Back to Journals » Journal of Pain Research » Volume 13
Severity of Wound-Related Pain and Associated Factors Among Patients Who Underwent Wound Management at Teaching and Referral Hospital, Northwest Ethiopia
Authors Tegegne BA , Lema GF , Fentie DY , Bizuneh YB
Received 10 August 2020
Accepted for publication 26 September 2020
Published 13 October 2020 Volume 2020:13 Pages 2543—2551
DOI https://doi.org/10.2147/JPR.S276449
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Robert B. Raffa
Biresaw Ayen Tegegne, Girmay Fitiwi Lema, Demeke Yilkal Fentie, Yosef Belay Bizuneh
Department of Anesthesia, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Girmay Fitiwi Lema
Department of Anesthesia, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Tel +251-9-85-03-15
Email [email protected]
Background: Wound management is one of the commonly performed procedures in hospitals. It can be a major source of pain and pain may be a frequently experienced but under-considered component of wound management. Therefore, we aimed to determine the severity of wound-related pain and identifying factors associated with it among patients who underwent wound management.
Patients and Methods: An institutional-based, cross-sectional study was conducted from March to May, 2020 in the University of Gondar Comprehensive Specialized Hospital. A total of 424 patients were included in this study. Data were collected by direct observation, chart review, and interview of patients by using questionnaires. Statistical analysis had performed using SPSS 25.00 version statistical software. Descriptive statistics were conducted to summarize patients’ information and to determine the prevalence of pain. Bi-variable analysis was performed to determine each of the independent variables and only variables with a P-value< 0.2 were entered into the multivariable analysis. The strength of the association was present by odds ratio and 95% Confidence interval. P-value< 0.05 was consider as statistically significant.
Results: The prevalence of moderate-to-severe wound-related pain during wound management was 94.1% (95% CI=91.7– 96.2). Anxiety (AOR=18.16; 95% CI=4.83– 68.23), acute wound (AOR=11.49; 95% CI=1.013– 130.2), baseline pain (AOR=3.51; 95% CI=1.18– 10.46), and analgesia intake (AOR=0.026; 95% CI=0.001– 0.895) were significantly associated with the severity of wound-related pain.
Conclusion: The prevalence of moderate-to-severe wound-related pain was considerably high. Anxiety, type of wound, baseline pain, and analgesia intake were the independent risk factors. Therefore, wound care providers should assess the severity of wound-related pain and manage accordingly. Additionally, more emphasis should be given for patients who have baseline pain, anxiety, and acute wound.
Keywords: pain assessment, pain management, wound management
Background
Wound is disruption of structural and functional integrity of tissue1. Skin is considered as the largest organ in the body and damage to the skin may alter its functions which can have catastrophic consequences for the patient. Patients having wound at hospital may need wound management in order to fasten wound healing.2
Wound management is the process of removing dead tissue, cleansing the wound or providing a protective environment.3 The most common wound management performed on open wounds are dressing changes and wound cleansing.4 It is a major source of wound-related pain, which may be frequently experienced but underlooked.5
Dressing change causes moderate-to-severe wound-related pain in 74% of patients, nearly half (36%) of them had experienced severe pain which was associated with patient factors like young age, female sex, anxiety, depression and wound-related factors like recent tissue loss, inflammatory wound, baseline wound pain, chronic pain, chronic wound, and partial thickness wound4,6. In addition, factors like size of wound, types of cleansing agents, location of the wound, duration of wound management, and not using analgesics/sedatives were also found to be associated with pain during wound management.7 Despite the increase in quality of pain management, wound management related pain is still poorly managed because of different reasons.8 An international comparative survey on wound-related pain found that practitioners in the wound care service tend to focus on healing processes rather than considering patient’s total pain experience involving an appropriate pain assessment and selection of an appropriate pain management strategy.9. Studies had found that baseline pain and treatment adequacy were not assessed by wound care providers which resulted in inadequate pain management during wound management.10−13
Untreated pain can result in a number of potentially serious events including; delayed mobilization, delayed recovery, cardiac complications, thrombosis, pulmonary complications, stress, anxiety, depression, psychosocial problems, delayed wound healing, and chronic pain syndromes.14
A simple evidence based pharmacological technique was offered as a potential strategie to minimize the experience of pain. Moderate-to-severe wound-related pain was usually treated with opioids and acetaminophen, whereas inflammatory pain was responded better with non-steroidal anti-inflammatory drugs (NSAIDs).7 Combination analgesic therapy for wound-related pain had been found to give better analgesia during wound care procedures.15,16
Pain management practice during wound management can be improved through determining the severity of wound-related pain (WRP) and identifying contributing factors for it. Thus, adequate wound-related pain prevention and management may improve patient satisfaction via hastened wound healing, reducing hospital stay, and cost17. Therefore, this study aimed to assess the severity of wound-related pain (WRP) and its associated factors during wound management.
Patients and Materials
Ethical approval was obtained from the University of Gondar, School of Medicine ethical review committee (Ref No: 1926/03/2020). Written informed consent was obtained from the participants. An institutional based cross-sectional study was conducted among patients who underwent wound management from March–May, 2020 at University of Gondar Comprehensive Specialized Hospital mainly in surgical, trauma, orthopedic, and gynecologic wards.
All adult patients who underwent wound management during the study period were included in the study. Patients who had chronic pain, burn injury, diabetic wound ulcer pain, psychosis, and patients with sensory impairment were excluded.
Variables of the Study
Dependent Variable
Severity of pain (the maximum pain experienced) during wound management was assessed in terms of the verbal rating scale (VRS) pain assessment tool.
Independent Variables
Patient Related Factors
Age, gender, anxiety measured via Six-item state-trait anxiety inventory and depression assessed through personal health questionnaire depression scale.
Clinical/Procedure Related Factors
Duration of WCPs, cleansing solutions used, and using analgesics/sedatives.
Wound-Related Factors
Size of the wound, location of the wound, baseline wound pain, chronic wound pain, type of wound, depth of wound, sign of clinical inflammation, and recent injury of wound.
Operational Definitions
Verbal Rating Scale
A pain assessment scale that consists of a list of describing words about severity of pain (no pain, mild pain, moderate pain, and severe pain). The VRS has high validity and reliability for assessing acute pain. The VRS is one of the most appropriate pain assessment tools for use in adults experiencing procedural pain like WCP since VRS is simple, easy to understand, and a low failure rate than both numeric rating scale and visual analog scale.18–21
Wound Management
It includes dressing changes and wound cleansing.
Chronic Wounds
Wounds that lasts ≥3 months were considered as chronic wounds.22
Chronic Wound Pain
Wound pain that lasts for ≥3 months was considered as chronic wound pain.23
Sensory Impairment
Defined as a lack of sharp vs dull sensation around the wound, especially in a diabetic foot.24
Partial Thickness Wounds
Are wounds that extend only into the first two layers of skin, the epidermis, dermis, or both.25
Recent Injury
The inflammatory period is proposed to last 3–5 days in acute wounds.26
Six-Item State-Trait Anxiety Inventory
This is the short-form of the STAI, which is the most frequently used measure of anxiety. When compared with the full form of the STAI, the six-item version offers a briefer and just as acceptable scale for subjects while maintaining results that are comparable to those obtained using the full form of the STAI. It is a reliable and sensitive measure of anxiety. To calculate the total score, sum all six scores and multiply by 20/6 then you can get a score from 20–80. A total value greater than 20 is considered as having anxiety.27
Personal Health Questionnaire Depression Scale (PHQ-9)
This is established as a reliable and valid diagnostic measure for depression among Ethiopian adults. The total score for the nine questions are added up and can range from 0–27. A score of 5 or greater can be considered for defining current depression.28
Sample Size Calculation and Sampling Techniques
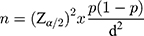
The sample size was calculated using a single population proportion formula
where n is the minimum sample size, Z is the standardized normal distribution value at α/2, p is the prevalence/proportion of pain, and d is the margin of error. Let p denote the proportion of success. Since there was no previous study regarding the incidence or severity of pain during wound care in Ethiopia, we took the 50% (P=0.5), Maximum acceptable difference (d)=5%, desired confidence level: at 95% confidence level and 10% of non-response rate. Therefore, sample size was
n=(1.96)2×0.5(1–0.5)/0.052
where n= 384.16~385: non-response rate=10%, 384.16×10%=38.416~39. The total sample size was 385+39=424 patients were included in this study.
All consecutive patients who fulfilled the inclusion criteria and who had undergone wound management until the calculated sample size was reached were selected.
Data Collection Procedure and Data Quality Control
Data were collected after the completion of wound management by using a semi-structured questionnaire. The questionnaire was including direct observation, chart review, interview of the patient, and wound care provider.
To ensure the quality of data, training had given for three data collectors and one supervisor. To ensure a quality questionnaire, a pretest was done on 22 patients and the necessary corrections were made on the questionnaire for the main study. Pretested respondents were not included in the main study. The data collectors were supervised daily; the filled questionnaires were checked every day for completeness and clarity by the supervisor and the principal investigator.
Data Analysis and Interpretation
Sociodemographic variables, severity of wound-related pain, and associated factors of wound-related pain were entered to Epidata 3.1 version and it was transferred to SPSS 25.00 version statistical software for analysis. Descriptive statistics were conducted to summarize patients’ information and to determine the prevalence of wound-related pain (WRP). To determine the association between severities of wound-related pain with potential predictors, the chi-square test was employed. Binary logistic regression analysis was conducted to identify factors associated with severity of wound-related pain (WRP) and bi-variable analysis was performed to determine each of the independent variables. Only variables with a P-value<0.2 during bi-variable analysis were entered into the multivariate analysis. We have used the Hosmer Lemeshow test of goodness of fit to check the appropriateness of the model for analysis. The strength of the association was presented by adjusted odds ratio and 95% Confidence interval. Finally, data is presented by using numbers or frequencies, percentages, figure, and tables. P-values<0.05 were considered as statistically significant.
Results
Socio-Demographic Characteristics
A total of 424 patents aged 20–80 years who underwent wound management were included. Of these, 268 (63.2%) were males and the remaining 156 (36.8%) were females. Among those patients, 403 (95%) were aged <55 years, while 21 (5%) were aged ≥55 years (Table 1).
 |
Table 1 Sociodemographic Characteristics of the Study Participants at UOGCSH, Ethiopia (n=424) |
The Prevalence of Pain During Wound management
In this study, all patients experienced mild-to-severe wound-related pain (WRP) during wound management. Of therse patients, 25 (5.9%), 116 (27.4%), and 283 (66.7) experienced mild, moderate, and severe wound-related pain, respectively. A total of 399 (94.1%) patients developed moderate-to-severe wound-related pain (95% CI=91.7–96.2) (Figure 1).
 |
Figure 1 Prevalence of wound-related pain. |
Factors Associated with Severity of Wound-Related Pain (WRP) During Wound Management
Patient Related Factors
The majority of patients aged <55 years old experienced moderate-to-severe wound-related pain (380, 89.6%). Two hundred and fifty-six (60.4%) male patients reported moderate-to-severe wound-related pain (WRP). Most of the patients who had anxiety and depression were associated with moderate-to-severe wound-related pain, which accounted for 83.5% and 67.5%, respectively (Table 2).
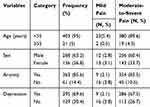 |
Table 2 Patient Related Factors and Severity of Wound-Related Pain During Wound Management in UOGCSH, Ethiopia (N=424) |
Wound-Related Factors
The majority of patients (292, 68.9%) who had baseline wound pain experienced moderate-to-severe wound-related pain during wound management. Among 33 patients having symptoms of inflammatory wound, 32 (7.5%) of them had reported moderate-to-severe WRP. The majority of patients (399, 94.1%) had partial thickness wounds, and 377 (88.9%) of them had experienced moderate-to-severe WRP during wound management (Table 3).
 |
Table 3 Wound-Related Factors and Severity of Wound-Related Pain During Wound Management at UOGCSH, Ethiopia (N=424) |
Procedure Related Factors
The majority of patients (398, 93.9%) did not receive analgesia and reported moderate-to-severe wound-related pain during wound management. Most of the patients (355, 83.7%) whose wound management took ≥14 minutes had associated moderate-to-severe WRP (Table 4).
 |
Table 4 Wound Management Related Factors and Severity of WRP at UOGCSH, Ethiopia (N=424) |
Factors Associated with Moderate-to-Severe WRP During Wound Management
The bi-variable logistic regression showed that age, anxiety, depression, type of wound, baseline pain, depth of wound, duration of wound management, and analgesia intake were associated with moderate-to-severe WRP during wound management at a P-value<0.2.
Baseline wound pain, analgesia intake, acute wound, and anxiety were significantly associated with moderate-to-severe WRP during wound management in multi-variable logistic regression at a P-value<0.05.
The odds of moderate-to-severe WRP wound management among patients who had experienced baseline wound pain were 3.51 (AOR=3.51; 95% CI=1.18–10.46, P-value=0.024) times higher as compared to patients who did not have baseline wound pain. The odds of moderate-to-severe WRP during wound management among patients who received analgesia were 97.4% (AOR=0.026; 95% CI=0.001–0.895, P-value=0.043) lower as compared to patients who did not receive analgesia.
The odds of moderate-to-severe WRP among patients who had acute wounds were 11.49 (AOR=11.49; 95% CI=1.013–130.2, P-value=0.049) times higher as compared to patients having chronic wounds. The odds of moderate-to-severe WRP during wound management among patients who have anxiety was 18.16 (AOR=18.16; 95% CI=4.83–68.23, P-value=0.000) times higher as compared to patients who did not have anxiety (Table 5).
 |
Table 5 Bivariate and Multivariate Logistic Regression Analysis of Factors Associated with Moderate-to- Severe WRP During Wound Management at UOGCSH, Ethiopia (n=424) |
Discussion
The purpose of this study was to find the severity of WRP during wound management and to establish a relationship between the patient-related factors, wound-related factors, and wound management-related factors as predictors of WRP severity.
In this study, moderate-to-severe WRP was reported in 94.1% of the patients, which was considerably high as compared to other studies. A study done at the University of Lowa, USA in 2017 found that 74% of the patients experienced prevalence of moderate-to-severe pain during wound care procedures which was lower than our result.4 Another study done in the USA in 2018 also found a 74% prevalence of moderate-to-severe pain during wound care procedures.6 In addition, a study done in France in 2004 showed that the prevalence of moderate-to-severe pain was reported in 79.9% of the patients.29 Furthermore, 81% of the patients who underwent ae wound care procedure had experienced severe pain at dressing change according to a study done in the USA in 2004.3 The high prevalence of moderate-to-severe pain during wound care procedures in this study area might possibly be due to inconsistent use of analgesics.
In the current study, baseline wound pain, analgesia intake, type of wound, and anxiety were significantly associated with moderate-to-severe pain in multivariable logistic regression.
The result of our study showed that patients who had experienced baseline wound pain had higher odds of moderate-to-severe WRP during wound management than patients who did not have baseline wound pain. Evidence shows that pain was often exacerbated by procedures like dressing changes and wound cleansing. So, a substantial proportion of patients also experienced wound-related pain at rest, and this clinical problem is anticipated, therefore, clinicians should assess and manage this on a regular basis.30 Inadequate management of baseline wound pain was one of the main reasons to experience moderate-to-severe WRP during wound management.31 A study done in the USA in 2002 showed that patients with baseline wound pain were more likely to experience severe WRP and received opiates before and/or during wound management than patients who had no baseline wound pain.32 This might possibly be because the mechanical manipulation of the wound during wound management stimulates sensitized nociceptors through mechanoreceptors in the wound bed, resulting in higher pain.
In this study, patients who received analgesia had lower odds of moderate-to-severe WRP during wound management than patients who did not receive analgesia. Inconsistent with our result, another study showed that 84.1% of patients who reported moderate-to-severe WRP received analgesics during the procedure and the pain severity score after analgesia intake was mild.33 Analgesics such as paracetamol, NSAIDs (diclofenac), and opioids reduce the severity of pain during wound management.34 In addition, administration of analgesics before starting wound care procedures had reduced the severity of pain during WCP.31 Furthermore, for patients with wounds who experienced severe pain, non-steroidal anti-inflammatory drugs and opioids were given during dressing change and it was found to be effective in reducing pain severity during wound management.17 However, a study done in Californiashowed that no difference in severity of pain was reported when NSAIDs were used during wound management with a P-value>0.05 3. This variation from our result might possibly be because of differences in the group of drugs.
In the current study, patients with an acute wound had higher odds of moderate-to-severe WRP during wound management than patients having a chronic wound. In agreement with our finding, a study done at University of Hull, UK in 2009 showed that acute wounds, such as incision wounds following surgery, burn injuries, and traumatic wounds were extremely painful during wound care procedures.2 In addition, an acute wounds that were found in patients with surgical and traumatic wounds had experienced moderate-to-severe WRP during wound management, this might possibly have been due to a consequence of one or all of these mechanisms including nociceptive, inflammatory, neuropathic, and ischemia that encourages anaerobic metabolism, lowering pH, and elevating lactate levels in the wound, which sensitize nociceptors.7 In another study, a similar number of patients with acute and chronic wounds had reported moderate-to-severe pain during wound care procedures (79.9% and 79.7%, respectively).29 Contrary to the current study, patients with chronic wounds reported a higher intensity of pain during wound care procedures than patients with acute wounds.35 A possible reason for this may be the small number of patients who had chronic wounds in the current study.
In this study, anxiety was another major determinant factor for the experiencing of moderate-to-severe WRP during wound management, and the result of our study is in agreement with various studies. Pain during wound management is often triggered by tissue injury or trauma, it may be also modulated by emotional reactions (anxiety).36 Another study also showed that the presence of anxiety before wound management was significantly associated with the severity of pain during wound management.37 Patients who have anxiety had expected more pain and when the wound was manipulated to provide wound management, expectations of increased pain powerfully enhanced the subjective experience of pain.5 A possible reason for this might be because anxiety leads to anticipation of pain, which promotes an overestimation of pain intensity or increases pain perception.4,38
Limitation of the Study
This study did not explore the knowledge and attitudes of wound care providers towards the assessment of severity of wound-related pain, risk factors for wound-related pain, and its management.
Conclusion
The prevalence of moderate-to-severe WRP during wound management was considerably high. Anxiety, the presence of baseline wound pain, acute wound, and analgesia intake were independent risk factors for the severity of WRP during wound management. Therefore, we recommend that wound care providers should assess baseline wound pain, degree of WRP, and manage accordingly. Additionally, more emphasis should be given to patients with baseline wound pain, anxiety, and acute wounds. Furthermore, we recommend further similar studies incorporate the knowledge and attitudes of wound care providers towards pain control during wound care procedures.
Abbrevations
AOR, adjusted odds ratio; COR, crude odds ratio; VRS, verbal rating scale; NSAID, non-steroidal anti-inflammatory drugs; PHQ, personal health questionnaire; SPSS, statistical package of social sciences; STAI, state-trait anxiety inventory; UOGCSH, University of Gondar Comprehensive Specialized Hospital; WRP, wound-related pain.
Data Sharing Statement
Data and materials used in this study are available and can be presented by the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the ethical review committee of college of medicine and health sciences, University of Gondar. Signed informed consent was obtained from each participant after detailed disclosure and in accordance with the Declaration of Helsinki.
Consent for Publication
Not applicable: the article did not include any personal or any clinical detail of any participant.
Acknowledgments
We acknowledge the University of Gondar for giving us the chance to conduct this research. Our gratitude also goes to the data collectors and colleagues for their encouragement through the whole process.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflict of interests.
References
1. Lazarus GS, Cooper DM, Knighton DR, et al. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regeneration. 1994;2(3):165–170.
2. Bowers K, Barrett S. Wound-related pain: features, assessment and treatment. Prim Health Care. 2009;19:10. doi:10.7748/phc2009.12.19.10.37.c7417
3. Stotts NA, Puntillo K, Morris AB, et al. Wound care pain in hospitalized adult patients. Heart Lung. 2004;33(5):321–332. doi:10.1016/j.hrtlng.2004.04.001
4. Gardner SE, Abbott LI, Fiala CA, Rakel BA. Factors associated with high pain intensity during wound care procedures: a model. Wound Repair Regeneration. 2017;25(4):558–563. doi:10.1111/wrr.12553
5. Bechert K, Abraham SE. Pain management and wound care. J Am Col Certif Wound Spec. 2009;1(2):65–71. doi:10.1016/j.jcws.2008.12.001
6. Fiala CA, Abbott LI, Carter CD, et al. Severe pain during wound care procedures: a cross-sectional study protocol. J Adv Nurs. 2018;74(8):1964–1974. doi:10.1111/jan.13699
7. Arroyo-Novoa CM, Figueroa-Ramos MI, Miaskowski C, Padilla G, Stotts N, Puntillo KA. Acute wound pain: gaining a better understanding. Adv Skin Wound Care. 2009;22(8):373–380. doi:10.1097/01.ASW.0000358637.38161.8f
8. Price PE, Fagervik‐Morton H, Mudge EJ, et al. Dressing‐related pain in patients with chronic wounds: an international patient perspective. Int Wound J. 2008;5(2):159–171. doi:10.1111/j.1742-481X.2008.00471.x
9. Coulling S. Fundamentals of pain management in wound care. Br J Nurs. 2007;16(11):S4–6, S8, S10.
10. Eshete MT, Baeumler PI, Siebeck M, et al. The views of patients, healthcare professionals and hospital officials on barriers to and facilitators of quality pain management in Ethiopian hospitals: a qualitative study. PLoS One. 2019;14(3):e0213644. doi:10.1371/journal.pone.0213644
11. Allen KD, Somers TJ, Campbell LC, et al. Pain coping skills training for African Americans with osteoarthritis: results of a randomized controlled trial. Pain. 2019;160(6):1297–1307. doi:10.1097/j.pain.0000000000001525
12. Hollinworth H. Pain at wound dressing-related procedures: a template for assessment. World Wide Wounds. 2005;1.
13. Stotts NA, Puntillo K, Stanik-Hutt J, Thompson CL, White C, Wild LR. Does age make a difference in procedural pain perceptions and responses in hospitalized adults? Acute Pain. 2007;9(3):125–134. doi:10.1016/j.acpain.2007.07.001
14. Size M, Soyannwo O, Justins D. Pain management in developing countries. Anaesthesia. 2007;62:38–43. doi:10.1111/j.1365-2044.2007.05296.x
15. Coulling S. Fundamentals of pain management in wound care. Br J Nurs. 2007;16(Sup2):S4–S12.
16. Richardson C, Upton D. Managing pain and stress in wound care. Wounds UK. 2011;7(4):100–107.
17. Fang Y, Wang N, Shi L, Barker T, Zhang P. Pain relief during wound care for patients with a deep open wound in an orthopedic trauma department: a best practice implementation project. JBI Database Syst Rev Implementation Rep. 2019;17(12):2559–2569. doi:10.11124/JBISRIR-D-19-00126
18. Brown DN. Pain assessment in the recovery room. J Perioper Pract. 2008;18(11):480–489. doi:10.1177/175045890801801103
19. Briggs M, Ferris FD, Glynn C, et al. Assessing pain at wound dressing-related procedures. Nurs Times. 2004;100(41):56–57.
20. Olaogun M, Adedoyin R, Anifaloba R. Reliability and concurrent validity of visual analogue scale and modified verbal rating scale of pain assessment in adult patients with knee osteoathritis in Nigeria. South Afr J Physiother. 2003;59(2):12–15. doi:10.4102/sajp.v59i2.238
21. Given J. Management of procedural pain in adult patients. Nurs Standard (Through 2013). 2010;25(14):35.
22. Werdin F, Tennenhaus M, Schaller H-E, Rennekampff H-O. Evidence-based management strategies for treatment of chronic wounds. Eplasty. 2009;9.
23. Price P, Fogh K, Glynn C, Krasner DL, Osterbrink J, Sibbald RG. Managing painful chronic wounds: the wound pain Management Model. Int Wound J. 2007;4:4–15. doi:10.1111/j.1742-481X.2007.00311.x
24. Falanga V. Wound healing and its impairment in the diabetic foot. The Lancet. 2005;366(9498):1736–1743. doi:10.1016/S0140-6736(05)67700-8
25. Atiyeh BS, El‐MUSA KA, Dham R. Scar quality and physiologic barrier function restoration after moist and moist‐exposed dressings of partial‐thickness wounds. Dermatol Surg. 2003;29(1):14–20.
26. Duperret EK, Natale CA, Monteleon C, Dahal A, Ridky TW. The integrin αv-TGFβ signaling axis is necessary for epidermal proliferation during cutaneous wound healing. Cell Cycle. 2016;15(15):2077–2086. doi:10.1080/15384101.2016.1199306
27. Marteau TM, Bekker H. The development of a six‐item short‐form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI). Br J Clin Psychol. 1992;31(3):301–306.
28. Gelaye B, Williams MA, Lemma S, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. 2013;210(2):653–661. doi:10.1016/j.psychres.2013.07.015
29. Meaume S, Teot L, Lazareth I, Martini J, Bohbot S. The importance of pain reduction through dressing selection in routine wound management: the MAPP study. J Wound Care. 2004;13(10):409–413. doi:10.12968/jowc.2004.13.10.27268
30. Szor JK, Bourguignon C. Description of pressure ulcer pain at rest and at dressing change. J WOCN. 1999;26(3):115–120.
31. Hollinworth H. The management of patients’ pain in wound care. Nurs Standard. 2005;20(7):65–6, 8, 70. doi:10.7748/ns.20.7.65.s54
32. Puntillo KA, Wild LR, Morris AB, Stanik-Hutt J, Thompson CL, White C. Practices and predictors of analgesic interventions for adults undergoing painful procedures. Am J Critical Care. 2002;11(5):415–429. doi:10.4037/ajcc2002.11.5.415
33. Rawe C, Trame CD, Moddeman G, et al. Management of procedural pain: empowering nurses to care for patients through clinical nurse specialist consultation and intervention. Clin Nurse Specialist. 2009;23(3):131–137. doi:10.1097/NUR.0b013e3181a07580
34. Akita S. WUWHS 2012 - better care, better life. J Wound Care. 2012;21(8):357. doi:10.12968/jowc.2012.21.8.357
35. Wiegand C, Schönfelder U, Abel M, Ruth P, Kaatz M, Hipler U-C. Protease and pro-inflammatory cytokine concentrations are elevated in chronic compared to acute wounds and can be modulated by collagen type I in vitro. Arch Dermatol Res. 2010;302(6):419–428. doi:10.1007/s00403-009-1011-1
36. Woo KY. Unravelling nocebo effect: the mediating effect of anxiety between anticipation and pain at wound dressing change. J Clin Nurs. 2015;24(13–14):1975–1984. doi:10.1111/jocn.12858
37. Upton D. Psychological aspects of wound care: implications for clinical practice. J Community Nurs. 2014;28(2):52–57.
38. Koyama T, McHaffie JG, Laurienti PJ, Coghill RC. The subjective experience of pain: where expectations become reality. Proc Natl Acad Sci. 2005;102(36):12950–12955. doi:10.1073/pnas.0408576102
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.