Back to Journals » International Journal of General Medicine » Volume 15
Sex-Specific Risk Factors Associated with Helicobacter pylori Infection Among Individuals Undergoing Health Examinations in China
Authors Wu Y, Zeng H, Zhang M, Li C, Tang Y, Li X, Yuan S, Wei Q, Wang J , Ning X, Zhang X
Received 19 March 2022
Accepted for publication 27 May 2022
Published 29 June 2022 Volume 2022:15 Pages 5861—5868
DOI https://doi.org/10.2147/IJGM.S367142
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yumei Wu,1 Hui Zeng,2 Meiping Zhang,1 Chunyan Li,2 Yuanlin Tang,2 Xiufen Li,1 Shanyou Yuan,3 Qifeng Wei,3 Jinghua Wang,4 Xianjia Ning,4 Xiaoyin Zhang1
1Department of Gastroenterology, the Third People’s Hospital of Shenzhen, Shenzhen, Guangdong Province, People’s Republic of China; 2Department of Health Management, the Third People’s Hospital of Shenzhen, Shenzhen, Guangdong Province, People’s Republic of China; 3Department of Orthopedics, the Third People’s Hospital of Shenzhen, Shenzhen, Guangdong Province, People’s Republic of China; 4Centre of Clinical Epidemiology, the Third People’s Hospital of Shenzhen, Shenzhen, Guangdong Province, People’s Republic of China
Correspondence: Xiaoyin Zhang, Department of Gastroenterology, the Third People’s Hospital of Shenzhen, 29 Bulan Road, Longgang District, Shenzhen, Guangdong Province, 518112, People’s Republic of China, Tel +86-755-61222333, Fax +86-755-61238928, Email [email protected] Xianjia Ning, Center of Clinical Epidemiology, the Third People’s Hospital of Shenzhen, 29 Bulan Road, Longgang District, Shenzhen, Guangdong Province, 518112, People’s Republic of China, Tel +86-755-61222333, Fax +86-755-61238928, Email [email protected]
Purpose: Helicobacter pylori is one of the most common causes of peptic ulcers, gastritis, and gastric cancers. This study investigated sex-specific differences in the prevalence of H. pylori infection and its associated factors among individuals undergoing hospital-based health examinations in southern China.
Methods: This study enrolled consecutive healthy individuals who underwent regular health examinations at a hospital physical examination center between September 2020 and September 2021. Anthropometric characteristics and biochemical profiles were measured. All individuals underwent carbon-13 urea breath tests. Univariate and multivariate analyses were used to evaluate the factors associated with H. pylori infection.
Results: A total of 5035 individuals (men, 59.1%; women, 40.9%) were included in the analyses. The total rate of H. pylori infection was 35.0% (men, 35.5%; women, 34.3%). In the multivariate analysis, the risk factors identified for H. pylori infections were high fasting blood glucose levels and blood pressure ≥ 160 mmHg in men and older age, high body mass index, and low albumin levels in women.
Conclusion: These findings suggest that physicians must be aware of the metabolic factors associated with H. pylori infections in the Chinese population. Early detection of these factors and timely intervention are expected to reduce H. pylori infections and provide a theoretical basis for the primary prevention of several gastrointestinal diseases.
Keywords: Helicobacter pylori infection, gastrointestinal disease, sex differences, prevalence, metabolic factors
Introduction
Helicobacter pylori is a spiral-shaped Gram-negative bacterium, which plays a role in the development of gastritis, peptic ulcers, and gastric cancers in humans. In recent years, H. pylori infections have been reported to be closely related to cardiovascular disease and its risk factors.1 Moreover, H. pylori has recently been listed as a human carcinogen by the National Toxicology Program of the US Department of Health and Human Services.2
H. pylori infections are estimated to exist in more than half of the global population,3 especially in developing countries where the incidence may reach 80–90%.4 China is a high-incidence area of H. pylori infection.5 In addition, the prevalence of H. pylori infections varies based on geographical locations, environmental factors, sociodemographic characteristics, and socioeconomic status.6 With the rapid economic growth and development observed in recent decades, an evaluation of the prevalence of H. pylori infections observed during routine checkups in a small segment of the population is expected to reflect the prevalence of these infections in the general population.
The factors associated with H. pylori infections have not been firmly established. Socioeconomic status is an important determinant that is negatively correlated with H. pylori infection.7 Additionally, H. pylori infections appears to be more prevalent among men than among women. Recently, metabolic factors have gained increasing attention owing to their possible association with H. pylori infection. Individuals who are overweight or obese tend to have a higher prevalence of H. pylori infections.8 Moreover, potential associations between metabolic syndrome, insulin resistance, and H. pylori infection have been observed in several studies.9 However, few data are available regarding sex-specific differences associated with H. pylori infections, especially in urban, developed areas in China.
In this study, we evaluated the prevalence of H. pylori infection in healthy individuals undergoing routine health examinations in one region of China to identify sex-specific metabolic factors associated with H. pylori infection.
Methods
Participant Selection and Study Design
This retrospective study enrolled adults aged ≥18 years undergoing the regular health examination at the Third People’s Hospital of Shenzhen between September 2020 and September 2021. The analyses were limited to participants with complete anthropometric and biochemical data and those who had H. pylori test results.
The study was approved by the Ethics Committee of the Third People’s Hospital of Shenzhen and conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent. In this study, personal identification information was anonymized and replaced with a coding system.
Information Collection
Information on sex, age, and clinical examinations was collected from the medical records. Each participant’s clinical examination included anthropometric and laboratory measurements. Age was categorized into five groups: <30 years, 30–39 years, 40–49 years, 50–59 years, and ≥60 years.
Anthropometry
Anthropometric indicators included height, weight, and blood pressure. All measurements were performed by trained doctors or nurses using standard methods. Height and weight were measured with the participant wearing light clothing and no shoes. Blood pressures, both diastolic (DBP) and systolic (SBP), were recorded using an automated sphygmomanometer. Diagnoses of hypertension and diabetes were based on participant self-reports or medical records. Body mass index (BMI) was calculated using the following formula: weight [kilogram (kg)] divided by the square of the height [meter (m)]. Participants with a BMI <24.0 kg/m2, 24.0~27.9 kg/m2 and ≥28.0 kg/m2 were defined as the normal weight, overweight, and obesity groups, respectively.
Laboratory Measurements
Fasting blood samples were obtained for biochemical examinations following an overnight fast of at least 12 hours. Laboratory measurements included fasting blood glucose (FBG), total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), serum albumin, and uric acid.
H. pylori Test
H. pylori infections were diagnosed based on the results of a fasting carbon-13 urea breath test (13C-UBT). A 13C-UBT is one of the most reliable, widely applied, and noninvasive methods used to test for H. pylori infection.10,11
The 13C-UBT was carried out according to standard procedures.12 Briefly, participants were required to fast for at least 2 hours; discontinue various antibiotics within 1 month of the test; and discontinue use of any proton pump inhibitors, bismuth, or H2-receptor inhibitors within 2 weeks of the test. A baseline breathing sample was collected by asking each person to blow through a straw into a 10-mL plastic container. Then, the individual was required to take a tablet containing 75 mg of 13C-urea with 100 mL of water. A second breath sample was collected 30 minutes later. The breath samples were analyzed using an infrared heterodyne radiometer. If the 30-minute sample demonstrated a value that was >4% different from the baseline value, the participant was considered to have tested positive for an H. pylori infection.
Statistical Analysis
Continuous variables (including age, BMI, SBP, DBP, FBG, TC, TG, HDL-C, LDL-C, uric acid, and albumin) were presented as means and standard deviations, while categorical variables (including sex, age group, BMI group, hypertension, diabetes, and nutrition risk) were presented as frequencies and percentages. Student’s t-tests and Pearson’s chi-squared tests were used to analyze differences in the means and proportions between patients with and without H. pylori infections and between the sexes. Factors associated with H. pylori infection were assessed separately for men and women using univariate and multivariable regression analyses. Significant variables (P<0.1) in the two-tailed univariate analyses were selected for multivariable logistic regression analyses. Age and BMI were analyzed as continuous variables in the multivariable logistic regression analyses. The results of the multivariate analysis are presented as odds ratios (ORs) and 95% confidence intervals (CIs), after adjusting for covariates. A two-tailed P-value of <0.05 was considered significant. All statistical analyses were performed using SPSS software (Version 19.0; SPSS; Chicago, IL, USA).
Results
Study Participant Characteristics by Sex
Of the 5035 participants enrolled in this study, 59.1% were men and 40.9% were women (Table 1). The overall average age of the participants was 39.18 years, with <5% of the participants being >60 years old. In the overall study population, the prevalence of hypertension and diabetes was 12.6% and 7.3%, respectively. The overall average BMI (23.93 kg/m2), SBP (120.45 mmHg), DBP (75.54 mmHg), FBG (5.33 mmol/L), TC (4.85 mmol/L), TG (1.62 mmol/L), HDL (1.30 mmol/L), LDL (3.09 mmol/L), uric acid (362.27 µmol/L), and albumin (46.64 g/L) levels were determined.
 |
Table 1 Characteristics of All Participants by Gender |
H. pylori Infection Prevalence
H. pylori infections were diagnosed in 1761 (35.0%) participants, with a prevalence of 35.5% and 34.3% among men and women, respectively. The difference between the prevalence rates was not significant (P=0.373; Table 1).
Risk Factors of H. pylori Infection in Men
We analyzed the risk factors for H. pylori infection by sex. Table 2 shows the univariate analysis, demonstrating that the primary risk factor for H. pylori infection in men was the FBG level (P=0.002).
 |
Table 2 Associated Factors of Helicobacter Pylori Infection by Gender in Univariate Analysis |
After adjusting for age, blood pressure, and FBG levels (all P<0.1 in the univariate analysis), a high FBG level (OR=1.089; 95% CI, 1.024–1.157; P=0.007) and blood pressure ≥160 mmHg (OR=2.202; 95% CI, 1.173–4.138; P=0.014) remained significantly associated with a high risk of H. pylori infection in the multivariate analysis (Table 3). The nomogram shows that 42 points for blood pressure ≥160 mmHg, 100 points for FBP (Supplemental Figure 1).
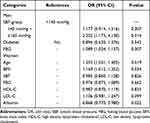 |
Table 3 Multivariable Analysis for Risk Factors Associated with Helicobacter Pylori Infection in Men and in Women |
Risk Factors of H. pylori Infection in Women
For women, the univariate analysis showed that age, BMI, SBP, FBG, TC, HDL-C, LDL-C, and albumin levels were associated with H. pylori infection (all P<0.05; Table 2).
After adjusting for all variables with P<0.1 in the univariate analysis (age, BMI, SBP, FBG, HDL-C, LDL-C, and albumin), only age (OR=1.203; 95% CI, 1.031–1.405;P=0.019), BMI (OR=1.169; 95% CI, 1.012–1.352; P=0.034), and albumin level (OR=0.868; 95% CI, 0.770–0.980; P=0.002) were significantly associated with H. pylori infection (Table 3). The nomogram shows that 92.5 points for age, 93 points for BMI, and 85 points for albumin (Supplemental Figure 2).
Discussion
H. pylori infections are becoming an important health and social issue, especially in China, because of their increasing prevalence. In this study, we investigated the sex-specific differences of H. pylori infection based on health examination data from hospitals in first-tier cities in China. In our study, 35.0% of our cohort was positive for H. pylori infection (35.5% men and 34.3% women). Some metabolic factors were associated with H. pylori infection, including high FBG levels and blood pressure ≥160 mmHg in men and older age, high BMI, and low serum albumin levels in women.
Globally, H. pylori infection is the most common chronic infection, resulting in a serious disease burden. In addition to being an important pathogen associated with chronic gastritis and stomach cancers, H. pylori is also closely associated with the occurrence of non-gastrointestinal diseases. Interestingly, the prevalence of H. pylori infection varies by country and race. In developed countries, the prevalence of infection is declining,13–15 however, H. pylori infections remains high in developing countries. A study from the gastroenterology department of an internal medicine facility in Beijing, China showed that the H. pylori-positive rate was as high as 50% among Chinese adults.16 A recent study reported that the total prevalence of H. pylori infection among asymptomatic individuals was 55.2% in Wenzhou, China.17 In our study, the prevalence of H. pylori infection was 35.0%, which is lower than the previously reported rate of 60% in the rural areas of China.18,19 Considering that China is one of the most rapidly developing countries and that the socioeconomic status of residents has been improving significantly over recent decades, especially in the Shenzhen area where socioeconomic status and income levels are high, a declining trend in the prevalence of H. pylori infection may be occurring. Additionally, a study conducted in Taiwan showed a similar trend to our study in the prevalence of H. pylori infections in men and women.20
There is accumulating evidence that H. pylori infection are associated with a higher risk of diabetes and cardiovascular disease.21–23 A study of 8820 participants in China revealed that H. pylori-positive participants had significantly higher BMIs, waist circumferences, SBPs, and serum levels of TC and LDL-C as well as lower serum HDL-C levels compared to H. pylori-negative participants.24 Some studies have reported that H. pylori infections tend to be more prevalent in obese individuals.8,9 A cross-sectional study of Taiwanese adults reported that H. pylori infection was positively associated with metabolic syndrome, especially in women.20 In the present study, we found an association between H. pylori infection and elevated FBG levels and increased blood pressure in men but not in women. However, a positive correlation was found between H. pylori infection and BMI in women. These results support the hypothesis that sex-specific metabolic factors are associated with H. pylori infections. Larger sample sizes and additional studies are needed to further identify sex-specific risk factors of H. pylori infection.
Epidemiologic studies have shown that the prevalence of H. pylori infection varies considerably with age.20 A cross-sectional study conducted in a university hospital in mainland China suggested that the rate of H. pylori infection increased with age in individuals <36 years old, but no significant correlation was detected between age and prevalence in individuals >36 years old.25 An observational study from an outpatient clinic in Turkey reported that H. pylori seropositivity was associated with increasing age, representing the combined effect of a lower childhood exposure rate (correlated with improved living standards) and a greater chance of acquiring an infection associated with duration of life.26 A nationwide, multicenter study conducted over a 13-year period in Korea reported that the clinical risk factors associated with H. pylori infection were male sex and older age.27 As expected from the results of previous studies, our results also showed that H. pylori infection was more prevalent in older women; however, this trend was not observed in men. This inconsistency may arise from differences in the study population, sample size, and H. pylori infection testing methodologies.
Serum albumin, the most abundant plasma protein, is the main determinant of plasma osmotic pressure and the main modulator of fluid distribution between body compartments.28 Furthermore, previous studies have shown that albumin plays an important part in immunomodulation.29 The results of our study showed that low albumin levels are associated with a higher prevalence of H. pylori infection in women, consistent with the findings of a previous study conducted in southwest China.30 The study demonstrated that low albumin levels were an independent risk factor for H. pylori infection, with individuals with serum albumin levels ≥48 g/L having the lowest rate of infection and individuals with serum albumin levels <45 g/L having the highest rate.30 Low serum albumin levels have been associated with increased infection susceptibility and hospitalization duration;31 moreover, albumin infusions have been shown to have positive effects on patients with infections.32
This study has several limitations. First, the retrospective design of our study prevents the determination of causal relationships. Second, the participants attending the hospital-based health examination may not have been representative of the general Chinese population. For example, the socioeconomic status of the individuals who underwent health checkups may have been higher than the national average, limiting our ability to extend these findings to other regions. Third, some information was not recorded, including antibiotic use, history of gastrointestinal disease, smoking, drinking, and residence information, which can impact the relationship between metabolic factors and H. pylori infection. Thus, further investigation is needed to understand the underlying mechanisms of the association between metabolic factors and infection risk.
Conclusions
This study identified sex-specific differences in the association of metabolic factors with H. pylori infection in a population from southern China, providing data relevant to China’s first-tier urban areas. However, the overall prevalence of H. pylori infection was 35.0%, with no significant difference between the sexes. High FBG levels and blood pressure ≥160 mmHg were positively associated with H. pylori infection in men, whereas older age, high BMI, and low albumin levels were risk factors in women. These findings support the importance of early detection of sex-specific metabolic factors related to H. pylori infections. Monitoring of these metabolic factors and appropriate intervention are needed to reduce the prevalence and burden of H. pylori infection in China.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang B, Yu M, Zhang R, Chen S, Xi Y, Duan G. A meta-analysis of the association between Helicobacter pylori infection and risk of atherosclerotic cardiovascular disease. Helicobacter. 2020;25(6):e12761. doi:10.1111/hel.12761
2. 15th Report on Carcinogens. National Toxicology Program; 2021. Available from: https://ntp.niehs.nih.gov/go/roc15.
3. Mitchell H, Katelaris P. Epidemiology, clinical impacts and current clinical management of Helicobacter pylori infection. Med J Aust. 2016;204(10):376–380.
4. Kamboj AK, Cotter TG, Oxentenko AS. Helicobacter pylori: the Past, Present, and Future in Management. Mayo Clin Proc. 2017;92(4):599–604.
5. Park JY, Forman D, Waskito LA, Yamaoka Y, Crabtree JE. Epidemiology of Helicobacter pylori and CagA-Positive Infections and Global Variations in Gastric Cancer. Toxins. 2018;10(4):163.
6. Mladenova I. Clinical Relevance of Helicobacter pylori Infection. J Clin Med. 2021;10(16):3473.
7. Yan TL, Hu QD, Zhang Q, Li YM, Liang TB. National rates of Helicobacter pylori recurrence are significantly and inversely correlated with human development index. Aliment Pharmacol Ther. 2013;37(10):963–968.
8. Polyzos SA, Kountouras J, Zavos C, Deretzi G. The association between Helicobacter pylori infection and insulin resistance: a systematic review. Helicobacter. 2011;16(2):79–88.
9. Azami M, Baradaran HR, Dehghanbanadaki H, et al. Association of Helicobacter pylori infection with the risk of metabolic syndrome and insulin resistance: an updated systematic review and meta-analysis. Diabetol Metab Syndr. 2021;13(1):145.
10. Goh KL, Manikam J, Qua CS. High-dose rabeprazole-amoxicillin dual therapy and rabeprazole triple therapy with amoxicillin and levofloxacin for 2 weeks as first and second line rescue therapies for Helicobacter pylori treatment failures. Aliment Pharmacol Ther. 2012;35(9):1097–1102.
11. Monteiro L, de Mascarel A, Sarrasqueta AM, et al. Diagnosis of Helicobacter pylori infection: noninvasive methods compared to invasive methods and evaluation of two new tests. Am J Gastroenterol. 2001;96(2):353–358.
12. Shen Z, Qin Y, Liu Y, et al. Helicobacter pylori infection is associated with the presence of thyroid nodules in the euthyroid population. PLoS One. 2013;8(11):e80042.
13. Rothenbacher D, Schultze V, Jähnig P, Scharschmidt B, Brenner H. Evidence of a rapid decrease in prevalence of Helicobacter pylori infection in children of a high risk group living in Germany. Eur J Pediatr. 2004;163(6):339–340.
14. Loffeld RJ, van der Putten AB. Changes in prevalence of Helicobacter pylori infection in two groups of patients undergoing endoscopy and living in the same region in the Netherlands. Scand J Gastroenterol. 2003;38(9):938–941.
15. Pérez-Aisa MA, Del Pino D, Siles M, Lanas A. Clinical trends in ulcer diagnosis in a population with high prevalence of Helicobacter pylori infection. Aliment Pharmacol Ther. 2005;21(1):65–72.
16. Huang GD, Huang YH, Xiao MZ, Huang DF, Liu J, Li JB. Effect of volatile oil of amomum on expressions of platelet activating factor and mastocarcinoma-related peptide in the gastric membrane of chronic gastritis patients with helicobacter-pylori infection. Chin J Integr Med. 2008;14(1):23–27.
17. Wu W, Leja M, Tsukanov V, et al. Sex differences in the relationship among alcohol, smoking, and Helicobacter pylori infection in asymptomatic individuals. J Int Med Res. 2020;48(5):300060520926036.
18. Shi R, Xu S, Zhang H, et al. Prevalence and risk factors for Helicobacter pylori infection in Chinese populations. Helicobacter. 2008;13(2):157–165.
19. Brown LM, Thomas TL, Ma JL, et al. Helicobacter pylori infection in rural China: demographic, lifestyle and environmental factors. Int J Epidemiol. 2002;31(3):638–645.
20. Chen TP, Hung HF, Chen MK, et al. Helicobacter Pylori Infection is Positively Associated with Metabolic Syndrome in Taiwanese Adults: a Cross-Sectional Study. Helicobacter. 2015;20(3):184–191.
21. Jeon CY, Haan MN, Cheng C, et al. Helicobacter pylori infection is associated with an increased rate of diabetes. Diabetes Care. 2012;35(3):520–525.
22. Pasceri V, Cammarota G, Patti G, et al. Association of virulent Helicobacter pylori strains with ischemic heart disease. Circulation. 1998;97(17):1675–1679.
23. Whincup P, Danesh J, Walker M, et al. Prospective study of potentially virulent strains of Helicobacter pylori and coronary heart disease in middle-aged men. Circulation. 2000;101(14):1647–1652.
24. Xu C, Yan M, Sun Y, et al. Prevalence of Helicobacter pylori infection and its relation with body mass index in a Chinese population. Helicobacter. 2014;19(6):437–442.
25. Hong W, Tang HL, Dong XL, et al. Prevalence of Helicobacter pylori infection in a third-tier Chinese city: relationship with gender, age, birth-year and survey years. Microb Health Dis. 2019;1:e150.
26. Burucoa C, Axon A. Epidemiology of Helicobacter pylori infection. Helicobacter. 2017;22(Suppl 1):548.
27. Kanbay M, Gür G, Arslan H, Yilmaz U, Boyacioglu S. The relationship of ABO blood group, age, gender, smoking, and Helicobacter pylori infection. Dig Dis Sci. 2005;50(7):1214–1217.
28. Lim SH, Kwon JW, Kim N, et al. Prevalence and risk factors of Helicobacter pylori infection in Korea: nationwide multicenter study over 13 years. BMC Gastroenterol. 2013;13:104.
29. Fanali G, Di Masi A, Trezza V, Marino M, Fasano M, Ascenzi P. Human serum albumin: from bench to bedside. Mol Aspects Med. 2012;33(3):209–290.
30. Liu J, Wang Y, Zhao Q, et al. Prevalence and risk factors for Helicobacter pylori infection in southwest China: a study of health examination participants based on 13C-urea breath test. Turk J Med Sci. 2017;47(5):1456–1462.
31. Ataseven H, Demir M, Gen R. Effect of sequential treatment as a first-line therapy for Helicobacter pylori eradication in patients with diabetes mellitus. South Med J. 2010;103(10):988–992.
32. Chen TA, Tsao YC, Chen A, et al. Effect of intravenous albumin on endotoxin removal, cytokines, and nitric oxide production in patients with cirrhosis and spontaneous bacterial peritonitis. Scand J Gastroenterol. 2009;44(5):619–625.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
