Back to Journals » Clinical and Experimental Gastroenterology » Volume 8
Serum magnesium concentrations in patients receiving sodium picosulfate and magnesium citrate bowel preparation: an assessment of renal function and electrocardiographic conduction
Authors Bertiger G, Jones E, Dahdal D, Marshall D, Joseph R
Received 13 December 2014
Accepted for publication 3 April 2015
Published 28 July 2015 Volume 2015:8 Pages 215—224
DOI https://doi.org/10.2147/CEG.S79216
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Andreas M. Kaiser
Gerald Bertiger,1 Edward Jones,2 David N Dahdal,3 Dennis C Marshall,3 Raymond E Joseph3
1Hillmont GI, Flourtown, PA, USA; 2Delaware Valley Nephrology and Hypertension Associates, Philadelphia, PA, USA; 3Ferring Pharmaceuticals Inc., Parsippany, NJ, USA
Background: We performed a post hoc analysis of two clinical trials to assess whether sodium picosulfate and magnesium (Mg2+) citrate (Prepopik® [P/MC]), a dual-action bowel preparation for colonoscopy, has an impact on serum Mg2+ levels and cardiac electrophysiology. Although rare, hypermagnesemia has been reported in patients consuming Mg2+-containing cathartics, especially patients who are elderly and have renal impairment.
Methods: Data were analyzed from two prospective, Phase III, randomized, assessor-blinded, active-control, multicenter, pivotal studies that investigated split-dose/day-before P/MC. Serum Mg2+ and creatinine clearance (CrCl) were measured at screening, on the day of colonoscopy, and 24–48 hours, 7 days, and 4 weeks after colonoscopy; electrocardiograms also were obtained at these time points.
Results: In total, 304 patients received split-dose P/MC and 294 patients received day-before P/MC. Only 10% of the patients had serum Mg2+ above the upper limit of normal (1.05 mmol/L) on the day of colonoscopy. There was a slight inverse correlation between CrCl and Mg2+ levels on the day of colonoscopy; however, even at the lowest CrCl, serum Mg2+ remained below clinically significant levels of 2.0 mmol/L. Increases in serum Mg2+ were transient, with levels returning to baseline within 24–48 hours, regardless of renal function. No patients with elevated Mg2+ experienced a corrected QT (QTc) interval >500 milliseconds or a QTc interval increase of ≥60 milliseconds from baseline. P/MC had no impact on PR or QRS interval.
Conclusion: P/MC produces little impact on serum Mg2+ levels with no clinically significant effect on cardiac conduction in patients, including those with mild-to-moderate renal impairment.
Keywords: bowel preparation, hypermagnesemia, renal impairment, sodium picosulfate
Introduction
Magnesium (Mg2+), a bivalent cation, plays a vital role in a multitude of biological processes, including membrane stability, muscle contraction, enzymatic function, metabolism, protein/hormone synthesis, and neurotransmission.1–3 Mg2+ is obtained through diet and is absorbed primarily by the small intestine.2 The average daily intake of Mg2+ in the United States is 275 mg.4 Between dietary intake and renal excretion, serum Mg2+ levels are strictly maintained within a narrow range of 0.7–1.05 mmol/L.5
Hypermagnesemia is rare and usually iatrogenic. It occurs occasionally in patients receiving Mg2+-containing parenteral infusions for preeclampsia and eclampsia,2 high doses of calcium or lithium,6,7 or Mg2+-containing cathartics for drug overdose,8–11 and/or in patients with creatinine clearance (CrCl) rates <30 mL/minute who have consumed Mg2+-containing antacids or cathartics.2,3,12–15 Patients with mild-to-moderate renal impairment (CrCl >30 mL/minute but <90 mL/minute) are typically able to compensate for transient increases in serum Mg2+.5 Older patients are generally more susceptible to hypermagnesemia than are younger patients, because of decreases in renal function. Clinical manifestations of hypermagnesemia are concentration-dependent and range from mild nausea/vomiting, bradycardia, and flushing (1.5–2.0 mmol/L) to flaccid paralysis of voluntary muscles, complete heart block, and coma (6–10 mmol/L) (Figure 1).2,12–14,16,17
  | Figure 1 Schematic depicting the onset of clinical manifestations due to hypermagnesemia with increasing serum Mg2+ concentrations. |
Because the use of Mg2+-containing bowel cleansing preparations before colonoscopy have the potential to produce disturbances in electrolytes, caution is advised when used in individuals with renal impairment.5,13,15,16,18–22 Additionally, depending on the severity of these electrolyte disturbances, decreases in cardiac conduction and contractility may be seen.16 With a focus on safety, we analyzed data from two Phase III, active-control, pivotal clinical studies that used sodium picosulfate and Mg2+ citrate (Prepopik® [P/MC]; Ferring Pharmaceuticals Inc., Parsippany, NJ, USA), a nonphosphate, dual-action, low-volume, natural orange-flavored bowel cleansing preparation, for colonoscopy. Post hoc analyses were performed to assess whether 1) patients receiving P/MC in preparation for colonoscopy experience an increase in serum Mg2+ concentrations, 2) there is any correlation between serum Mg2+ concentrations and renal function, and 3) an increase in serum Mg2+ concentration is associated with changes in cardiac conduction or contractility in these patients.
Methods
Patients
Patients aged 18–80 years and undergoing an elective colonoscopy were screened for inclusion into one of two Phase III clinical studies, SEE CLEAR I and SEE CLEAR II (Safety and Efficacy of a Dual-action, Low-volume Bowel Preparation: An Evaluation of Colon Cleansing in Day-before and Split-dose Regimens), that investigated the efficacy and safety of P/MC.23,24 To be eligible, patients needed to have had at least three spontaneous bowel movements per week for 1 month before the scheduled colonoscopy. Patients with renal insufficiency at screening, that is, patients with serum CrCl outside the normal range (45–84 μmol/L for women and 59–104 μmol/L for men) and serum potassium outside the normal range (3.6–5.2 mmol/L) were excluded from the study. Patients also were excluded if they had active inflammatory bowel disease, colonic disease, or gastrointestinal disorders; had undergone prior colorectal or upper gastrointestinal surgery; or had uncontrolled angina and/or myocardial infarction within 3 months before screening, or congestive heart failure, or uncontrolled hypertension. All patients provided written informed consent at screening.
Study design and treatment
This is a post hoc analysis of two prospective, Phase III, randomized, multicenter, active-control, assessor-blinded, pivotal clinical studies that investigated the efficacy, safety, and tolerability of split-dose P/MC (SEE CLEAR I) or day-before P/MC (SEE CLEAR II) compared with conventional day-before 2 L polyethylene glycol (PEG) and two 5 mg bisacodyl tablets (2 L PEG-3350 and bisacodyl tablets; HalfLytely and Bisacodyl Tablets Bowel Prep Kit; Braintree Laboratories, Inc.; Braintree, MA, USA). The Phase III studies were conducted in accordance with the Declaration of Helsinki,25 International Conference on Harmonisation Good Clinical Practice guidelines,26 applicable regulatory requirements, and the institutional review boards at each study site.
A description of the bowel preparations used during the studies has been previously reported.23,24 In brief, patients randomly assigned to receive split-dose P/MC were instructed to reconstitute and drink the first P/MC packet between 5 pm and 9 pm the evening before the colonoscopy. These patients were instructed to consume the second reconstituted packet at least 5 hours, but not more than 9 hours, before the colonoscopy. Patients assigned to receive day-before P/MC were instructed to consume the first reconstituted packet between 4 pm and 6 pm the day before the colonoscopy and to take the second reconstituted packet at least 6 hours later, between 10 pm and 12 am. After consumption of the first P/MC packet, patients were instructed to consume approximately five 8-ounce glasses of clear fluids; after consumption of the second packet, patients were instructed to consume at least three 8-ounce glasses of clear liquids of their choice over the next few hours as per manufacturers instructions. The two packets of P/MC contain a combined 4.2 g of Mg2+.
Assessments
Serum Mg2+ (normal range, 0.7–1.05 mmol/L) and serum creatinine concentrations were measured as part of a full chemistry panel on blood samples obtained at screening, on the day of colonoscopy, and 24–48 hours, 7 days (up to +3 days), and 4 weeks (±5 days) after colonoscopy. Laboratory measurements were performed by a central laboratory (ICON Central Laboratories, Inc.; Farmingdale, NY, USA) with validated methods, and CrCl was estimated with the Cockcroft–Gault method.
Twelve lead electrocardiograms (ECGs) were obtained at screening, on the day of colonoscopy, and 24–48 hours, 7 days (up to +3 days), and 4 weeks (±5 days) after colonoscopy. All ECG measurements were performed by a central ECG laboratory (eResearch Technology, Inc.; Philadelphia, PA, USA) with standard methods. Ventricular rate (beats/minute) was calculated, and the PR, R-R, QRS, and QT interval durations were measured with computer-assisted caliper placement on three consecutive beats in Lead II or an alternative lead if Lead II was not acceptable for measurement. Experienced cardiac safety specialists reviewed all ECGs for correct lead and beat selection, with caliper placement adjudication where necessary. The onset of the QRS complex and the end of the T wave were reviewed to define the QT interval. R-R duration was similarly reviewed, selecting the peak of two consecutive R waves, starting with a previous R wave from the first PQRST complex. Independent parameters, including corrected QT interval using Bazett’s formula (QTcB) or Fridericia’s formula (QTcF), were derived and recorded.
Adverse events (AEs) were recorded throughout the study, coded using version 13.0 of the Medical Dictionary for Regulatory Activities,27 and were based on a patient’s response to questions about his or her health, spontaneous reports, and clinically relevant changes and abnormalities observed by the investigator. A treatment-emergent AE (TEAE) was any AE that began during the treatment period or was a worsening of a preexisting medical condition. The relationship of a TEAE to treatment was assessed by the investigator on the basis of clinical judgment.
Statistical analysis
This analysis was based on the intent-to-treat populations of patients randomly assigned to receive P/MC during the SEE CLEAR studies. Patients were stratified within each P/MC dosing regimen by serum Mg2+ level (normal or abnormal) and by CrCl rate (>90 mL/minute, 60–89 mL/minute, and 30–59 mL/minute). Descriptive statistics were used to describe demographics, baseline characteristics, serum Mg2+ concentrations, and ECG parameters. A simple linear regression model was used to correlate serum Mg2+ concentrations and rate of CrCl.
Results
Patients
A total of 304 patients who received split-dose P/MC and 294 patients who received day-before P/MC were included in this analysis (Table 1). Across both dosing regimens, the mean age was 56 years; approximately 20% of the patients receiving either dosing regimen were aged 65 years or older. Approximately one-third of the patients receiving either dosing regimen had a CrCl <90 mL/minute. Patients with renal insufficiency were excluded from this study; therefore, no patients had a CrCl rate <30 mL/minute. Despite the intake of 4.2 g of Mg2+ with the consumption of P/MC, only 11% of the patients receiving split-dose P/MC and 9% of the patients receiving day-before P/MC had serum Mg2+ concentrations above the upper limit of the normal range (1.05 mmol/L).
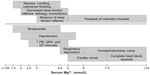
Serum Mg2+ concentrations and rate of CrCl
Individual mean serum Mg2+ concentrations by rate of CrCl on the day of colonoscopy for both dosing regimens are shown in Figure 2. The highest reported serum Mg2+ concentration with either dosing regimen was a transient 1.25 mmol/L (n=2), with the majority of Mg2+ concentrations at or below 1.15 mmol/L (n=266 for split-dose P/MC; n=265 for day-before P/MC). All patients with CrCl <60 mL/minute had serum Mg2+ levels well below the lowest clinically significant Mg2+ concentration known to cause AEs (1.5–2 mmol/L). Among patients who received split-dose P/MC and who had abnormal serum Mg2+ levels on the day of colonoscopy, there was a slight trend for increased serum Mg2+ concentration with decreasing CrCl. However, when posttreatment mean CrCl levels were stratified according to values of 30–59 mL/minute, 60–89 mL/minute, and ≥90 mL/minute and plotted against mean serum Mg2+ levels, no differences were observed on the basis of renal function (Figure 3). Overall, slight-to-moderate renal impairment did not alter serum Mg2+ concentrations among patients receiving P/MC.
Serum Mg2+ concentrations over time
All patients receiving P/MC had serum Mg2+ concentrations within the normal range at screening (split-dose: range, 0.6–1.05 mmol/L; day-before: range, 0.6–1.00 mmol/L), regardless of CrCl (Figure 4). Compared with mean serum Mg2+ concentrations at screening, there was a transient increase on the day of colonoscopy; however, mean serum Mg2+ concentrations returned to baseline levels within 24–48 hours.
Serum Mg2+ concentrations by dosing regimen
Patients following different P/MC dosing regimens could be experiencing different peaks in Mg2+ levels and at different times after dosing. However, when the mean serum Mg2+ levels among patients with abnormal Mg2+ levels on the day of colonoscopy were compared across both dosing regimens, there was no difference in either the peak mean serum Mg2+ concentrations or the time to recovery to baseline levels 24–48 hours later (Figure 5).
Serum Mg2+ concentrations and cardiac assessments
In either study, no patients with elevated Mg2+ levels who received P/MC experienced a QTcB or QTcF interval >500 milliseconds. One patient with normal Mg2+ levels experienced QTcB and QTcF intervals >500 milliseconds; however, these intervals were due to only minimal increases from baseline (<30 milliseconds). During the course of both studies, three patients who received split-dose P/MC and two patients who received the day-before regimen had a QTcB or QTcF interval increase from baseline ≥60 milliseconds. However, all the patients in both studies who had a QT interval increase from baseline ≥60 milliseconds maintained serum Mg2+ levels between 0.6 and 1.0 mmol/L throughout the study. Overall, there were no changes in cardiac function or electrophysiology following either the day-before or split-dose regimen. PR intervals (Figure 6) and QRS intervals (Figure 7) were similar, with overlapping first and third quartile values during the study for patients with normal or elevated serum Mg2+ concentrations on the day of colonoscopy, regardless of dosing regimen. Other cardiac parameters are summarized in Table 2.
Safety
The percentage of patients reporting a TEAE possibly or probably related to the bowel preparation was marginally higher among patients with elevated Mg2+ concentrations on the day of colonoscopy (split-dose: four patients [12%]; day-before: four patients [16%]) compared with those with normal Mg2+ levels on the day of colonoscopy (split-dose: 15 patients [6%]; day-before: 27 patients [10%]). The possibly or probably related TEAEs among patients with elevated Mg2+ concentrations on the day of colonoscopy are listed in Table 3. Only 1 TEAE (mild vomiting) was considered probably related to the bowel preparation. All of the TEAEs possibly or probably related to the bowel preparation were mild or moderate in intensity and were not considered serious AEs. One patient experienced dry throat and throat irritation for a week after colonoscopy; all other TEAEs resolved on the day of or day after the procedure.
Discussion
There have been rare reports of severe, and sometimes fatal, cases of hypermagnesemia after the use of activated charcoal combined with a Mg2+-containing cathartic for the treatment of accidental drug overdose in elderly patients8,11,28 and for intentional drug overdose in younger adults.9,10,16 In all the above case studies, patients had peak serum Mg2+ concentrations of 2.3 mmol/L to as high as 10.65 mmol/L and developed symptoms indicative of hypermagnesemia, including marked hyporeflexia, bradycardia, and/or cardiorespiratory arrest; one of the seven patients in these case studies died.11 In all of these cases, the absolute amount of Mg2+ administered (ranging from 6.6 g administered over 16 hours [0.4 g/hour] to 90 g administered over 18 hours [5 g/hour]) was much greater than the dose in the present studies (4.2 g).8–11,16,28 One patient who died from excessive Mg2+ received a one-time dose of 17.5 g of Mg2+ via an enteral tube.11 In a prospective observational study of 102 patients (without renal disease) who were referred to a statewide-based poison control system after consuming activated charcoal and Mg2+ citrate (mean, 9.2 g Mg2+ over 24–48 hours), the mean serum Mg2+ concentration increased from 0.9 mmol/L at baseline to 1.25 mmol/L.15 Nearly half of the patients had peak Mg2+ concentrations >1.2 mmol/L, the upper limit of normal for the study, and 12 patients had peak Mg2+ concentrations between 1.5 and 2.0 mmol/L.15 This dose was more than double the amount of Mg2+ in the current studies, and the majority of patients’ serum Mg2+ levels remained in the normal range.
Hypermagnesemia has been reported in patients (most often elderly, frail, and with decreased renal function [CrCl <30 mL/minute]) who consumed oral Mg2+-containing cathartics for constipation12,29 or bowel preparation for planned procedures.13,30,31 In a retrospective review of hospital records, Clark and Brown32 described eight cases (out of 19,761 total patients investigated) of hypermagnesemia (2.55–3.62 mmol/L) after ingestion of Mg2+ in elderly patients with gastrointestinal disease that may have altered the mucosal barrier or decreased motility. Recently published UK consensus guidelines for the use of oral bowel preparations state that although Mg2+-containing cathartics present a risk for hypermagnesemia in patients with stage 4 or 5 chronic kidney disease (CKD), Mg2+-containing bowel cleansers are acceptable for patients with early CKD (stages 1–3) and in patients with stage 5 CKD who are receiving hemodialysis.18 Moreover, in patients with stage 4 or 5 CKD who are not receiving hemodialysis, Mg2+-containing cathartics can be used if patients are unable to tolerate the ingestion of the large fluid volumes associated with PEG bowel preparations, although caution should be exercised and Mg2+ levels should be monitored.18
Although there is a concern for hypermagnesemia in patients taking a Mg2+-containing bowel cleanser, specifically those with renal impairment, results of our analysis indicate that minor, transient abnormal concentrations of Mg2+ in patients receiving P/MC for colonoscopy are not clinically significant. In the current studies, serum Mg2+ levels did not reach threshold values (1.5–2.0 mmol/L) where clinical symptoms typically begin, with maximum serum Mg2+ level reaching 1.25 mmol/L in only two patients in either SEE CLEAR study. Our results are similar to those previously reported for P/MC-containing cathartics where significant, but not clinically meaningful, increases (mean increase of 0.063–0.12 mmol/L; P<0.05) in mean peak serum Mg2+ concentrations compared with baseline or a non–Mg2+-containing bowel preparation were reported.19–21,33 Although three patients in one study experienced an increase in serum Mg2+ in excess of 0.25 mmol/L,19 and the maximum increase in serum Mg2+ in another study was reported to be 0.34 mmol/L,33 the maximum serum Mg2+ concentration noted in these reports was <1.2 mmol/L, with no clinical sequelae.19–21
In our analysis, a slight-to-moderate impairment of renal function did not meaningfully affect serum Mg2+ levels. There was a trend for a slight increase in serum Mg2+ concentration with decreasing CrCl, but at CrCl between 30 and 60 mL/minute, serum Mg2+ concentrations also remained well below the 1.5–2.0-mmol/L threshold. Increases in serum Mg2+ concentrations in all patients were transient and returned to baseline within 24–48 hours after colonoscopy. Given the rapid change in Mg2+ concentrations, our data cannot rule out the possibility that Mg2+ concentrations were further elevated in some patients before measurement on the day of colonoscopy. However, similar changes in serum Mg2+ concentrations occurred with both treatment regimens (split-dose or day-before P/MC), and no clinically significant effect on cardiac conduction was observed in patients with elevated Mg2+ concentrations.
Although hypermagnesemia can lead to reduced cardiac contractility,16 our analysis indicates that elevated serum Mg2+ levels found in patients receiving P/MC did not have an untoward impact on cardiac electrophysiology. There were no differences in the PR or QRS intervals between baseline ECGs and the ECGs obtained on the day of colonoscopy among patients experiencing elevated serum Mg2+ or in patients with normal Mg2+ levels on the day of colonoscopy. A QT interval (corrected for heart rate) >500 milliseconds or an increase of ≥60 milliseconds is considered to be predictive of serious adverse drug effects or increased risk for torsades de pointes.34,35 Across both SEE CLEAR studies, only one patient with normal Mg2+ levels experienced a QTcB and QTcF >500 milliseconds, and three patients with normal Mg2+ levels experienced an increase of ≥60 milliseconds. These results indicate that the minimal P/MC-related increases in Mg2+ did not cause any significant cardiac electrophysiologic sequelae.
The percentage of patients reporting a TEAE possibly or probably related to the bowel preparation was slightly higher among patients with elevated Mg2+ concentrations on the day of colonoscopy. However, this result could be expected given the approximately ten fold higher number of patients with normal Mg2+ levels than patients with elevated Mg2+ concentrations on the day of colonoscopy. None of the possibly or probably related TEAEs in the patients with elevated Mg2+ levels on the day of colonoscopy were considered severe, and all but one resolved within 48 hours after colonoscopy (one patient’s dry and irritated throat resolved within 10 days). Moreover, none of the TEAEs in the patients with elevated Mg2+ levels on the day of colonoscopy were considered cardiac disorders. Any changes in ECG among these patients were not considered TEAEs.
Results from this post hoc analysis agree with the recommendations by the UK National Patient Safety Agency, indicating that Mg2+-containing bowel preparations for colonoscopy, such as P/MC, can be used safely in patients with mild-to-moderate renal impairment.18 As always, caution should still be exercised when using any high-volume agents in patients with severe renal impairment. In this analysis of two large-scale, pivotal efficacy and safety studies using split-dose and day-before dosing of P/MC, there were only slight changes in Mg2+ levels in a few patients, with no negative effects on any cardiac measures. Additional studies may be needed to further characterize the risk of hypermagnesemia in elderly patients and in patients with preexisting morbidity. Eleven elderly patients (aged ≥65 years) were included in our analysis; however, the majority of patients in both studies were <65 years old. Additionally, patients with specific gastrointestinal and cardiovascular comorbidities were excluded from both studies. Due to this, it is not clear how well these results extrapolate to patients with prior colorectal surgery, active irritable bowel syndrome, or other disorders that may be associated with alterations of the colonic barrier. A prospective randomized trial is needed to fully identify factors that may predispose patients to a greater risk of developing hypermagnesemia when consuming a Mg2+-containing cathartic.
Conclusion
In patients receiving P/MC to prepare for colonoscopy, serum Mg2+ concentrations generally were not affected by a patient’s level of renal function. An elevation in serum Mg2+ levels was found in a small proportion of patients; however, Mg2+ levels remained well below the threshold for hypermagnesemia symptoms and returned to baseline within 1–2 days. P/MC showed no clinically significant effect on cardiac conduction in patients, including those with mild-to-moderate renal impairment.
Acknowledgments
This study was supported by Ferring Pharmaceuticals Inc., Parsippany, NJ. The authors thank Kelly Cameron, PhD, and Lamara D Shrode, PhD, ISMPP Certified Medical Publication Professional™, of The JB Ashtin Group, Inc., for their assistance in preparing this manuscript for publication based on authors’ input and direction. Editorial support was provided by The Curry Rockefeller Group, LLC. Financial support for editorial assistance was provided by Ferring Pharmaceuticals Inc.
Disclosure
Gerald Bertiger has served as a consultant and has been a part of the speakers bureau for Ferring Pharmaceuticals Inc. Edward Jones serves on the board of directors for CytoSorbents Corporation. David N Dahdal, Dennis C Marshall, and Raymond E Joseph are full-time employees of Ferring Pharmaceuticals Inc. The authors report no other conflicts of interest in this work.
References
Cowan JA. Structural and catalytic chemistry of magnesium-dependent enzymes. Biometals. 2002;15(3):225–235. | |
Rude RK. Magnesium. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, editors. Modern Nutrition in Health and Disease. 11th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2014:159–175. | |
Weisinger JR, Bellorín-Font E. Magnesium and phosphorus. Lancet. 1998;352(9125):391–396. | |
Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, DC: National Academies Press; 1997. | |
Cunningham J, Rodríguez M, Messa P. Magnesium in chronic kidney disease Stages 3 and 4 and in dialysis patients. Clin Kidney J. 2012; 5(Suppl 1):i39–i51. | |
Musso CG. Magnesium metabolism in health and disease. Int Urol Nephrol. 2009;41(2):357–362. | |
Swaminathan R. Magnesium metabolism and its disorders. Clin Biochem Rev. 2003;24(2):47–66. | |
Garrelts JC, Watson WA, Holloway KD, Sweet DE. Magnesium toxicity secondary to catharsis during management of theophylline poisoning. Am J Emerg Med. 1989;7(1):34–37. | |
Gren J, Woolf A. Hypermagnesemia associated with catharsis in a salicylate-intoxicated patient with anorexia nervosa. Ann Emerg Med. 1989;18(2):200–203. | |
Smilkstein MJ, Smolinske SC, Kulig KW, Rumack BH. Severe hypermagnesemia due to multiple-dose cathartic therapy. West J Med. 1988;148(2):208–211. | |
Weber CA, Santiago RM. Hypermagnesemia. A potential complication during treatment of theophylline intoxication with oral activated charcoal and magnesium-containing cathartics. Chest. 1989;95(1):56–59. | |
Kontani M, Hara A, Ohta S, Ikeda T. Hypermagnesemia induced by massive cathartic ingestion in an elderly woman without pre-existing renal dysfunction. Intern Med. 2005;44(5):448–452. | |
Onishi S, Yoshino S. Cathartic-induced fatal hypermagnesemia in the elderly. Intern Med. 2006;45(4):207–210. | |
Rude RK, Singer FR. Magnesium deficiency and excess. Annu Rev Med. 1981;32:245–259. | |
Woodard JA, Shannon M, Lacouture PG, Woolf A. Serum magnesium concentrations after repetitive magnesium cathartic administration. Am J Emerg Med. 1990;8(4):297–300. | |
Jones J, Heiselman D, Dougherty J, Eddy A. Cathartic-induced magnesium toxicity during overdose management. Ann Emerg Med. 1986;15(10):1214–1218. | |
Mordes JP, Wacker WE. Excess magnesium. Pharmacol Rev. 1977; 29(4):273–300. | |
Connor A, Tolan D, Hughes S, Carr N, Tomson C. Consensus guidelines for the safe prescription and administration of oral bowel-cleansing agents. Gut. 2012;61(11):1525–1532. | |
McLaughlin P, Eustace J, McSweeney S, et al. Bowel preparation in CT colonography: electrolyte and renal function disturbances in the frail and elderly patient. Eur Radiol. 2010;20(3):604–612. | |
Rahman A, Vanner SJ, Baranchuk A, Hookey LC. Serial monitoring of the physiological effects of the standard Pico-Salax® regimen for colon cleansing in healthy volunteers. Can J Gastroenterol. 2012;26(7):424–428. | |
Ryan F, Anobile T, Scutt D, Hopwood M, Murphy G. Effects of oral sodium picosulphate Picolax on urea and electrolytes. Nurs Stand. 2005;19(45):41–45. | |
Johnson DA, Barkun AN, Cohen LB, et al; US Multi-Society Task Force on Colorectal Cancer. Optimizing adequacy of bowel cleansing for colonoscopy: recommendations from the US multi-society task force on colorectal cancer. Gastroenterology. 2014;147(4):903–924. | |
Katz PO, Rex DK, Epstein M, et al. A dual-action, low-volume bowel cleanser administered the day before colonoscopy: results from the SEE CLEAR II study. Am J Gastroenterol. 2013;108(3):401–409. | |
Rex DK, Katz PO, Bertiger G, et al. Split-dose administration of a dual-action, low-volume bowel cleanser for colonoscopy: the SEE CLEAR I study. Gastrointest Endosc. 2013;78(1):132–141. | |
World Medical Association General Assembly. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Int Bioethique. 2004;15(1):124–129. | |
Dixon JR Jr. The International Conference on Harmonization Good Clinical Practice guideline. Qual Assur. 1998;6(2):65–74. | |
International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH). Understanding MedDRA: The Medical Dictionary for Regulatory Activities. Geneva: ICH; 2013. Available from: http://www.meddra.org/sites/default/files/page/documents/meddra2013.pdf. Accessed June 16, 2015. | |
Fassler CA, Rodriguez RM, Badesch DB, Stone WJ, Marini JJ. Magnesium toxicity as a cause of hypotension and hypoventilation. Occurrence in patients with normal renal function. Arch Intern Med. 1985;145(9):1604–1606. | |
Gerard SK, Hernandez C, Khayam-Bashi H. Extreme hypermagnesemia caused by an overdose of magnesium-containing cathartics. Ann Emerg Med. 1988;17(7):728–731. | |
Evans MD, Barton K, Pritchard GA, Williams EJ, Karandikar SS. Plasma magnesium should be monitored perioperatively in patients undergoing colorectal resection. Colorectal Dis. 2009;11(6):613–618. | |
Schelling JR. Fatal hypermagnesemia. Clin Nephrol. 2000;53(1):61–65. | |
Clark BA, Brown RS. Unsuspected morbid hypermagnesemia in elderly patients. Am J Nephrol. 1992;12(5):336–343. | |
Hamilton D, Mulcahy D, Walsh D, Farrelly C, Tormey WP, Watson G. Sodium picosulphate compared with polyethylene glycol solution for large bowel lavage: a prospective randomised trial. Br J Clin Pract. 1996;50(2):73–75. | |
Roden DM. Drug-induced prolongation of the QT interval. N Engl J Med. 2004;350(10):1013–1022. | |
Shah RR. The significance of QT interval in drug development. Br J Clin Pharmacol. 2002;54(2):188–202. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.