Back to Journals » Patient Preference and Adherence » Volume 11
Self-reported adherence and associated factors to isoniazid preventive therapy for latent tuberculosis among people living with HIV/AIDS at health centers in Gondar town, North West Ethiopia
Authors Ayele AA , Asrade Atnafie S , Balcha DD, Weredekal AT, Woldegiorgis BA, Wotte MM, Gebresillassie BM
Received 30 December 2016
Accepted for publication 14 March 2017
Published 10 April 2017 Volume 2017:11 Pages 743—749
DOI https://doi.org/10.2147/PPA.S131314
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Asnakew Achaw Ayele,1 Seyfe Asrade Atnafie,2 Demis Driba Balcha,1 Asegedech Tsegaw Weredekal,2 Birhanu Alemayehu Woldegiorgis,1 Mulgeta Melaku Wotte,1 Begashaw Melaku Gebresillasie1
1Department of Clinical Pharmacy, 2Department of Pharmacology, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Purpose: This study aimed to assess self-reported adherence and associated factors to isoniazid preventive therapy (IPT) for latent tuberculosis among people living with HIV/AIDS (PLWHA) at health centers in Gondar town, North West Ethiopia.
Patients and methods: An institution-based prospective cross-sectional study was conducted from March 10 to June 11, 2016. A total of 154 eligible participants were included in the study, using the simple random sampling method, from the available four health centers and one teaching referral hospital that provided antiretroviral therapy (ART) for HIV/AIDS patients. Adherence was measured by self-report of isoniazid (INH) tablets taken for the preceding 7 days. Participants were recruited through in-depth interviews. The collected data were entered and analyzed using the statistical packages for social sciences (SPSS) version 20.
Results: The adherence level to IPT was 90.3% for the last 7 days of the study. ART was initiated for 84.4%, and all of them were on a first-line regimen. Isoniazid-related side effects were reported by 48 (31.2%) participants, of which the most commonly identified were abdominal pain, vomiting, skin rash, jaundice, and numbness. Only 3 (2%) participants discontinued from the study. In the bivariate logistic regression analysis, respondents who had received an explanation about IPT were 83% times more likely to be adherent compared to those who had not received it (95% CI, AOR: 0.266 [0.23–3.127]). Respondents who had taken IPT for ≥5 months were more likely to be adherent than those who had taken it for 1–2 months [95% CI, COR: 1.484]. On the other hand, respondents who experienced side effects were 36% less likely to be adherent compared to those who did not experience any.
Conclusion: The level of adherence to IPT among PLWHA was high. Among the predictors reported, carelessness and/or forgetfulness, side effects, and absence from home were the major factors identified for being nonadherent. Health professionals and the Ministry of Health should design and deliver appropriate health education tips and messages. Moreover, counseling of patients who are in their first 2 months of therapy should be strengthened further.
Keywords: adherence, isoniazid, preventive therapy, HIV/AIDS, side effects
Introduction
Tuberculosis (TB) is the leading and most common opportunistic infection and cause of mortality in people living with HIV/AIDS (PLWHA). The risk of developing TB among PLWHA is 21–34 times greater than among those without HIV infection.1
The interaction between TB and HIV/AIDS is bidirectional, with each disease potentiating the adverse effects of the other. This, in turn, affects the prognosis of patients and complicates clinical diagnosis and management plans through unusual presentation of symptoms, adverse drug reactions, drug–drug interactions, and overlapping drug toxicities between anti-TB drugs and highly active antiretroviral therapy.2–4 Coinfection with TB and HIV/AIDS contributes significantly to the burden on health systems in the developing world and complicates and thwarts efforts aimed at achieving globally set development and health objectives.2–5
Among the collaborative TB/HIV activities by World Health Organization (WHO) is to have 100% coverage of isoniazid preventive therapy (IPT) for PLWHA attending HIV care services among those eligible by 2015.6,7
IPT is the provision of the drug called isoniazid to people at high risk of developing active tuberculosis.8 The current recommended dose of IPT for adults is 300 mg of isoniazid per day for 6 months, with 36 months conditionally recommended in areas of high TB prevalence and transmission.8 Adolescents and adults living with HIV/AIDS should be screened with the WHO checklist for TB symptoms to rule out active TB infection. Those reporting one or more symptoms might have active TB and should be further evaluated and then either treated for TB or, if active TB is ruled out, placed on IPT. Those reporting none of the symptoms should also be placed on IPT.9
To counter the incidence of TB/HIV coinfection, which is about 27.7% in the Amhara region, Ethiopia has developed strategies for TB/HIV collaborative activities since 2002. However, no published explanations have defined the role of these collaborative efforts in strengthening linkages between HIV/AIDS and TB management units at the point-of-care level; this supports the rates of HIV testing and linkage to cotrimoxazole preventive therapy being higher than screening HIV positives for TB, initiation of IPT, linkages, referral, and TB diagnostic capacity.10,11
In 2011, WHO recommended that patients infected by HIV/AIDS in resource-limited settings should be placed on IPT in order to reduce the incidence of TB.8
Studies on IPT delivery have revealed variable rates of acceptance of and adherence to TB preventive therapy among populations at risk for TB. The overall adherence rate for IPT was only 45% in a 2010 study among patients attending chest clinics in New York City.12 On the other hand, the IPT completion rate among HIV-infected patients with a positive tuberculin skin test (TST) who had counseling and transport reimbursement was 87% in a study done in Dar es Salaam, Tanzania.13 Adherence to IPT in TST-positive and non-TST-screened HIV-infected subjects in Thailand was 84.5 and 79.7% by self-reporting, and 81.8 and 73.9% by pill count monitoring.14 In 2014, a study on IPT adherence rate reported 86.5% of adherence in 1 month among HIV-infected patients in Ethiopia.10
Good adherence to IPT has been attributed to counseling before initiation of therapy, regular attendance at follow-up clinics, and freedom to take INH publicly.11 Other factors shown to affect IPT adherence among HIV-infected patients include beliefs about INH safety, understanding of IPT rationale, and concerns about potential INH side effects. Moreover, patient denial of HIV infection, concerns regarding concurrent use of highly active antiretroviral therapy, and HIV/AIDS-related stigma are also relevant.15,16 Directly observed preventive therapy and shorter-duration regimens for preventive therapy have both been found to improve treatment adherence rates.17 Barriers to the implementation of IPT have been found to be connected to both patient factors, as mentioned earlier, and health care system factors.18
Several studies reported that nonadherence to therapy is the principal problem in the control of TB in developing countries. The dual infection of HIV/AIDS and tuberculosis presents further adherence problems because of adverse effects and high pill burden. Adherence to therapy is the key to success.11,19,20
The evidence generated from this study is crucial to provide a basis for possible TB/HIV program interventions and the management of nonadherence to IPT. Therefore, the aim of this study was to assess self-reported adherence and associated factors to IPT for latent TB among PLWHA at health centers in Gondar town, North West Ethiopia.
Materials and methods
Study design and setting
An institution-based prospective cross-sectional study was conducted at health centers located in Gondar town. The town has one referral and teaching hospital, one private general hospital, nine health centers, and many private clinics. Of these, only four health centers and one referral and teaching hospital are providing ART medications to the patients.
Sample size determination and sampling procedure
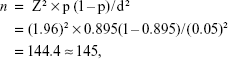
The sample size was determined by using a single mean formula.21
|
where n = the required number of sample size
Z = the standard normal distribution designed 95% confidence, usually Z =1.96
p = percentage of patient adherence rate of IPT from previous study in Ethiopia, which is 0.895
d = degree of accuracy, usually 5%.
Expecting an overall adherence rate of 89.5% at a 95% confidence interval, and after adding 5% of the calculated sample size for possible nonresponse, 154 patients were interviewed. All the four health centers and one referral and teaching hospital that are providing ART medications were included in the study. Then the number of patients to be included in the study from each health center and referral hospital was calculated on the basis of the average daily patient flow to each, and this was used to proportionally allocate the calculated total sample size to the health centers and referral hospital. The study was conducted during the period March 10 to June 11, 2016, and all patients who fulfilled the inclusion criteria and were available during the study period were included in the analysis.
Operational definitions
Nonadherence
Failed to take >80% or missed ≥ two doses of INH pills prescribed in the last 7 days (1 week) prior to the interview.
Adherence
Able to take ≥80% of the prescribed INH pills in the last 7 days (1 week) prior to the interview.
Carelessness: lack of attention or consideration.
Data collection and management
The data collection tool used in the study was adopted from previous studies and prepared in English. This was translated into the Amharic local language and then back into English to ensure that the translated version gave the proper meaning. The data collection instrument was pretested on 10 patients who were not included in the final analysis, and relevant modifications were instituted before the commencement of actual data collection. The data were collected by four principal investigators through interviewer-administered questionnaires and face-to-face interviews by explaining what the questions meant to those who were unable to read and/or write. The investigators who collected the data were trained in using the instrument and in approaching the patients and securing their permission for interviews prior to the data collection process.
Data entry and analysis
The data collected using the quantitative method were cleaned, entered, and analyzed using IBM SPSS Statistics for Windows, version 20.0 (Armonk, NY, USA). In this study, sociodemographic characteristics, levels of adherence, and associated factors were described using frequencies, percentages, mean, and standard deviation (SD). Binary logistic regression was employed to assess the factors associated with adherence, and P-values of less than 0.05 and 95% confidence intervals (CI) were used as cutoff points to determine the statistical significance of associations among different variables.
Ethical consideration
Ethical approval was obtained from the research and ethics review committee of the School of Pharmacy, University of Gondar, to conduct the study. Written informed consent was also obtained from each respondent after the purpose of the study had been explained. They were also informed that participation was voluntary and they could withdraw from the study at any stage if they desired. Participants’ confidentiality was guaranteed by not recording their personal identifiers on the questionnaire.
Results
Sociodemographic characteristics of respondents
All the 154 interview guides/questionnaires of the sample were included in the analysis, making the response rate 100%. The participants had a mean age of 37.7 years and an SD of 8.97 years. Nearly half (48.1%) of the participants were females, and about 2.7% were pregnant. The majority (93.5%) of the respondents were Amhara by ethnicity and Orthodox Christian religion followers (90.3%). More than two-thirds (68.2%) of the participants had completed their primary education and lived in families of five or fewer members (76.6%). About one-third (29.2%) of the participants were self-employed and spent an average of 15–30 minutes to reach the health centers (68.2%) (Table 1).
About one-third (31.2%) of the participants experienced INH-associated adverse drug reactions (ADRs), of which abdominal pain, vomiting, skin rash, jaundice, and numbness were the most commonly identified. More than one-third (38.3%) of the participants drank alcohol while they were on medication; among these, 13% of them drank up to 3 units of alcohol 2–3 times per week.
Patients report on adherence and associated factors
About 84.4% of the patients were on IPT-initiated ART, all of whom were on first-line ART regimen. INH-related common side effects were reported by 48 (31.2%) of the participants, of which abdominal pain, vomiting, skin rash, jaundice, and numbness were the most commonly identified. Among the participants who experienced one or more of the above symptoms, only 3 (2%) discontinued INH, which showed that most who had mild abdominal pain and vomiting continued taking INH. In terms of occupation, the maximum percentage of nonadherence was observed among government employees, merchants, and servants (Table 2).
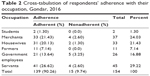  | Table 2 Cross-tabulation of respondents’ adherence with their occupation, Gondar, 2016 |
The level of self-reported adherence rate of IPT was found to be 90.3% with 95% CI (86.1–92.3). In the bivariate logistic regression analysis, respondents who did not receive any explanation about IPT had 83% lower odds of being adherent compared to those who received an explanation [95% CI, AOR: 0.266 (0.23–3.127)]. Respondents who took IPT for ≥5 months were more likely to be adherent than those who took it for 1–2 months [95% CI, COR: 1.484]. On the other hand, respondents who experienced side effects had 36% lower odds of being adherent compared to those who experienced none (Table 3).
Reasons for nonadherence
The most frequently mentioned reasons for being nonadherent were carelessness and forgetfulness (33%), side effects (20%), and being away from their residential areas or homes (20%) (Figure 1).
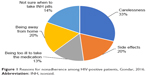  | Figure 1 Reasons for nonadherence among HIV-positive patients, Gondar, 2016. |
Discussion
This study attempted to assess the level of IPT adherence and the available evidence regarding factors that hinder adherence to TB preventive therapy among PLWHA in selected health centers located in Gondar town. The study found an adherence rate of 90.3%, which was in agreement with the adherence level reported from a study conducted in Addis Ababa (89.5%).10 However, it was higher than the level of adherence reported from South Africa, which was 72%.22 This might be because the level of adherence in the South African study was measured by the more objective method, called the Arkansas method, which is laboratory based (biochemical test). About 90.3% of the study participants had taken at least 80% of their prescribed isoniazid doses in the 7 days prior to the study. This was similar to the findings of studies done in Addis Ababa, Diredawa, and Cambodia, where the levels were 89.5%, 86%, and 86.5%, respectively.10,23,24
Among the reasons for good adherence, explanation and counseling about IPT and TB secondary to HIV/AIDS was a major one, and most of the adherent participants had a good understanding of the benefits of IPT from their health providers. This means that providing sound counseling periodically on the importance of IPT and adherence will lead to the required knowledge and understanding. Associated with this, some of them thought that isoniazid is effective in reducing or lowering blood HIV viral load or concentration, and in preventing other HIV/AIDS-related complications.
In the binary logistic regression analysis, patients who took IPT for ≥5 months were more likely to be adherent than those who took it for about 1–2 months. A similar finding was reported by the study conducted in Addis Ababa.10 This was probably because the repeated counseling services that the patient got from the health facilities during their long follow-up period made them more adherent.
Among the reasons for nonadherence, carelessness and forgetfulness (33%) to take medication was the major reason followed by experiencing ADRs (20%) and being away from home (20%). While taking the medication, some of the patients experiencing ADRs stopped taking the medication. This could be because the ADRs were not minor or self-limited and because some, like acute hepatitis, tingling, and numbness (associated peripheral neuropathy), were not effectively controlled. Along with this, a guideline developed in South Africa for treatment of TB also recommends that in cases of mild peripheral neuropathy, pyridoxine (vitamin B6) must be given and increased from 25 mg to 100 mg daily until the symptoms disappear. If the peripheral neuropathy is severe or worsens, then isoniazid should be discontinued immediately.22
If the patient develops signs or symptoms suggestive of hepatitis, isoniazid should be stopped immediately, a blood sample should be sent for liver function tests (ALT test is adequate), and the patient should be referred immediately to a medical officer.22 On the other hand, worsening or developing acute illness, pneumonia, and gastrointestinal infections were also among the contributing reasons for nonadherence. Participants who developed an acute illness might have taken only drugs that treated the illness and ignored their preventive treatment with isoniazid.
Not being sure at which time to take isoniazid pills was also a reason for nonadherence (14%). Similarly, a study conducted in Thailand also revealed that the perceived side effects of isoniazid and misunderstanding about the duration of the preventive therapy were reasons for being nonadherent.25
With regard to occupation as a factor in nonadherence, self-employed participants such as merchants and servants showed higher nonadherence rates. This might be attributed to their jobs, since they might have been leaving their pills at home, and searching for jobs might have been a barrier to taking their INH pills.25 Being employed in government jobs may also have been a factor in nonadherence, due to carelessness in taking INH pills, fear of stigma at the workplace, and less confidentiality.
Limitations of the study
This study tried to assess the level of IPT adherence using a self-reported survey, which is subject to recall and social desirability biases. The other limitation was that no standard questionnaire was used to measure the level of adherence; instead, a cutoff point of adherence of 80% and above was used as a standard from previous studies that were conducted in South Africa and Addis Ababa. Moreover, data on CD4 level and HIV viral load test were not obtained.
Conclusion
The overall level of adherence to IPT is high. Patients who took INH for ≥5 months and did not experience any side effects were found to be more likely to be adherent than those who took it between 1 and 2 months and experienced side effects. Among the predictors reported for being nonadherent, carelessness and/or forgetfulness were the major ones. Health professionals and the Ministry of Health should design and deliver appropriate health education tips and messages on the aforementioned risk factors for patients to promote better adherence. Moreover, counseling should focus on patients who are in the first and second months of follow-up and advise them to develop habits such as using cell phones and watches with alarms and memory aids such as diaries as reminders are very important to improve their adherence.
Acknowledgments
We would like to acknowledge the staff of Gondar University Referral Hospital ART Pharmacy and selected health centers in the town for their cooperation during data collection.
Disclosure
Financial support was provided only by the authors. The authors report no other conflicts of interest in this work.
References
WHO. Global Tuberculosis Control. Geneva: World Health Organization; 2011. Available from: http://www.who.int/tb/publications/glob1port/2011/gtbr11_full.pdf | ||
Sharma SK, Mohan A, Kadhiravan T. HIV-TB co-infection: epidemiology, diagnosis & management. Indian J Med Res. 2005;121:550–567. | ||
Sterling TR, Pham PA, Chaisson RE. HIV Infection – related tuberculosis: clinical manifestations and treatment. Clin Infect Dis. 2010;50:S223–S230. | ||
Pawlowski A, Jansson M, Sköld M, Rottenberg ME, Källenius G. Tuberculosis and HIV Co-Infection. PLoS Pathog. 2012;8:e1002464. | ||
Getahun H, Gunneberg C, Granich R, Nunn P. HIV Infection associated tuberculosis: the epidemiology and the response. Clin Infect Dis. 2010;50:S201–S207. | ||
WHO. Global Tuberculosis Report. Geneva: World Health Oraganization; 2012:8–12. Available from: www.who.int/tb/publications/factsheet_global.pdf | ||
WHO. Policy on Collaborative TB/HIV Activities. Geneva: World Health Oraganization; 2012:15–18. Available from: http://whqlibdoc.who.int/publications/2012/9789241503006_eng.pdf | ||
World Health Organization. Guidelines for Intensified Tuberculosis Case-Finding and Isoniazid Preventive Therapy for People Living with HIV in Resource-Constrained Settings. Geneva: World Health Organization; 2011. | ||
Hart L. Isoniazid Preventive Therapy for the Prevention of Tuberculosis in PeopleLiving with HIV/AIDS. The FHI 360 Research Utilization unit; 2011. | ||
Berhe M, Demissie M, Tesfaye G. Isoniazid preventive therapy adherence and associated factors among HIV positive patients in Addis Ababa. Ethiopia Adv Epidemiol. 2014;2014:1–6. | ||
Mindachew M, Deribew A, Tessema F, Biadgilign S. Predictors of adherence to isoniazid preventive therapy among HIV positive adults in Addis, Ethiopia. BMC Public Health. 2011;11(1):916. | ||
Li J, Munsiff SS, Tarantino T, Dorsinville M. Adherence to treatment of latent tuberculosis infection in a clinical population in New York City. Int J Infect Dis. 2010;14(4):e292–e297. | ||
Munseri PJ, Talbot EA, Mtei L, Von Reyn CF. Completion of isoniazid preventive therapy among HIV-infected patients in Tanzania. Int J Tuberc Lung Dis. 2008;12(9):1037–1041. | ||
Hiransuthikul N, Nelson KE, Hiransuthikul P, Vorayingyong A, Paewplot R. INH preventive therapy among adult HIV-infected patients in Thailand. Int J Tuberc Lung Dis. 2005;9:270–275. | ||
Makanjuola T, Taddese HB, Booth A. Factors associated with adherence to treatment with isoniazid for the prevention of tuberculosis amongst people living with HIV/AIDS: a systematic review of qualitative data. PLoS One. 2014;9(2):e87166. | ||
Rutherford ME, Ruslami R, Maharani W, et al. Adherence to isoniazid preventive therapy in Indonesian children: a quantitative and qualitative investigation. BMC Res Notes. 2012;5:7. | ||
Golub JE, Paul P, Mohapi L, et al. Isoniazid preventive therapy, HAART and tuberculosis risk in HIV-infected adults in South Africa: a prospective cohort. AIDS. 2009;23(5):631–636. | ||
Mindachew M, Deribew A, Memiah P, Biadgilign S. Perceived barriers to the implementation of isoniazid preventive therapy for people living with HIV in resource constrained settings: a qualitative study. Pan Afr Med J. 2014;17:1–6. | ||
Gust DA, Mosimaneotsile B, Mathebula U. Risk factors for non-adherence and loss to follow-up in a three-year clinical trial in botswana. PloS One. 2011;6:5–7. | ||
Rowe KA, Makhubele B, Hargreaves JR, Porter JD, Hausler HP, Pronyk PM. Adherence to TB preventive therapy for HIV-positive patients in rural South Africa: implications for antiretroviral delivery in resource-poor settings? Int J Tuberc Lung Dis. 2005;9:263–269. | ||
Getu D, Tegbar Y. Lecture Notes for Health Sciences: Research Methodology. Gondar: University of Gondar; 2006:47–50. | ||
Guidelines For Tuberculosis Preventive Therapy Among HIV Infected Individuals (South Africa guidelines). Available from: http://www.who.int/hiv/pub/guidelines/south_africa_hiv_tb.pdf. Accessed April 3, 2017. | ||
Taddesse D. Assessment of IPT implementation, adherence and its determinants in the public health facilities of Diredawa. UOG/ACIPH. 2009:5–7. | ||
Sutton BS, Arias MS, Chheng P, Eang MT, Kimerling ME. The cost of intensified case finding and isoniazid preventive therapy for HIV-infected patients in Battambang, Cambodia. Int J Tuberc Lung Dis. 2009;13(6):713–718. | ||
Ngamvithayapong J, Uthaivoravit W, Yanai H, Akarasewi P, Sawanpanyalert P. Adherence to tuberculosis preventive therapy among HIV-infected persons in Chiang Rai, Thailand. AIDS. 1997l;11(1):107–111. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.