Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 8
Seroprevalence of human immunodeficiency virus among voluntary counseling and testing clients at the University of Gondar Teaching Hospital, Northwest Ethiopia
Authors Sinku Y, Gezahegn T, Gashaw Y, Workineh M , Deressa T
Received 11 April 2016
Accepted for publication 17 June 2016
Published 16 August 2016 Volume 2016:8 Pages 135—140
DOI https://doi.org/10.2147/HIV.S110337
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Yohannes Sinku,1,2 Takele Gezahegn,1 Yalewayiker Gashaw,1 Meseret Workineh,1 Tekalign Deressa1
1School of Biomedical and Laboratory Sciences, College of Medicine and Health Sciences, University of Gondar, 2Diagnostic Laboratory Case Team, University of Gondar Teaching Hospital, Gondar, Ethiopia
Background: The epidemiology of human immunodeficiency virus (HIV) infection in Ethiopia varies with regions, study population, and time. Thus, timely information on HIV epidemiology is critical for the combat of the epidemic. In this study, we aim to update HIV prevalence and risk factors among voluntary counseling and testing (VCT) clients at the University of Gondar Teaching Hospital, Northwest Ethiopia.
Methods: A total of 2,120 VCT clients’ records from September 2007 to August 2010 were analyzed retrospectively. Bivariate logistic regression analysis was used to identify significant predictors. Odds ratio (OR) and 95% confidence intervals (CIs) were calculated. Statistical significance was set at P-value <0.05.
Results: Of 2,120 VCT clients, 363 (17.1%) were seropositive for HIV. A higher rate of HIV positivity was observed among female clients (20.4%) than that in male clients (14.0%) (OR 1.58, 95% CI 1.26–1.98, P=0.00). Widowed (95% CI 10.42–34.92, P=0.00), married (95% CI 3.42–5.94, P=0.00), divorced (95% CI 2.79–5.32, P=0.00), and illiterate (95% CI 2.33–5.47, P=0.00) clients were associated with HIV infection with the odds ratios of 19.07, 4.51, 3.85, and 3.57, respectively. Clients within the age category of 35–49 years (OR 5.03, 95% CI 3.56–7.12, P=0.00) and above the age of 50 years (OR 4.99, 95% CI 2.67–9.34, P=0.00) were more likely to be infected with HIV.
Conclusion: HIV is still the major concern of public health in the Gondar area as evidenced by our data. Being female, widowed, married, illiterate, and older age were the identified risk factors for HIV infection. Thus, consideration of these factors in future intervention and clinical practice is recommended.
Keywords: HIV, AIDS, voluntary counseling and testing, prevalence, Northwest Ethiopia
Introduction
The human immunodeficiency virus (HIV) pandemic continues to be a major public health threat in the world. Since its recognition, HIV has claimed >34 million lives worldwide and ˜36.9 million people were living with HIV by the end of 2014.1 Sub-Saharan Africa accounts for 70% of the world HIV/AIDS infections and deaths. Ethiopia is one of the sub-Saharan African countries most affected by the HIV pandemic. The adult prevalence of HIV was estimated to be 0.2% in 1985, 3.2% in 1995, and 4.4% in 2003.2–4 Trend analysis of national HIV prevalence rate reveals a gradual rise until the late 1990s and a decline after 2000.2–5 In 2014, the number of people living with HIV was estimated to be 769,600, with 15,700 new HIV infections and 35,600 AIDS-related deaths.6 According to this report, annual new HIV infections and AIDS-related deaths have been declined by 90% and 53%, respectively, between 2000 and 2011, due to expansion of HIV counseling and testing, care, and treatment services.
Despite the significant drop of HIV prevalence in the country, studies show that there is remarkable heterogeneity with geographic regions, study populations, and the period of study.7–11 Further, factors that sustain disparities in HIV prevalence and fueling the epidemic such as high-risk sexual behaviors, low education, limited access to health service, the social stigma surrounding HIV, and poverty are still highly prevalent among the population of Ethiopia.12–14 Furthermore, many of HIV-infected people do not know about their status, and a significant number of the population remain uninformed or misinformed about the cause, transmission, and preventive measures.15–17 Therefore, there is a pressing need for continuous monitoring and analysis of existing data to generate pragmatic evidence to explain the basis of the prevalence and variations. Such strategies are useful for identification of more vulnerable population groups and to design interventions focusing on those who are at more risk of acquiring HIV infection.
HIV counseling and testing is the key entry point to prevention, care, treatment, and support services, where people learn their HIV status and its implications to make informed decisions about their health.8,12,15 Voluntary counseling and testing (VCT), provider-initiated testing and counseling, and mandatory HIV screening are the three types of HIV tests being used in Ethiopia.18 VCT continues to be a cornerstone for HIV prevention and care services in the country. It increases clients’ perception of their vulnerability to HIV, promotes behavioral changes, facilitates early referral for care and support, and assists in reducing social stigma. Furthermore, data from VCT clients have been used as important sources of information for estimating HIV prevalence and determinants of the epidemic.18,19
Although information on HIV prevalence among different segments of population is available,8–12 data on prevalence of this infection among VCT clients from the Gondar area are scarce. Thus, we sought to fill this gap by updating the prevalence of HIV infection among VCT clients who attended the University of Gondar Teaching Hospital in 3 consecutive years and to identify the sociodemographic determinants for HIV seropositivity.
Materials and methods
Study design, settings, and population
A retrospective study was conducted at the University of Gondar Teaching Hospital, Gondar, Northwest Ethiopia, to determine the prevalence of HIV infection and the associated risk factors among VCT clients between September 2007 and August 2010. Gondar is located at 737 km from the country’s capital Addis Ababa in North Gondar zone of the Amhara regional state. The town has latitude and longitude of 120361N and 370281E, respectively, and an elevation of 2,133 m above sea level. Gondar is a capital of North Gondar Zone with urban population of ˜227,100 in 2007.20
The University of Gondar Hospital is a tertiary-level teaching and referral hospital with 450 beds for inpatients and provides referral health services for >5 million inhabitants in Northwest Ethiopia. The hospital also has a VCT clinic, where clients from Gondar town and surrounding areas receive VCT for HIV free of any charges.
Determination of HIV infection
HIV infection was detected by rapid HIV test kits as per the national algorithm for HIV testing. Briefly, sera prepared from venous blood/whole blood were screened for HIV using a KHB diagnostic kit (Shanghai Kehua Bio-Engineering Co. Ltd, Shanghai, People’s Republic of China). Reactive samples were confirmed by Stat-Pack (Chembio Diagnostics, Medford, NY, USA) and Uni-Gold kits (Trinity Biotech, Wicklow, Ireland) according to the national algorithm for HIV testing.
Data collection
Data were collected from the VCT registration book. Data with missing values with respect to the study variables were omitted. Sociodemographic variables such as age, sex, residence, education status, and clinical characteristics such as HIV serostatus were collected.
Statistical analysis
Data analysis was performed using SPSS Version 20 statistical package (IBM Corporation, Armonk, NY, USA). Data were summarized using frequencies and proportions to describe the study population in relation to relevant variables. Bivariate analysis was used to identify significant predictors. The degree of association between independent and dependent variables was assessed using odds ratio (OR) with 95% confidence interval (CI). P-value <0.05 was considered as statistically significant.
Ethical considerations
Ethical clearance for this study was obtained from the School of Biomedical and Laboratory Sciences (SBMLS), University of Gondar. A permission letter was also obtained from the Hospital Laboratory head prior to data collection. The ethics review committee of SBMLS did not require written informed consent to be obtained from all patients, as this was retrospective study, and all data was anonymous and handled confidentially.
Results
Characteristics of the study participants
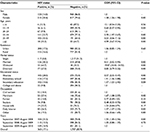
A total of 2,120 clients’ data were retrieved from VCT registries of the University of Gondar Teaching Hospital. Of the 2,120 VCT clients, 1,093 (51.6%) were males and 1,027 (48.4%) were females, giving a male-to-female ratio of 1.06:1. The median age of the study subjects was 23.0 years (interquartile range ±10). 1,188 (56%) of the clients were from urban areas; and >80% of the participants had elementary education and above. In terms of their marital status, 1,334 (62.9%) were never married, followed by married (21.2%), divorced (13.4%), and widowed clients (2.4%). A little over one-third of the VCT clients (36.7%) were students, 316 (14.9%) were daily laborers, and 282 (13.3%) were government employees (Table 1).
Prevalence of HIV infection among the study subjects
Overall, 17.1% (363/2,120) of the study participants were found to be HIV positive (Table 2). Higher rates of HIV positivity were observed among female clients (20.4%) than males (14.0%) (OR 1.58, 95% CI 1.26–1.98, P=0.00). The prevalence of HIV was higher among the participants in the age group of 35–49 years (35.5%), followed by >50 years (35.3%) and 20–24 years (22.7%). In terms of their marital status, higher rates of HIV positivity were observed among widowed (64.7%) and married participants (30.2%). The prevalence of HIV among VCT clients showed an inverse relationship with their education level, with a higher HIV rate among illiterates (28.0%) than among educated ones. With respect to occupations of the clients, higher HIV rates of positivity were detected among merchants (27.4%), daily laborers (26.3%), and housewives (25.7%) compared to that among other occupations. Year-specific HIV-positive rates were 25.2%, 15.5%, and 14.9% in the years 2007/2008, 2008/2009, and 2009/2010, respectively.
Bivariate analysis revealed that widowed (95% CI 10.42–34.92, P=0.00), married (95% CI 3.42–5.94, P=0.00), divorced (95% CI 2.79–5.32, P=0.00), and illiterate clients (95% CI 2.33–5.47, P=0.00) were associated with HIV infection, with the odds ratios of 19.07, 4.51, 3.85, and 3.57, respectively. Clients within the age category of 35–49 years (OR 5.03, 95% CI 3.56–7.12, P=0.00) and over the age of 50 years (OR 4.99, 95% CI 2.67–9.34, P=0.00) were more likely to be infected with HIV.
Discussion
HIV/AIDS continues to be a major public health challenge in the world, despite the major efforts and resources allocated to combat the epidemic. Interventions such as HIV counseling and testing service has been shown to reduce HIV prevalence by promoting safer sexual behavior and serving as a key entry point for HIV treatment and care. Ethiopia has shown an encouraging improvement in the expansion of VCT centers and antiretroviral therapy programs over the past decade that has reduced HIV prevalence at the national level.2–5,10 Nevertheless, HIV epidemiology in the country varies markedly in terms of prevalence and risk factors from place to place. Therefore, accurate and timely data on the local epidemiology of HIV are a necessity to identify at-risk groups and to tailor intervention strategies accordingly. To this end, our study sought to update the prevalence and associated risk factors for HIV seropositivity among VCT clients at the University of Gondar Teaching Hospital.
The overall prevalence of HIV observed in our study was 17.1%. This was higher than the 13.7% VCT-based national prevalence rate21 and 13.4% rate in Burie, Ethiopia.22 Yet, it was lower than the previously reported 25.4% rate from Gondar,8 24.5% rate in Addis Ababa, Ethiopia,23 and 24.6% in Tanzania.24 The variability in HIV prevalence across the studies and our finding could be explained by differences in sociodemographics of the study participants and prevailing HIV risk factors in the study areas. HIV prevalence rates were declining over the study period, albeit the increasing trend in VCT uptake. This was in agreement with the declining trends of HIV prevalence among the general population of Ethiopia and different segments of populations in the country.7,8,11 However, it is not clear whether this decline could be related to the general declining trend of HIV in the country as this is not a community-based study.
Analysis of sociodemographic characteristics revealed higher HIV prevalence among females than males. This observation was in line with a number of previous studies including the national demographic and health survey that reported higher HIV positivity rate among females.7,8,10 This could be ascribed to biological, cultural, sexual violence, and economic disadvantages related to their sex. Similarly, widowed and married clients were more likely to be infected with HIV than unmarried ones. This might be partly attributed to the prevalent extramarital sex or successive marriages in the area. Another possible reason that explains the high HIV prevalence among this group is that married/widowed clients often seek VCT service upon developing symptoms that suggest HIV infection. However, this issue remains to be a subject of further investigations to understand the contextual influences of couples’ relationship and behaviors on their health and to design tailored intervention methods.
This study found that clients above the age of 35 years are at about five times at higher risk of being infected with HIV than the younger ones. This finding was in agreement with previous studies.23,25 Presumably, younger people may be less likely to acquire HIV infection due to the significant reduction in new HIV infections as a result of expanded interventions and HIV testing and care services in the country.6 However, the reason behind the high HIV rate among older age group is not clear. It appears that older age groups are more likely to be married, divorced, or widowed (which are found to be risk factors for HIV in this study), which could explain the higher prevalence in these groups. This study also identified higher likelihood of HIV infection among illiterates than educated clients, which was consistent with the report of Ethiopian health and demographic survey.7 This suggests that an insufficient awareness regarding HIV transmission and prevention could be the drivers for the seropositivity among this group of the population.
The results of this study were solely derived from records of VCT clients; thus, our inferences are subject to some limitations. Key variables such as clients’ socioeconomic status, risk behavior, number of sexual partners, and awareness of HIV transmission and prevention methods were missing. Nevertheless, our data provide useful information regarding HIV prevalence and risk factors among VCT clients in the Gondar area.
Conclusion
HIV is still the major public health concern in the Gondar area as evidenced by our data. Being female, widowed, married, illiterate, and of older age were found to be associated with higher likelihood of HIV infection. Thus, concerted efforts and intervention strategies that target these at-risk populations are recommended.
Acknowledgment
The authors would like to acknowledge the Gondar University Teaching Hospital physicians, VCT counseling nurses, and laboratory staff for their unreserved support during data collection.
Disclosure
The authors report no conflicts of interest in this work.
References
WHO [webpage on the Internet]. HIV/AIDS Factsheet. Available from: http://www.who.int/mediacentre/factsheets/fs360/en/. Accessed December 16, 2015. | ||
MoH. National Technical Guideline. Integrated Disease Surveillance and Response. Addis Ababa, Ethiopia: MoH; 2002. | ||
Central Statistical Agency (Ethiopia) and ORC Macro. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia and Calverton, MD: Central Statistical Agency and ORC Macro; 2005. | ||
World Health Organization: the WHO Country Office for Ethiopia and the WHO Regional Office for Africa. Summary Country Profile for HIV/AIDS Treatment Scale-Up; 2005. Available from: www.who.int/3by5. Accessed April 12, 2016. | ||
Federal HIV/AIDS Prevention and Control Office. Report on Progress towards Implementation of the UN Declaration of Commitment on HIV/AIDS. Federal Democratic Republic of Ethiopia: Federal HIV/AIDS Prevention and Control Office; 2010. | ||
World Health Organization: the WHO Country Office for Ethiopia [webpage on the Internet]. HIV/AIDS progress in 2014. Available from: http://www.afro.who.int/en/ethiopia/country-programmes/topics/4480-hivaids.html. Accessed May 23, 2016. | ||
Ethiopia Central Statistical Agency and ICF International. Ethiopian Demographic and Health Survey. Addis Ababa, Ethiopia; Calverton, MD: Ethiopia Central Statistical Agency; ICF International; 2012. | ||
Alemie GA, Balcha SA. VCT clinic HIV burden and its link with HIV care clinic at the University of Gondar Hospital. BMC Public Health. 2012;12:1010. | ||
Endris M, Deressa T, Belyhun Y, Moges F. Seroprevalence of syphilis and human immunodeficiency virus infections among pregnant women who attend the University of Gondar Teaching Hospital, Northwest Ethiopia: a cross sectional study. BMC Infect Dis. 2015;15:111. | ||
Tessema B, Yismaw G, Kassu A, et al. Sero-prevalence of HIV, HBV, HCV and syphilis infections among blood donors at Gondar University Teaching Hospital, northwest Ethiopia: declining trends over a period of five years. BMC Infect Dis. 2010;10:111.9. | ||
Moges F, Kebede Y, Kassu A, et al. Seroprevalence of HIV, HBV infections and syphilis among street dwellers in Gondar city, northwest Ethiopia. Ethio J Health Dev. 2006;20:160–165. | ||
Berhane Y, Wuhib T, Sanders E, et al. HIV/AIDS. In: Berhane Y, Hailemariam D, Kloos H, editors. The Epidemiology and Ecology of Health and Disease in Ethiopia. Addis Ababa, Ethiopia: Shama Books; 2006:446–474. | ||
Arthur G, Nduba V, Forsythe S, Mutemi R, Odhiambo J, Gilks C. Behaviour change in clients of health centre-based voluntary HIV counselling and testing services in Kenya. Sex Transm Inf. 2007;83(7):541–546. | ||
MOH/HAPCO, AAU, CSA, and EPHA. HIV/AIDS Behavioral Surveillance Survey (BSS) Ethiopia: Round Two. Addis Ababa, Ethiopia: MOH/HAPCO, AAU, CSA, and EPHA; 2005. | ||
Joint United Nations Panel on HIV/AIDS (UNAIDS). UNAIDS Terminology Guidelines – Revised Version. Geneva: UNAIDS; 2011. | ||
Joint United Nations Panel on HIV/AIDS (UNAIDS). AIDS Epidemic Update. Geneva: UNAIDS; 2007. | ||
Admassu M, Fitaw Y. Factors affecting acceptance of VCT among different professional and community groups in North and South Gondar Administrative zones, North West Ethiopia. Ethio J Health Dev. 2006;20(1):24–30. | ||
Federal Ministry of Health: Federal HIV/AIDS Prevention and Control Office. Guidelines for HIV Counselling and Testing in Ethiopia. Addis Ababa: Federal Ministry of Health; 2007. | ||
World Health Organization. A Guide to Monitoring and Evaluation for Collaborative TB/HIV Activities. Geneva: Stop TB Department and Department of HIV/AIDS, WHO; 2004:14. | ||
Comission FPC. Summary and Statistical Report of the 2007 Population and Housing Census of Ethiopia. Addis Ababa: CSA; 2008:57–60. | ||
Federal Ministry of Health/National HIV/AIDS Prevention and Control Office. AIDS in Ethiopia. Addis Ababa: MOH Sixth Report; 2007. | ||
Biadglegne F, Belyhun Y, Tessema B. Sero-prevalence of human immunodeficiency virus among voluntary counseling and testing clients in Burie Health Center, West Gojjam, Ethiopia. Ethiop Med J. 2010;48(2):149–156. | ||
Antenane K, Mebiratu B, Solomon T. Socio-demographic profile and prevalence of HIV infection among VCT clients in Addis Ababa. Ethiop J Health Dev. 2005;19(2):109–116. | ||
Mossdorf E, Stoeckle M, Vincenz A, et al. Impact of a national HIV voluntary counselling and testing (VCT) campaign on VCT in a rural hospital in Tanzania. Trop Med Int Health. 2010;15(5):567–573. | ||
Mulugeta E. Socio demographic characteristics, sexual behavior, and reasons for attending VCT service at Bethzatha VCT project; EPHA; 2003:5. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.