Back to Journals » Clinical Ophthalmology » Volume 13
Seven- and eight-year trends in resident and fellow glaucoma surgical experience
Authors Chadha N, Warren JL, Liu J , Tsai JC , Teng CC
Received 28 August 2018
Accepted for publication 29 November 2018
Published 8 February 2019 Volume 2019:13 Pages 303—309
DOI https://doi.org/10.2147/OPTH.S185529
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nisha Chadha,1,2 Joshua L Warren,3 Ji Liu,2 James C Tsai,1 Christopher C Teng2
1Department of Ophthalmology, Icahn School of Medicine at Mount Sinai, New York Eye and Ear, Eye and Vision Research Institute, NY 10029, USA; 2Department of Ophthalmology and Visual Science, Yale University School of Medicine, New Haven, CT 06510, USA; 3Department of Biostatistics, Yale University, New Haven, CT 06510, USA
Purpose: This study evaluated US resident and fellow glaucoma surgical experience over a 7- and 8-year period, respectively.
Methods: US ophthalmology resident glaucoma case logs from 2009 to 2016 and glaucoma fellow case logs from 2008 to 2016 were reviewed. The number of total, average, median, and minimum cases, along with percentile data for filtering surgery, shunting surgery, and novel procedures were analyzed for year-to-year trends.
Results: Among residents training from 2009 to 2016, there was a decline in the average number of primary filtering surgeries by 20%, from 6.0±5.0 to 4.8±4.0 cases, with a concurrent increase in average primary glaucoma drainage implant (GDI) surgeries by 40%, from 4.5±4.0 to 6.3±5.0 cases, which represented an increase of 6.5% per year, P<0.001. Glaucoma fellow data from 2008 to 2015 demonstrated a decline in average primary trabeculectomy surgeries by 3.7%, from 30.1 to 29.0 cases, but then increased to 32.1 cases in 2015–2016. There was an increase in average GDI surgeries by 57.9%, from 30.2 to 47.7 cases for fellows over this 8-year period, which represented a 5.9% increase per year, P<0.001. There was no microinvasive glaucoma surgery (MIGS) or other novel procedures reported in the Accreditation Council for Graduate Medical Education (ACGME) resident case logs. From 2008 to 2016, Association of University Professors of Ophthalmology (AUPO) glaucoma fellow case logs demonstrated an increase in endocyclophotocoagulation (ECP) from 2.3 to 5.4 cases, a 15.5% increase per year, P<0.001.
Conclusions: Over a 7–8-year period, trainee surgical experience with GDI surgery has steadily increased, whereas surgical experience with trabeculectomy has been fluctuating and may be on a downward trend. Educators should be aware of shifts in trainee surgical experience in order to maintain appropriate training experience.
Keywords: resident education, fellow education, surgical education, ophthalmology education
Introduction
Trabeculectomy has been considered the gold standard glaucoma surgery for the treatment of uncontrolled IOP, with glaucoma drainage implant (GDI) surgery typically being reserved for cases at high risk for filtration failure. In recent years, there has been a shift in the practice patterns of glaucoma specialists, with fewer trabeculectomies and more GDIs being performed. A survey of the American Glaucoma Society (AGS) members’ practice patterns in 2008 found an increase in GDI surgery and a decrease in trabeculectomies. A follow-up survey in 2016 demonstrated a continuation of this trend. This shift in practice pattern is also consistent with Medicare claims data.1–6
Additionally, the field of glaucoma has experienced a wave of new technology, which has offered various safer alternatives for IOP reduction, including microinvasive glaucoma surgeries (MIGSs) and other novel procedures.7 A recent review has revealed an increase in the use of novel procedures such as endocyclophotocoagulation (ECP) and canaloplasty (CP) among glaucoma providers.8 Although these novel therapies offer potentially safer options for glaucoma management, their long-term efficacy has yet to be determined, and therefore, they have not been widely adopted nor have they replaced traditional surgery.7
Equally important as reviewing physician practice patterns is the evaluation of trainee educational experience and trends. Periodic critical analysis of such information is essential for maintaining excellent education of future ophthalmologists. The purpose of this study is to evaluate resident and fellow experiences with both traditional and newer glaucoma procedures by reviewing Accreditation Council for Graduate Medical Education (ACGME) and Association of University Professors of Ophthalmology (AUPO) case log data. The review is intended to provide insight into shifts in trainee glaucoma surgical experience, in order to maintain appropriate training experience.
Methods
The publicly available, ophthalmology resident case log reports, published annually by the ACGME from 2009 to 2016, along with the glaucoma fellow case logs reported by the AUPO from 2008 to 2016 were evaluated.9,10 Reports on “filtering procedures” and “shunting procedures” in the ACGME reports and “trabeculectomy or express shunts” and “aqueous shunt” in the AUPO reports were reviewed for trends in total, average, median, minimum, and percentile data for the number of cases performed as a primary surgeon. The same parameters were evaluated for “endocyclophotocoagulation,” “anterior chamber to Schlemm’s canal shunt,” and “internal shunt (anterior chamber to suprachoroidal space)” in the AUPO glaucoma fellow reports from 2008 to 2016. The only three glaucoma procedure categories in the ACGME case logs are “filtering procedures,” “shunting procedures,” and “other glaucoma.” “Shunting procedures” were therefore interpreted to refer to glaucoma drainage device procedures. Since separate categories are present for some MIGS procedures in the AUPO case logs, “aqueous shunt” was also interpreted to refer to glaucoma drainage devices. If the total number of cases were not reported, total cases per year were calculated by multiplying average cases per fellow or resident by the number of fellows or residents in a given year and rounding to the nearest integer value (Table 1). The Yale Institutional Review Board (IRB)/ethics committee ruled that IRB determination was not required for this study as it did not involve human subjects.
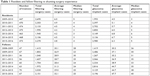  | Table 1 Resident and fellow filtering vs shunting surgery experience |
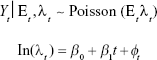
Statistical analysis was performed using a log-linear Poisson regression model with linear time trend effect, offset variable for the number of trainees (results in the modeling rates instead of counts), and observation-level random effects to account for overdispersion that is often observed in count data.11 Specifically, we define the model as
|
where Yt is the number of surgeries (for a selected trainee group and surgery type) performed in year t; Et is the number of trainees in year t (known); λt is the expected rate of surgery per trainee at year t; φt is observation-level random effect to account for overdispersion in Poisson data;  (independent and identically distributed); and β0, β1,
(independent and identically distributed); and β0, β1,  are parameters to be estimated (intercept, slope, and random effect variance, respectively).
are parameters to be estimated (intercept, slope, and random effect variance, respectively).
This model is similar to simple linear regression with year included as the predictor variable in that we can estimate trends in the number of surgeries across time and determine if those trends are statistically significant. However, Poisson regression is more appropriate in this setting because we are modeling count data as opposed to a normally distributed outcome. All models are fit using the glmer function within R statistical software.12
Results
Filtering surgery
The total numbers of resident “filtering procedures” performed as primary surgeon over seven consecutive academic years starting in 2009–2010 were 2,695, 2,303, 2,133, 1,995, 1,945, 2,106, and 2,270 with averages of 6.0, 4.9, 4.5, 4.2, 4.2, 4.5, and 4.8 cases, respectively (Table 1). These numbers generally declined, equating to a 20% decrease in average filtering procedures over this 7-year period. Poisson modeling was suggestive of a 3.3% decrease per year (RR =0.967, P=0.064) (Table 2). In Table 2, we present the statistical inference for the linear time trend predictor that is included in the model. The RR estimates reflect the estimated change in procedure type for a 1-year change in time.
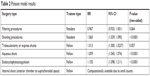  | Table 2 Poisson model results |
The total numbers of primary fellow performed “trabeculectomy or express shunts” over eight academic years beginning in 2008–2009 were 1,415, 1,802, 1,040, 1,607, 1,704, 1,972, 2,030, and 2,151 and the average numbers were 30.1, 26.9, 28.9, 28.7, 28.4, 31.3, 29.0, and 32.1, respectively (Table 1). Among glaucoma fellows, filtering surgery experience initially declined 3.7% from 2008 to 2015, but then increased in 2015–2016. Total data fluctuated from year to year due to variations in the total number of fellows each year ranging from 36 to 70 fellows. The model suggested an increase in fellow performed trabeculectomy over this period, an increase of 1.3% per year (RR =1.013, P=0.057) (Table 2).
The resident percentiles for filtering surgery cases generally declined in each percentile group reported in the ACGME statistical reports (10, 30, 50, 70, and 90) from 2009 to 2016 (Table 3). Of note, in 2012–2013 the 10th percentile for filtering procedures was zero and subsequently remained zero. The AUPO statistical reports included 25th and 75th percentile data only. The trend in percentiles from 2008 to 2016, among fellows, was less distinct. The 25th percentile values generally decreased, whereas the 75th percentile values increased (Table 4).
  | Table 3 ACGME resident percentiles for filtering vs shunting cases |
  | Table 4 AUPO glaucoma fellow percentiles for trabeculectomy or express shunt vs aqueous shunt cases |
Shunting surgery
From 2009 to 2016, the total numbers of resident “shunting procedures” performed as a primary surgeon were 1,993, 2,397, 2,702, 2,850, 3,149, 3,136, and 2,980 cases, with average numbers of 4.5, 5.1, 5.7, 6.0, 6.8, and 6.7, and 6.3 cases, respectively (Table 1). This equates to a 40% increase in average shunting procedures, with a 6.5% increase per year (RR =1.065, P<0.001) (Table 2).
For fellows, from 2009 to 2016, the total numbers of “aqueous shunt” procedures were 1,419, 2,486, 1,267, 2,066, 2,334, 2,816, 3,129, and 3,196, and the average numbers were 30.2, 37.1, 35.2, 36.9, 38.9, 44.7, 44.7, and 47.7, respectively (Table 1). This equates to a 57.9% increase in average shunting procedures, with a 5.9% increase per year (RR =1.059, P<0.001) (Table 2).
As with the average trend, the number of shunting procedures for residents generally increased in every percentile group over 7 years. The 10th percentile for shunt surgery was zero in 2009–2010, but increased thereafter (Table 3). For fellows, there was a steady increase in the 25th percentile, with cases increasing from 15 to 26 cases from 2008 to 2016. The 75th percentile for GDI fluctuated but ultimately increased from 43 to 61 cases in 2015–2016 (Table 4).
MIGS and other novel procedures
The ACGME case logs to date do not contain any MIGS or novel procedure categories. Therefore, resident experience with these procedures could not be assessed.
For fellows, the AUPO case logs included ECP, “anterior chamber to Schlemm’s canal shunt,” and “internal shunt (anterior chamber to suprachoroidal space)” procedures. For ECP, the average number of cases fluctuated but ultimately increased from 2.3 cases in 2008–2009 to 5.4 cases in 2015–2016 (Table 5). This represents a 15.5% increase in ECP cases per year (RR 1.155, P<0.001) (Table 2).
Experience with “anterior chamber to Schlemm’s canal shunt” was only reported from 2013 to 2016 but increased from 3.6 to 7 cases over this 3-year period. The median ranged from 0 to 3 cases, 25th percentile was zero each year, and 75th percentile ranged from 3 to 9 cases over the 8-year period. Primary cases of “internal shunt” were minimal, ranging from 0 to 0.7 cases from 2008 to 2016. The median, 25th, and 75th percentiles over all 8 years were zero for “internal shunt” procedures.10 Poisson model analysis of internal shunting data could not be performed due to insufficient data.
Other MIGS procedures, such as trabectome, Cypass microstent, Xen glaucoma implant, and gonioscopy-assisted transluminal trabeculotomy (GATT), are not included in the AUPO fellow case logs and therefore this experience could not be determined.
Discussion
A review of the ACGME resident case logs reveals a declining trend in average filtering surgery experience, with a concurrent increase in average shunting surgery experience. These trends may be a reflection of physician practice pattern shifts, which are possibly influencing training experience.1–6,8 These trends are also supported by and may have been further influenced by the outcomes of the Tube vs Trabeculectomy study.13
For fellows, there was initially a declining trend in trabeculectomy experience from 2008 to 2015, but then increased in 2015–2016. This finding may be attributed to general fluctuation or may be a result of efforts to increase fellow training in this category. The surgical numbers indicate that fellows are still learning and performing trabeculectomies. Conversely, the average resident case numbers for trabeculectomy are in the single digits and decreasing. Every percentile for resident filtering surgery demonstrated a decline from 2009 to 2016. Notably, the 10th percentile for the number of filtering surgeries performed by a resident as a primary surgeon from 2012 to 2016 was zero. This shows that many residents are graduating without having performed a trabeculectomy and suggests that over time if this trend continues, resident surgical experience with filtering surgery may become inadequate. These findings highlight the decreasing role of trabeculectomy in residency education. Based on these findings, ACGME case minimums may need to be re-evaluated and adjusted. If trabeculectomy experience is phased out of residency training, whether intentionally or not, educators may need to consider whether this core skill should be replaced with alternative ones, such as MIGS.
A review of both resident and fellow shunting experience revealed an overall increase in this surgical experience for both groups. Despite the overall increase, the 10th percentile number of resident-performed shunting cases was one case in 2015–2016.9 One possible explanation for this finding is that less emphasis is placed on subspecialty training for residents, which may lead to less glaucoma surgical experience than for fellows. Additionally, emphasis on shunting procedures may not be universally adopted at all programs nationwide, and so some educators still may be performing filtering surgery as their primary procedures. Although this difference is expected between training levels, the lack of glaucoma surgical experience at the resident level may be a deficiency. Residency minimums exist for the purpose of ensuring comprehensive education, and insufficient training will not prepare graduates to function as independent general ophthalmologists. Shortcomings in subspecialty experience may force general ophthalmologists to rely more heavily upon their subspecialty colleagues or may persuade graduates to pursue fellowship training out of concern for inadequate exposure.
To date, MIGSs are not part of the ACGME resident case logs. This does not mean that residents are not exposed to these novel surgeries, but that such experience is presently not tracked or required. At the fellow level, the AUPO case logs demonstrated limited experience with ECP and internal shunts, with ECP experience increasing by 15.5% per year. While average ECP and anterior chamber to Schlemm’s canal shunt cases were in the single digits, the trend for both these categories was upward. Other MIGS procedures such as trabectome, Cypass microstent, Xen glaucoma implant, and GATT are not currently part of the AUPO case logs and therefore surgical experience with these techniques could not be assessed. Although the role of MIGS in residency curricula is debatable, it may be advantageous for fellowship training to equip future glaucoma specialists with skills in the most current technology. It is therefore encouraging to see experience with novel procedures reflected in the fellow case logs, though not yet comprehensive. Expansion of MIGS categories included in the fellow case logs and addition of these categories to the resident case logs should be considered. Minimum requirements may not be necessary for residents, but tracking of this information would be helpful for education purposes.
Limitations of this study include that only 7 and 8 years of data were available, and so we were unable to report on case numbers prior to these dates. Comprehensive MIGS data were also not available, and so we were unable to elucidate on the possible contribution of MIGS to trabeculectomy trends. We also evaluated only trainee experience with cases performed as a primary surgeon and did not analyze data related to assisting in cases. Therefore, this may not fully reflect trainee experience with glaucoma procedures, as trainees may have observed many cases and had meaningful involvement in cases as an assistant. Additionally, the accuracy of the case log data may be limited by trainee reporting, as the data are self-reported. Finally, we recognize that as new devices are emerging, there will be an inherent delay in resident education in these procedures, as attending educators must first receive adequate training in them.
The major strength of this study is that, compared to survey studies that may be limited by response rates, this study provides a comprehensive evaluation of trainee glaucoma surgical experience based on national case log data.
Conclusion
This study represents a comprehensive overview of resident and fellow experiences with glaucoma procedures using publicly available case logs. Over a 7–8-year period, trainee surgical experience with GDI surgery has steadily increased, whereas surgical experience with trabeculectomy has been fluctuating and may be on a downward trend. The AUPO glaucoma fellow minimum surgical requirement as a primary surgeon for “trabeculectomy,” “aqueous shunt,” and “other ab externo procedures” combined is 25 cases, but specific requirements for each category are not set.14 Similarly, the ACGME resident minimum requirement as a primary surgeon for glaucoma surgeries is five cases, but it also does not specify requirements for subcategories.9 Considering the current minimums, the findings of this study suggest that training requirements may need to be re-assessed. Educators should be aware of shifts in trainee surgical experience in order to maintain appropriate training experience.
Acknowledgments
This study was supported by CTSA Grant Number UL1 TR001863 and KL2 TR001862 from the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Disclosure
The authors report no conflicts of interest in this work.
References
Chadha N, Liu J, Teng CC. Resident and Fellow Glaucoma surgical experience following the tube versus trabeculectomy study. Ophthalmology. 2015;122(9):1953–1954. | ||
Chadha N, Liu J, Maslin JS, Teng CC. Trends in ophthalmology resident surgical experience from 2009 to 2015. Clin Ophthalmol. 2016;10:1205–1208. | ||
Gedde SJ, Vinod K. Resident surgical training in glaucoma. Curr Opin Ophthalmol. 2016;27(2):151–157. | ||
Desai MA, Gedde SJ, Feuer WJ, Shi W, Chen PP, Parrish RK. Practice preferences for glaucoma surgery: a survey of the American Glaucoma Society in 2008. Ophthalmic Surg Lasers Imaging. 2011;42(3):202–208. | ||
Vinod K, Gedde SJ, Feuer WJ, et al. Practice preferences for glaucoma surgery: a survey of the american glaucoma society. J Glaucoma. 2017;26(8):687–693. | ||
Ramulu PY, Corcoran KJ, Corcoran SL, Robin AL. Utilization of various glaucoma surgeries and procedures in Medicare beneficiaries from 1995 to 2004. Ophthalmology. 2007;114(12):2265–2270. | ||
Francis BA, Singh K, Lin SC, et al. Novel glaucoma procedures: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118(7):1466–1480. | ||
Arora KS, Robin AL, Corcoran KJ, Corcoran SL, Ramulu PY. Use of various glaucoma surgeries and procedures in medicare beneficiaries from 1994 to 2012. Ophthalmology. 2015;122(8):1615–1624. | ||
AGCME Case Log Statistical Reports for Ophthalmology Residents 2009-2016. Available from: https://www.acgme.org/acgmeweb/tabid/274/DataCollectionSystems/ ResidentCaseLogSystem/CaseLogsStatisticalReports.aspx. Accessed March 11, 2017. | ||
AUPO [homepage on the Internet]. Statistical report: procedures reported by glaucoma fellows in exit survey; 2009–2016. Available from: http://www.aupofcc.org/subspecialties/glaucoma/index.html. Accessed March 11, 2017. | ||
Dean C, Lawless JF. Tests for detecting overdispersion in Poisson regression models. J Am Stat Assoc. 1989;84(406):467–472. | ||
R Core Team (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available from: https://www.R-project.org/. Accessed March 8, 2018. | ||
Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL. Tube versus Trabeculectomy Study Group. Treatment outcomes in the Tube versus Trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol. 2012;153(5):789–803. | ||
AUPO Fellowship compliance committee: program requirements for fellowship education in glaucoma. Available from: https://aupofcc.org/system/files/resources/2017-08/glaucoma_guidelines.pdf. Accessed November 15, 2018. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.