one and the same issue, never realizing that dual protection is recommended. Previous studies corroborate our finding and identify the need to design curriculum that address this important gap in knowledge among young people and especially Hispanics.22,23
In our study, female Hispanic students reported healthier sexual practices when compared to males. First, they were more likely to agree that condoms should always be used during sexual intercourse even if two people knew each other very well. This response may be associated with the fact that sociocultural norms, especially in the Hispanic culture, unfairly place the burden associated with an unwanted pregnancy on females, who in most cases are forced to drop out of school so as to be able to nurture and provide for their newborn.9,24 Second, they reported more confidence in knowing how to use a condom as well as how to explain this correctly to their partner. This finding may be best understood by the fact that female are generally more concerned and better informed about their health and utilize health care services more often than male.25 Finally, they were also more confident that they could go to the store and buy condoms. As female begin to buy and use feminine hygiene products from adolescence, it is not surprising that they are more comfortable than male buying and using intimate products, such as condoms.
Additionally, our study found that Hispanic students were more likely to agree that having sex with a steady partner was acceptable when compared to non-Hispanic students. This may be a direct consequence of the sexual attitudes and perceptions specific to Hispanics. Some researchers have argued that as Hispanic students reportedly have higher sexual activity and suffer disproportionate rates of STIs, sexual relations with a long-term partner rather than casual hookups may seem a safer and preferred alternative.26
In line with previous research,26,27 our study demonstrated that student participants were less likely to use condoms if they were in a long-term relationship with their partner. However, the majority of our student participants were not in a long-term relationship and while their reported sexual activity increased between their first (ie, freshman) and second year (ie, sophomore) in college, their self-efficacy in refusing to have sex until their partner agreed to adhere to using a condom decreased. This finding was both significant and surprising.
Studies have shown that the odds of sexual intercourse among students increase at a comparatively gradual pace between their freshman and senior years in college.1,3 Additionally, it has been reported that with increased sexual activity comes increased adherence to the use of condoms.3 However, the results of our study do not support this observation. On the contrary, the odds of unprotected sexual intercourse increased significantly for both male and female students as they transitioned from their first (ie, freshman) to their second (ie, sophomore) year in college. It is possible that second-year students become largely desensitized to the risks of unprotected sex as a consequence of their increased familiarity and growing comfort level with their college community and social networks.27,28 This may lead them to develop a false sense of security and puts them at an increased risk to engage in unprotected sex.29
The present study has several strengths and limitations. Among its strengths are the high response rate, use of a validated survey instrument, and the clear patterns of association found across a number of sexual behaviors when comparing Hispanic to non-Hispanic and female to male college students. The study was also subject to several limitations. First, one should be cautious about drawing conclusions as our results may not apply to all community colleges. Second, the results of our study are subject to recall bias as students were asked to report on sexual behaviors during the past 12 months. Third, as sexual health is a sensitive topic, participants may have responded based on some factor of perceived social desirability. Finally, the study design was cross-sectional in nature and while it provides evidence in support of certain associations, it cannot be used to explain causation.
Implications for practice
Over the last few decades, much progress has been made but gaps still exist between young adults’ intentions to engage in safer sexual practices and their actual adherence to consistent condom use. Several factors were investigated in our study and found to be important in positively influencing condom use among Hispanic and non-Hispanic community college students. These factors included condom availability, positive attitudes about adherence to condom use, peer norms and perceptions that are supportive of condom use, and self-efficacy in refusing sex, communicating about condoms, and buying and adhering to the use of condoms. As such, there is a critical need to develop, support, and promote a student-focused, behavioral-driven condom awareness, knowledge, use, and adherence program at community colleges. Such programs have proven effective in helping reduce unsafe sexual practices (ie, STIs and unwanted pregnancies), increasing condom use, and decreasing the number of condom-related errors among adolescents.8,30–32
Conclusion
The sexual attitudes, norms, and behaviors of college students are of significant interest to a variety of groups, including researchers, policy makers, university administrators, and the general public. Colleges provide an ideal setting to reach a large number of young adults, including Hispanics. Our study findings indicate that adherence to consistent condom use was low among Hispanic college students. This may help explain why they are more likely to report unwanted pregnancies and STIs. There is a documented need to introduce culturally sensitive health promotion programming specifically designed to meet the needs of this at-risk and understudied population.
Disclosure
The authors report no conflicts of interest in this work.
References
Centers for Disease Control and Prevention (CDC). National Youth Risk Behavior Survey. Trends in the Prevalence of Selected Risk Behaviors for All Students; 2013. Available from: http://www.cdc.gov/mmwr/pdf/ss/ss6304.pdf. Accessed October 25, 2015. | ||
Gavin L, Mackay A, Brown K, et al. Sexual and reproductive health of persons aged 10–24 years, United States, 2002–2007. MMWR Surveill Summ. 2009;58:1–58. | ||
Franklin RM, Dotger S. Sex education knowledge differences between freshmen and senior college undergraduates. Coll Stud J. 2011;45(1):199–213. | ||
Center for Disease Control and Prevention (CDC). Fact Sheet: Reported STDs in the United States, National Data for Chlamydia, Gonorrhea and Syphilis; 2013. Available from: http://www.cdc.gov/nchhstp/newsroom/docs/factsheets/std-trends-508.pdf. Accessed October 27, 2015. | ||
Kaiser Family Foundation. Sexually transmitted diseases in America: How many cases and at what cost? 2003. Available from: http://www.kff.org/content/archive/1445/std_rep3.html. Accessed September 24, 2015. | ||
Centers for Disease Control and Prevention (CDC). Fast Facts: HIV Among Hispanics/Latinos in the United States and Dependent Areas; 2013. Available from: http://www.cdc.gov/hiv/pdf/risk_latino.pdf. Accessed October 24, 2015. | ||
World Health Organization. World Health Statistics; 2012. Available from: http://www.who.int/gho/publications/world_health_statistics/EN_WHS2012_Full.pdf. Accessed October 14, 2015. | ||
Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84(5):478–485. | ||
The National Campaign to Prevent Teen and Unplanned Pregnancy. Briefly: Unplanned Pregnancy Among Unmarried Young Women. Washington, DC: Author; 2012. Available from: https://thenationalcampaign.org/resource/briefly-unplanned-pregnancy-among-unmarried-young-women. Accessed November 15, 2015. | ||
The National Campaign to Prevent Teen Pregnancy. Counting It Up: The Public Costs of Teen Childbearing. Washington, DC: Author; 2013. Available from: https://thenationalcampaign.org/why-it-matters/public-cost. Accessed November 15, 2015. | ||
United States Census Bureau. FFF: Hispanic Heritage Month, 2014. Available from: http://www.census.gov/newsroom/facts-for-features/2014/cb14-ff22.html. Accessed November 28, 2015. | ||
United States-México Border Health Commission. Access to Health Care in the U.S.-México Border Region: Challenges and Opportunities. A White Paper, 2014. Available from: http://www.borderhealth.org/files/res_2756.pdf. Accessed November 19, 2015. | ||
Buhi ER, Marhefka SL, Hoban MT. The state of the union: sexual health disparities in a national sample of US college students. J Am Coll Health. 2010;58(4):337–346. | ||
U.S. Census Bureau. Profile of General Population and Housing Characteristics: 2010 Demographic Profile Data. Available from: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk. Accessed May 21, 2016. | ||
Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30:607–610. | ||
Basen-Engquist K, Edmundson EW, Parcel GS. Structure of health risk behavior among high school students. J Consult Clin Psychol. 1996;64(4):764–775. | ||
Davis CM, Yarber WL, Bauserman R, Schreer G, Davis SL. Handbook of Sexuality-Related Measures. Thousand Oaks, CA: SAGE Publications; 1998. | ||
Farmer MA, Meston CM. Predictors of condom use self-efficacy in an ethnically diverse university sample. Arch Sex Behav. 2006;35(3):313–326. | ||
Gurman T, Borzekowski DL. Condom use among Latino college students. J Am Coll Health. 2004;52(4):169–178. | ||
Hubley J. Interventions Targeted at Youth Aimed at Influencing Sexual Behavior and AIDS/STDs. United Kingdom: Leeds Health Education Database; 2000. | ||
Shu C, Fu A, Lu J, et al. Association between age at first sexual intercourse and knowledge, attitudes and practices regarding reproductive health and unplanned pregnancy: a cross-sectional study. Public Health. 2016;135:104–113. | ||
Abma JC, Martinez GM, Mosher WD, Dawson BS. Teenagers in the United States: sexual activity, contraceptive use, and childbearing. Vital Health Stat. 2002;23(24):1–48. | ||
Buhi RE, Marhefka LS, Wheldon WC, et al. Sexual and reproductive health disparities in a national sample of Hispanic and non-Hispanic white U.S. college students. J Health Dispar Res Pract. 2014;7(1):19–36. | ||
Dantzker ML, Eisenman R. Sexual attitudes among Hispanic college students: differences between males and females. Int J Adolesc Youth. 2003;11(1):79–89. | ||
Braunack-Mayer A, Avery JC. Before the consultation: why people do (or do not) go to the doctor. Br J Gen Pract. 2009;59(564):478–479. | ||
Malcolm S, Huang S, Cordova D, et al. Predicting condom use attitudes, norms, and control beliefs in Hispanic problem behavior youth: the effects of family functioning and parent–adolescent communication about sex on condom use. Health Educ Behav. 2013;40(4):384–391. | ||
Manning WD, Giordano PC, Longmore MA. Hooking up the relationship contexts of ‘non-relationship’ sex. J Adolesc Res. 2006;21(5):459–483. | ||
Downing-Matibag TM, Geisinger B. Hooking up and sexual risk taking among college students: A health belief model perspective. Qual Health Res. 2009;19(9):1196–1209. | ||
Fielder RL, Carey MP. Predictors and consequences of sexual ‘hookups’ among college students: a short-term prospective study. Arch Sex Behav. 2010;39(5):1105–1119. | ||
Centers for Disease Control and Prevention. Strategic Plan: Division of HIV/AIDS Prevention 2011 Through 2015. Atlanta, GA: Centers for Disease Control and Prevention; 2011. Available from: http://www.cdc.gov/hiv/pdf/policies_dhap-strategic-plan.pdf. Accessed March 5, 2016. | ||
Centers for Disease Control and Prevention. Youth risk behavior surveillance – United States, 2013. MMWR. 2014;63(4):1–168. | ||
Synovitz L, Herbert E, Kelley R, et al. Sexual knowledge of college students in a southern state: relationship to sexuality education results of Louisiana college student study shows need for sexuality programs. Am J Health Stud. 2002;17:163–173. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.