Back to Journals » Patient Preference and Adherence » Volume 12
Self-care agency in systemic lupus erythematosus and its associated factors: a cross-sectional study
Authors Yang H, Xie X, Song Y , Nie A, Chen H
Received 16 January 2018
Accepted for publication 10 March 2018
Published 23 April 2018 Volume 2018:12 Pages 607—613
DOI https://doi.org/10.2147/PPA.S162648
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Hui Yang, Xia Xie, Yuqing Song, Anliu Nie, Hong Chen
West China School of Nursing and Department of Nursing, West China Hospital, Sichuan University, Chengdu, China
Purpose: The aim of this study was to estimate the level of self-care agency and explore its associated factors in patients with systemic lupus erythematosus (SLE).
Patients and methods: In this cross-sectional study, all patients were from a tertiary general hospital between July and October 2016 in Southwest China. The self-care agency was assessed using the Exercise of Self-care Agency Scale. Other variables were measured by the Visual Analog Scale, Systemic Lupus Erythematosus Disease Activity Index 2000, the physical component summary, and mental component summary of the 36-item Short Form Health Survey. Multivariate regression analysis was performed to explore the associated factors of self-care agency.
Results: A total of 123 patients were recruited. The mean score of Exercise of Self-care Agency Scale was 86.29. In univariate analysis, self-care agency of patients differed in regard to gender, work status, educational level, household income monthly per capita, and disease activity (P<0.05). Additionally, higher body mass index, higher level of fatigue, and worse mental health were found in patients with lower self-care agency (P<0.05). The stepwise multivariate regression analysis showed that male gender (P=0.001), lower educational level (P=0.003), lower household income monthly per capita (P<0.001), and worse mental health (P<0.001) could predict lower self-care agency.
Conclusion: Patients with SLE had a middle level of self-care agency, suggesting that there is still much scope for improvement. The lower level of self-care agency was associated with male gender, lower educational level, lower household income monthly per capita, and worse mental health. Therefore, health care providers should develop targeted and comprehensive interventions to enhance self-care agency in patients with SLE.
Keywords: systemic lupus erythematosus, self-care agency, patients, mental health
Plain language summary
Systemic lupus erythematosus (SLE) is a common multisystem autoimmune rheumatic disease in China. According to previous studies, patients with a high level of self-care agency might achieve better health outcomes. Therefore, it is very important to cultivate better self-care agency in patients with SLE. However, few studies have been conducted to estimate the level of self-care agency and explore its associated factors in China. Therefore, this study was performed to investigate the level of self-care agency and explore its associated factors in patients with SLE in China. Their study included 123 patients from a tertiary general hospital between July and October 2016 in Southwest China. The result demonstrated that the patients with SLE had a middle level of self-care agency. In addition, male gender, lower educational level, lower household income monthly per capita, and worse mental health were associated with lower self-care agency. The results suggest that health care professionals should pay more attention to men and patients with lower educational level, lower household income monthly per capita, and worse mental health. Meanwhile, targeted and comprehensive interventions should also be developed to enhance their self-care agency.
Introduction
Systemic lupus erythematosus (SLE) is a chronic, inflammatory, potentially fatal, and multisystem autoimmune rheumatic disease with variable clinical manifestations and a complex course.1 It can occur at any age and is more common in women than in men. There are marked differences in SLE prevalence worldwide. In USA, the prevalence of SLE ranged from 5.8 to 130 per 100,000 population, whereas the prevalence in UK and Japan was approximately 40.7 and 19.1 per 100,000 population.2–4 In China, the prevalence of SLE ranged from 31 to 70 per 100,000 population.5 Although China does not have the highest prevalence of the disease, patients with SLE here would be form the largest cluster in the world due to the large population base.
Numerous studies have demonstrated the great improvements in the treatment of SLE, but the disease cannot be cured currently.6,7 Moreover, SLE has a negative effect on numerous aspects of a patient’s life, such as mental health, quality of life, and daily functioning,8–10 which may lead to low employment rates and heavy economic burden.6,11 According to previous studies, patients with high level of self-care agency might achieve better health outcomes.12 Therefore, it is very important to cultivate better self-care agency in patients with SLE. Self-care agency was first developed by Orem and defined as the acquired capability to meet one’s constant self-care requisites that could provide regular life processes, maintain and improve health, and promote well-being, without depending on others.13 It was also regarded as the determinant factor of self-care performance.14 Self-care agency, an important component of Self-Care Deficit Nursing theory, primarily concentrated on heightening self-care behavior, decreasing health-related cost, and improving self-care quality and patient outcome.15
At present, the self-care agency had been paid more attention in patients with chronic disease, mainly focusing on diabetes,16 hypertension,17 coronary heart disease,18 and rheumatoid arthritis (RA).19 However, few studies have been conducted to estimate the level of self-care agency in patients with SLE. Additionally, Orem’s Self-Care Model reveals that internal and external factors have an effect on self-care agency, including sociodemographic, psychological, and clinical characteristics.20 Therefore, the purpose of this study was to estimate the level of self-care agency and explore its associated factors in patients with SLE in China.
Patients and methods
Study design and population
Design
This cross-sectional study was conducted in a tertiary general hospital in Southwest China. Our study aimed to estimate the level of self-care agency and explore its association with sociodemographic and disease-related characteristics in patients with SLE.
Patients
All participants were enrolled by convenience sampling. Patients who met the following inclusion criteria were included: patients fulfilling the SLE diagnosis according to the 1997 American College of Rheumatology modified criteria for the classification,21 age 18 years or over, having the ability to read and write, being willing to participate in this study, and capable of completing the questionnaires independently. Patients were excluded if they could not communicate with researchers because of severe mental disturbance, occurrence of other comorbidities which might hinder their independence in health care management, like malignancy or stroke, and were pregnant at time of the visit.
Assessment methods
Self-care agency
Self-care agency was assessed using the Exercise of Self-care Agency (ESCA) Scale. This self-administered instrument consists of four subscales, including active versus passive response to situations, motivations, the knowledge base, and the sense of self-worth. It has 43 items on a 5-point Likert-type scale ranging from 0 (it does not describe me) to 5 (it completely describes me). The total score ranges from 0 to 172, which is equally divided into three levels: low (<56.76), moderate (56.76–113.52), and high (>113.52). Higher scores indicate higher level of self-care agency. In the Chinese version, the Cronbach’s α of ESCA was 0.88 and its content validity was 0.92, indicating a good reliability and validity.22,23
Pain and fatigue
The visual analog scale was used to estimate the severity of pain and fatigue. It records from 0 cm (none) to 10 cm (very severe) each item. Higher scores represent worse pain or fatigue.
Disease activity
Disease activity was measured by using Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K). SLEDAI-2K is based on the presence of 24 descriptors in nine organ systems over the previous 10 days. The final score ranges from 0 to 105. According to a previous study, this scale is divided into four levels: 0–4 (no activity); 5–9 (mild activity); 10–14 (moderate activity); and 15–105 (high activity).24
Physical and mental health
Physical and mental health were estimated by the physical component summary (PCS) and mental component summary (MCS) of the 36-item Short Form Health Survey. The PCS is comprised of four domains, including physical functioning, role-physical, bodily pain, and global health, while the other four domains, namely vitality, social functioning, role-emotional, and mental health, comprised the MCS. The total score of PCS or MCS is calculated by the summing four domains respectively. Higher scores indicate better physical or mental health.25 This scale had a good reliability with and validity in Chinese version.26
Statistics analysis
The sociodemographic and disease-related variables were assessed as mean ± standard deviation, median (interquartile range), frequencies, and percentage, according to the data types and distribution. In univariate analysis, independent samples t-test, one-way analysis of variance, Mann–Whitney U test, and Spearman’s rank-correlation test were used to analyze the relationship between demographic, disease-related variables, and self-care agency in SLE patients. Multivariate analysis was conducted using the stepwise multivariate regression analysis to explore the factors associated with self-care agency. A two-tailed P-value<0.05 was considered statistically significant. Analyses were performed using the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA) software version 21.0.
Ethics approval and informed consent
All procedures performed in studies involving human participants were performed in accordance with the ethical standards of the institutional research committee and following the tenets of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All patients provided written informed consent to participate and publish their details. This study had been approved by West China Hospital of Sichuan University Biomedical Research Ethics Committee (20160041).
Results
Patient characteristics
We distributed out 128 questionnaires, and all were returned. Five questionnaires were excluded from this study due to up to 10% missed items. Finally, a total of 123 patients were included in our study.
The sociodemographic and disease-related characteristics of the patients are shown in Tables 1 and 2. The median age was 36, and 87.5% of the patients were women. Patients who were unemployed constituted 77.2% of the study group. Twenty-six percent of these patients had been educated to the college level or higher, and 27.6% were single. The majority of patients had other disease (83.7%) and one or more children (69.9%). Only 6.5% of patients had SLEDAI-2K≦4, and household income monthly per capita (HIMPC) of 16.3% patients was less than $150. In addition, the mean score of ESCA was 86.29±8.52. The median score of body mass index, pain, and fatigue was 21.23, 2.00, and 4.00, respectively. The median duration of disease was 36.00 months. Also, the median score of PCS and MCS was 50.50 and 44.95, respectively.
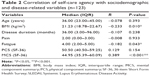
Factors associated with self-care agency
In univariate analysis, the results showed that self-care agency of discharged patients differed in regard to gender (P=0.011), work status (P=0.017), educational level (P<0.001), HIMPC (P<0.001), and disease activity (P=0.022) (Table 1). Spearman’s rank-correlation test showed that higher body mass index (r=−0.233, P=0.010), higher level of fatigue (r=−0.182, P=0.043), and worse mental health (r=0.389, P<0.001) were related with lower self-care agency (Table 2).
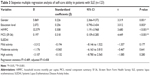
Table 3 shows the stepwise multivariate regression analysis for self-care ability. The multiple categorical variable was converted to a dummy variable. Our results showed that male gender (B=0.226, P=0.001), lower educational level (B=0.256, P=0.003), lower HIMPC (B=0.308, P<0.001), and worse mental health (B=0.318, P<0.001) could predict lower self-care agency. These variables could explain the 45.8% of variance in ESCA. However, there was no significant association between self-care agency and the other variables, including disease duration, pain, fatigue, physical health, disease activity, and other sociodemographic variables.
Discussion
In our study, the mean score of ESCA was 86.29±8.52, which demonstrated that our patients had a moderate level of self-care agency. The level of self-care agency in patients with SLE was consistent with that in patients with coronary heart disease and hypertension, whereas it was found to be higher than that in patients with RA.17–19 This may be explained by several possible reasons. The first one may be that 26.0% of patients with SLE had a college-level education or higher in our study, while Ovayolu et al19 revealed that only 5.1% of patients with RA had a college-level education or higher. Previous studies showed that patients with higher educational level have better self-care agency.16,17 Additionally, in recent years, the hospital where our study conducted has implemented a health care program of rheumatology diseases, including health education clinic and chronic disease management clinic, which could gradually improve self-care agency.27
Our analysis found that the level of self-care agency in women was higher than that in men. One of the reasons for the diverse results may be that women are more willing to seek health care than men, so women could gain more information and methods about how to manage disease better from health care providers.28 On the other hand, women are commonly regarded as caregivers of the whole family in Chinese traditional culture.29 They could thus also acquire knowledge and skills during caring for family members. Previous research revealed that the process of learning or teaching and guidance from others enable the development and promotion of self-care agency.30 As a result, self-care agency of women was higher than that of men.
As in previous studies,17–19 we also found that higher educational level was associated with higher level of self-care agency. A higher level of educational could increase the cognitive abilities and the decision-making capability, which makes individuals choose protective health behavior well, and in turn improves their self-care agency.31 In addition, in the human capital theory, education not only makes people more effective users of information but also encourages people to obtain information with the intent to use it.32 Marazienė et al33 also demonstrated that patients with higher education levels seek health-related information more frequently than those with primary or secondary education. Thus, patients with a high level of education might gain more health-related information, and in turn improved their self-care agency. Besides, higher educational attainment is propitious to increase the self-care agency that motivates patients to design a healthy lifestyle.34 Therefore, the health care professionals should help patients, especially those with a low level of education, receive more health-related information and offer various paths of access to information, thus helping patients enhance their self-care agency and take care of themselves better.
Our results found that lower HIMPC was positively associated with lower level of self-care agency. This can be due to the fact that patients with lower HIMPC reported insufficient social support, which was thus related with the lower level of self-care agency.35,36 Additionally, patients with lower HIMPC hardly maintain regular medical appointments, and thus this might preclude them from attaining sufficient information and developing their self-care agency.37 It suggests that health care professionals should provide more health-related assistance and that government also should improve social welfare for patients with lower HIMPC.
In addition, we observed that worse mental health was a positive contributing factor to a lower level of self-care agency. A prior study stated that worse mental health negatively affects executive function, a brain-control function.38 This executive function, used to guide the cognitive activities, includes diverse cognitive abilities, such as working memory, mindfulness and self-control, and other higher-order activities.39 They are propitious for individuals to possess regular the optimal emotional response, which might improve their self-care agency.40–42 Besides, a study by Yildirim et al43 reported that anxiety and depression have a negative effect on self-care agency. Thus, we should provide psychological counseling and efficient mental treatment for patients with mental health problems in order to promote mental health and enhance self-care agency.
In the present study, there was no statistical significance between pain and self-care agency, which was not in line with the finding from another study.19 A possible explanation for this could be that participants in our study had only slight pain which might not affect their self-care agency. In addition, self-care agency was found to not be associated with disease duration, disease activity, fatigue, and physical health. Further studies are needed to explore the association between pain, disease duration, disease activity, fatigue, and physical health.
Limitations
Our study had several limitations. First, all patients were included by the convenience sampling technique from a hospital, leading to the lack of generalizability. In addition, the cross-sectional study nature precludes us from indicating the causal link between self-care agency and other variables. Future longitudinal research studies with large sample size should be performed to appraise the fluctuation in self-care agency and its associated factors.
Conclusion
The results of this study indicated that patients with SLE had a middle level of self-care agency, suggesting that there is still much scope for improvement. The lower level of self-care agency was seen with men and those with lower educational level, lower HIMPC, and worse mental health. These findings suggest that health care providers should develop the targeted and comprehensive interventions to enhance self-care agency in patients with SLE, especially for the males and those with lower educational level, lower HIMPC, and worse mental health.
Acknowledgment
We specially thank all the patients who participated in the study and also the investigators for their valuable help in patient recruitment and data collection.
Disclosure
The authors report no conflicts of interest in this work.
References
Rahman A, Isenberg DA. Systemic lupus erythematosus. N Engl J Med. 2008;358(9):929–939. | ||
Petri M. Epidemiology of systemic lupus erythematosus. Best Pract Res Clin Rheumatol. 2002;16(5):847–858. | ||
Nightingale AL, Farmer RD, de Vries CS. Systemic lupus erythematosus prevalence in the UK: methodological issues when using the General Practice Research Database to estimate frequency of chronic relapsing-remitting disease. Pharmacoepidemiol Drug Saf. 2007;16(2):144–151. | ||
Osiosalido E, Manapatreyes H. Epidemiology of systemic lupus erythematosus in Asia. Rheumatology. 2010;19(12):1365–1373. | ||
Zeng QY, Chen R, Darmawan J, et al. Rheumatic diseases in China. Arthritis Res Ther. 2008;10(1):R17. | ||
Kan HJ, Song X, Johnson BH, Bechtel B, O’Sullivan D, Molta CT. Healthcare utilization and costs of systemic lupus erythematosus in medicaid. Biomed Res Int. 2013;2013:808391. | ||
Jiao B, Gao J. Intensive research on the prospective use of complementary and alternative medicine to treat systemic lupus erythematosus. Drug Discov Ther. 2013;7(4):167–171. | ||
Baker K, Pope J. Employment and work disability in systemic lupus erythematosus: a systematic review. Rheumatology. 2009;48(3):281–284. | ||
García-Carrasco M, Mendoza-Pinto C, Cardiel MH, et al. Health related quality of life in Mexican women with systemic lupus erythematosus: a descriptive study using SF-36 and LupusQoL(C). Lupus. 2012;21(11):1219–1224. | ||
Zhang L, Fu T, Yin R, Zhang Q, Shenl B. Prevalence of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. BMC Psychiatry. 2017;17:70. | ||
Yelin E, Trupin L, Katz P, et al. Work dynamics among persons with systemic lupus erythematosus. Arth Rheum. 2007;57(1):56–63. | ||
Hu L, Lingler JH, Devito DA, Dew MA, Sereika SM. Trajectories of self-care agency and associated factors in lung transplant recipients over the first 12-months following transplantation. Clin Transplant. 2017;31(9). | ||
Sousa VD. Conceptual analysis of self-care agency. Online Braz J Nur [serial on the Internet]. 2002;1(3). Available from: http://www.nepae.uff.br//siteantigo/objn103sousa.htm. Accessed August 15, 2008. | ||
Çiftçi B, Yildirim N, Şahin Altun Ö, Avşar G. What level of self-care agency in mental illness? The factors affecting self-care agency and self-care agency in patients with mental illness. Arch Psychiatr Nurs. 2015;29(6):372–376. | ||
Moore JB, Pichler VH. Measurement of Orem’s basic conditioning factors: a review of published research. Nurs Sci Q. 2000;13:137–142. | ||
Vosoghi Karkazloo N, Abootalebi Daryasari Gh, Farahani B, Mohammadnezhad E, Sajjadi A. The study of self-care agency in patients with diabetes. Mod Care J. 2012;8(2):197–204. | ||
Akyol AD, Çetinkaya Y, Bakan G, Yarali S, Akkuş S. Self-care agency and factors related to this agency among patients with hypertension. J Clin Nurs. 2007;16(4):679–687. | ||
Lukkarinen H, Hentinen M. Self-care agency and factors related to this agency among patients with coronary heart disease. Int J Nurs Stud. 1997;34(4):295–304. | ||
Ovayolu OU, Ovayolu N, Karadag G. The relationship between self-care agency, disability levels and factors regarding these situations among patients with rheumatoid arthritis. J Clin Nurs. 2012;21(1–2):101–110. | ||
Orem DE. Nursing: Concepts of Practice. 6th ed. St Louis: Mosby; 2001. | ||
Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 2010;40(9):1725. | ||
Wang HH, Laffrey SC. Preliminary development and testing of instruments to measure self-care agency and social support of women in Taiwan. Kaohsiungy Med Sci. 2000;16(9):459–467. | ||
Wang YB, Xu LY, Yang LS, Yang LM, Yang HY. [Reliability and validity of Chinese version of the exercise of self-care agency scale in schizophrenia Patients]. J Clin Psychiatry. 2014;2:104–107. Chinese. | ||
Giadman DD, lbanez D, Urowitz MB. Systemic lupus erythematosusc disease activity index 2000. J Rheumatol. 2002;29(2):288–291. | ||
Ware JE, Kosinski M, Bjorner JB, Turner-Bowker DM, Gandek B, Maruish ME. User’s manual for the SF-36v2 Health Survey. 2nd ed. Lincoln, RI: QualityMetric Incorporated; 2007. | ||
Dong AS, Cai YL, Zeng JN, et al. [Reliability and validity of SF-36 (v. 2) scale in hospitalized patients with chronic heart failure]. Chinese Modern Nurs J. 2016;22(6):746–751. Chinese. | ||
Yang H, Zhao Y, Liu Y. [Are you ready to carry out the chronic management of rheumatology diseases?]. Chinese Med Association. 2017:633–634. Chinese. | ||
Thompson AE, Anisimowicz Y, Miedema B, Hogg W, Wodchis WP, Aubrey-Bassler K. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract. 2016;17(1):1–7. | ||
Tung HH, Hunter A, Wei J, Chang CY. Gender differences in coping and anxiety in patients after coronary artery bypass graft surgery in Taiwan. Heart Lung. 2009;38(6):469–479. | ||
Wright K. Knowledge, Exercise of Self-care Agency, and Recidivism Levels after Completing a Pulmonary Education Program [dissertation]. Arizona: University of Arizona; 1990. | ||
Baker DP, Leon J, Greenaway EGS, Collins J, Movit M. The education effect on population health: a reassessment. Popul Dev Rev. 2011;37(2):307–332. | ||
Becker G. Investment in human capital: a theoretical analysis. J Political Econ. 1962;70(9):9–49. | ||
Marazienė D, Klumbienė J, Tomkevičiūtė J, Misevičienė I. Sources and reasons for seeking health information by Lithuanian adults. Medicina (Kaunas). 2012;48(7):371–378. | ||
Mirowsky J, Ross CE. Education, personal control, lifestyle and health a human capital hypothesis. Res Aging. 1998;20(4):415–449. | ||
Alarcón GS, McGwin G Jr, Sanchez ML, et al. Systemic lupus erythematosus in three ethnic groups. XIV. Poverty, wealth, and their influence on disease activity. Arthritis Rheum. 2004;51(1):73–77. | ||
Mollaoglu M. Perceived social support, anxiety, and self-care among patients receiving hemodialysis. Dial Transplant. 2010;35(3):144–155. | ||
Rca T, Borba Neto EF, Christopoulos GB, Sato EI. The influence of income and formal education on damage in Brazilian patients with systemic lupus erythematosus. J Clin Rheumatol. 2017;23(5):246–251. | ||
Baune BT, Fuhr M, Air T, Hering C. Neuropsychological functioning in adolescents and young adults with major depressive disorder – a review. Psychiatry Res. 2014;218(3):261–271. | ||
Suchy Y. Executive functioning: overview, assessment, and research issues for non-neuropsychologists. Ann Behav Med. 2009;37(2):106–116. | ||
Tangney JP, Baumeister RF, Boone AL. High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. J Pers. 2010;72(2):271–324. | ||
Hanley A, Warner A, Garland EL. Associations between mindfulness, psychological well-being, and subjective well-being with respect to contemplative practice. J Happiness Stud. 2015;16(6):1423–1436. | ||
Schmeichel BJ, Volokhov RN, Demaree HA. Working memory capacity and the self-regulation of emotional expression and experience. J Pers Soc Psychol. 2008;95(6):1526–1540. | ||
Yildirim A, Aşilar RH, Bakar N, Demir N. Effect of anxiety and depression on self-care agency and quality of life in hospitalized patients with chronic obstructive pulmonary disease: a questionnaire survey. Int J Nurs Pract. 2013;19(1):14–22. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.