Back to Journals » Clinical Interventions in Aging » Volume 9
Selection of acupoints for managing upper-extremity spasticity in chronic stroke patients
Authors Wang B, Lin C , Li T, Lin S, Lin J, Chou L
Received 31 August 2013
Accepted for publication 2 October 2013
Published 10 January 2014 Volume 2014:9 Pages 147—156
DOI https://doi.org/10.2147/CIA.S53814
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Bi-Huei Wang,1,* Chien-Lin Lin,1,2,* Te-Mao Li,2,3 Shih-Din Lin,3 Jaung-Geng Lin,2 Li-Wei Chou1,2,4
1Department of Physical Medicine and Rehabilitation, China Medical University Hospital; 2School of Chinese Medicine, College of Chinese Medicine; 3Graduate Institute of Acupuncture Science, 4Acupuncture Research Center, China Medical University, Taichung, Taiwan
*These authors contributed equally to this work
Background: This study investigated the clinical efficacy of electroacupuncture (EA) in inhibiting upper-extremity spasticity in chronic stroke patients, and also in mapping a unique preliminary acupoint-selection protocol.
Methods: Fifteen patients were divided into two groups: patients in the control group (n=6) received minimal acupuncture (MA), and those in the experimental group (n=9) received EA. Four acupoints, which include Neiguan (PC6), Shaohai (HT3), Zeqian (Ex-UE, A32), and Shounizhu (EX-UE), were treated near the motor points of the muscles for elbow flexion, forearm pronation, and finger flexion. Both groups were treated for twelve sessions, 20 minutes per session, for 6 weeks (two sessions per week). The outcome measures in this study included angle of muscle reaction (R1), passive range of motion (R2), and dynamic component (R2–R1).
Results: In the experimental group, the R2–R1 of the elbow joint was significantly decreased at 1 (P=0.0079), 3 (P=0.0013), and 6 weeks (P=0.0149) after treatment compared with pretreatment levels (P<0.05). The between-group difference in the R2–R1 of the elbow joint after the 6-week treatment was statistically significant.
Conclusion: Combining the 6-week EA and standard rehabilitation treatment reduced the spasticity of the elbow for chronic stroke survivors. However, no significant effect was observed in the spasticity of the wrist joints. The choice of acupoints and the frequency of EA have to be taken into account to achieve a positive treatment effect. The correlation between acupoints and motor points provides a model of acupoint selection to improve spasticity.
Keywords: acupoints, acupuncture, electroacupuncture, motor point, spasticity, stroke
Introduction
Stroke was the second-leading cause of death in the Taiwanese population between 1985 and 2006 and the third-leading cause of death in the Taiwanese population in 2010, based on statistical data from the Chinese Department of Health.1 Approximately 18.9% of stroke survivors in Taiwan have moderate levels of disability, and 26.4% have the most severe motor disability.2 Stroke survivors are seriously affected by such complications as handicaps, unclear consciousness, aphasia, dementia, psychological abnormalities,2 and incomplete bladder emptying.3 Most of these patients have permanent disabilities, and tend to show dependence in performing daily activities to various degrees. Stroke sequelae are a serious burden for the family of stroke survivors and for the whole society.
Spasticity is a component of upper-motor neuron syndromes such as stroke, and has been defined as a motor disorder characterized by a velocity-dependent increase in tonic stretch reflexes with exaggerated tendon jerks, which result from the hyperexcitability of the stretch reflex.4 Severe spasticity can cause reduced flexibility, posture, and functional mobility, as well as joint pain, contracture, and difficulty in positioning for comfort and hygiene.5 Pinedo and de la Villa6 also declared that 23% of stroke patients experienced joint tightness and soreness because of contracture. It is also considered as a potential obstacle in improving motor control and functional ability of the upper limb when patients undergo different rehabilitative techniques.
Various methods for managing spasticity can be used, depending on clinical need and probability of success, to achieve specific functional goals. Treatment may include antispastic medications, such as baclofen, diazepam, tizanidine, or dantrolene. Physical therapy regimens may include muscle stretching and range-of-motion exercises to help prevent muscle shortening and atrophy and to reduce the severity of symptoms. Physical modalities and electrical stimulation can also help in managing spasticity. Targeted injection of phenol and botulinum toxin may be used to relax specific muscles. Surgical techniques, including orthopedic procedures, intrathecal baclofen, and selective dorsal rhizotomy, may be recommended for tendon release or to sever the nerve–muscle pathway.5 However, these treatments have their own disadvantages or limitations. For instance, oral medications have systemic side effects, such as sedation and metabolic load.7 Botulinum toxin injection is relatively expensive and requires repetition.8 Intrathecal baclofen has been associated with pruritus, dramatic increase in spasticity, agitation, seizures, and mortality resulting from withdrawal.5
Acupuncture is one of the main modes of treatment in traditional Chinese medicine (TCM), and has been performed for more than 2,000 years. It was widely used to treat hemiplegia long before the Tang dynasty.9 TCM is based on the yin–yang theory, where energy called chi flows through the organs. Chi is essential in maintaining good health.10,11 Acupuncture can correct the imbalance of energy circulation.11 Studies have shown that acupuncture could improve poststroke motor ability.9,12,13 Systematic reviews14–16 that include a consensus statement from the National Institutes of Health in 199717 suggest that acupuncture might be a useful supplement to stroke rehabilitation. Electroacupuncture (EA) is performed in the therapy, where a trace electric current similar to the human bioelectric current is applied to the needle until a needling sensation is felt by the patient. The needle is placed on the meridian points of the human body.18 This method is often used to treat Wei flaccid syndrome and various injuries of the muscles, joints, ligaments, and tendons.18 A study has shown that EA can temporarily reduce spasticity caused by stroke, and if applied repeatedly, it can maintain a reduced level of spasticity.19 Another study has shown that acupuncture might improve the function of the affected upper limb in patients with chronic hemiparetic stroke by increasing the activity in the ipsilesional motor cortex.20 However, this study did not mention the selection of acupoints, and the sample size was small.
We conducted a pilot study to investigate the clinical efficacy of EA in inhibiting the upper-extremity spasticity of chronic stroke patients, and to map a unique preliminary acupoint-selection protocol based on TCM. We also tried to determine the correlation between acupoints and motor points.
Materials and methods
Patients
A prospective study was conducted between August 2008 and July 2009 at clinical sites in mid-Taiwan Chinese medical university medical centers. Patients diagnosed with first instance of stroke were recruited for this study. During the study enrollment period, the patients continued conventional therapy (medication including hypoglycemic agents, insulin, and hypertensive agents, as well as regular rehabilitation programs). No major changes in drug administration and rehabilitation were done during the study.
Inclusion and exclusion criteria
The inclusion criteria included the following: 1) first instance of stroke (confirmed by computerized tomography scan or magnetic resonance imaging based on the definition of the World Health Organization); 2) aged between 35 and 65 years; 3) stroke duration of over 6 months before enrollment; 4) had the ability of oral communication; 5) modified Ashworth scale of spasticity greater than or equal to 2; and 6) Brunnstrom stage II or III in the affected upper limb.
The exclusion criteria included the following: 1) recurrent stroke; 2) any condition of unstable neurologic or psychological symptom; 3) poorly controlled diabetic mellitus and hypertension; 4) infection or dermatologic condition at acupuncture sites; 5) inflammation, old fracture, or prosthesis in the study limb; 6) arrhythmia or implanted pacemaker; 7) past or planned treatment for spasticity in the study limb with phenol or alcohol block, intrathecal baclofen pumping, or surgery. In addition, patients were excluded if they had been treated with botulinum toxin injection within the last 6 months. All patients gave informed consent, and the institutional review board of the university approved the study.
Identification of the acupuncture points
Four acupuncture points – Neiguan (PC6), Shaohai (HT3), Shounizhu (EX-UE), and Zeqian (EX-UE, A32) (Table 1) – were selected for treatment and were identified by an experienced traditional Chinese physician in this study.21–23
Treatment procedures
After giving informed consent, the patients were given random numbers that were produced by a computer. The patients were grouped into two groups: experimental group, where the patients received EA with standard rehabilitation (SR); and control group, where the patients received minimal acupuncture (MA) with SR. SR included passive range-of-motion exercises, stretching exercises, strengthening exercises, balance training, mobility training, and functional training. The experimental group was treated with acupuncture for twelve sessions, 20 minutes per session, for over 6 weeks (two sessions per week). The needles were inserted in the following acupoints on the subject’s hemiparetic arm: Zeqian (EX-UE, A32), Shounizhu (EX-UE), Shaohai (HT3), and Neiguan (PC6). The frequency of electrical stimulation was 50 Hz. The intensity of the current was increased to the point where the patient reported a needling reaction. At this point, the current was slightly reduced to an unpleasant but tolerable intensity. The needling reaction is the characteristic response of a subject to acupuncture-needle insertion and manipulation. Electrical stimulation lasted for 20 minutes.
The control group received SR and MA. Stimulation was applied using the same electrodes, locations, and device with the electrical stimulator disconnected. Minimal acupuncture was used. Needle insertion was limited to depths of 0.05– 0.2 cun, and no needle manipulation was performed after needle insertion. Eliciting “de-chi” was prohibited. Electric stimulation lasted for 20 minutes.
Measurement of outcomes
The efficacy of treatment was measured before, immediately, 3 weeks, and 6 weeks after the start of the treatment. We measured the patient’s angle of muscle reaction (R1), passive range of motion (R2), dynamic component (R2–R1) in the wrist and elbow joints by using a goniometer. The R1 angle is the “angle of catch” after a quick stretch, whereas the R2 angle is the passive joint range of movement following a slow stretch. The R2–R1 value indicates the level of dynamic component of spasticity in the muscle, and is proportional to the severity of spasticity.24 Furthermore, to ensure consistency, the evaluating therapist who scored the outcome was the same person on each occasion for each patient, and was blinded to the type of treatment.
Statistical analysis
All statistical analyses were performed using SPSS version 10.0 for Windows (IBM, Armonk, NY, USA). The means and standard deviations were calculated for all subjects in each group for each parameter. Changes from these two groups were evaluated using a paired-sample t-test. A P-value of <0.05 was considered statistically significant.
Results
Demographics
A total of 20 patients were enrolled and randomly distributed to the experimental group or control group; 15 (75%) completed the whole study course (Figure 1). No complication was observed during the EA treatment. The experimental group consisted of three male participants and six female participants. The mean age was 61.67±6.91 years, and the average duration after stroke onset was 4.67±2 years. The ratio of ischemic stroke to hemorrhagic stroke was 5:4. The control group consisted of one male participant and five female participants. The mean age was 55.17±12.92 years, and the average duration after stroke onset was 5.33±1.03 years. The ratio of ischemic stroke to hemorrhagic stroke was 2:4. The demographic characteristics are shown in Table 2. No significant difference was observed in any demographic variable in either group (P>0.05).
  | Figure 1 Flow diagram showing the paths for recruited patients. |
  | Table 2 Demographic characteristics of the subjects in both groups |
Difference in R2–R1 obtained before and after treatment
In the experimental group, the R2–R1 value of the elbow joint was significantly decreased 1, 3, and 6 weeks after treatment compared with pretreatment levels (P<0.05) (Table 3 and Figure 2). In the experimental group, no significant changes were observed for any R2–R1 value of the wrist joint measured during the treatment period. In the control group, no significant changes were observed for any R2–R1 value of the elbow and wrist joints measured during the treatment period.
  | Table 3 Changes in R2–R1 of elbow and wrist joints in the two groups |
  | Figure 2 Intragroup and between-group change of R2–R1 of elbow joint and wrist joint. *P<0.05. |
Between-group differences in R2–R1
No significant difference was observed in the R2–R1 values of the elbow joint between the experimental and control groups at 3 weeks after treatment. After 6 weeks, the average R2–R1 value of the elbow joint was 31.75°±17.38° in the experimental group, which was significantly less than that of the control group, at 66°±11.87° (P=0.0014) (Table 4 and Figure 2). No significant difference was observed in the R2–R1 values of the wrist joint between the experimental and control groups at 3 and 6 weeks after treatment.
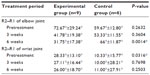  | Table 4 Comparison of R2–R1 between experimental and control groups |
Discussion
Summary of the important findings in this study
Patients diagnosed with first instance of stroke received either twelve sessions, two sessions per week, 20 minutes per session, EA of 50 Hz with SR in the experimental group or MA with SR in the control group. This study demonstrates that a significant reduction was observed in the R2–R1 values of the elbow joint 1, 3, and 6 weeks after treatment compared with pretreatment levels in the experimental group. However, no significant treatment effect was observed in the wrist joint. In the control group, no significant changes were observed for any R2–R1 value of the elbow and wrist joints measured during the treatment period.
Effectiveness of the EA treatment for spasticity in stroke patients
The spasticity and R2–R1 value of the elbow joints were significantly reduced after 6 weeks of SR and additional EA twice per week in nine patients in the experimental group. A randomized controlled study has also shown that EA has additional beneficial effects on the long-term recovery of motor function in patients after the first instance of ischemic stroke, especially in upper-limb motor function, compared with conventional rehabilitation.25 Furthermore, the reduction of the R2–R1 value of the elbow in the experimental group 6 weeks after treatment (−40.75°±35.92°) was greater than that 3 weeks after treatment (−30.89°±19.16°). The treatment effect in poststroke spasticity could be maintained by repeated EA. This observation supports those of other studies, where EA was reported to reduce temporarily the spasticity caused by stroke and that a reduced level of spasticity could be maintained when EA was repeatedly applied.19
On the contrary, the R2–R1 value of the wrist joint in the experimental group 3 weeks after treatment (27.11°±16.44°) was less than that before treatment (28.33°±13.10°). The R2–R1 value of the wrist joint 6 weeks after treatment (26.00°±18.70°) was less than that 3 weeks after treatment. No significant treatment effect was observed in the wrist joint. Furthermore, we assumed that this phenomenon was related to the principle of selection of acupoints.
Correlation between acupoints, myofascial trigger points, and end plate
The motor point is the point over a muscle where a contraction of a muscle may be elicited by a minimal-intensity, short-duration electric stimulus. The motor point corresponds anatomically to the location of the terminal portion of the motor nerve fibers (end-plate zone). The end-plate zone is the region in a muscle where the neuromuscular junctions of the skeletal muscle fibers are concentrated.26
The myofascial trigger point (MTrP) is defined by Travell and Simons27,28 as the most tender (hyperirritable) spot in a palpable taut band of skeletal muscle fibers. It has been suggested that “spot tenderness,” “taut band,” and “pain recognition” are the three important criteria for the diagnosis of MTrP, and “referred pain” and “local twitch responses” (brisk contraction of muscle fibers in its taut band) can be “confirmatory signs” for MTrP diagnosis.29 It has been suggested that MTrPs appear to be related to excessive acetylcholine release in the neuromuscular junction (motor end plate), and MTrPs appear to be located in the end-plate zone of the affected muscle fibers, where there was increased spontaneous electrical activity.30–32
Melzack et al33 found the trigger points are firmly anchored in the anatomy of the neural and muscular systems. He suggested a hypothesis that trigger points and acupoints for pain, though discovered independently and labeled differently, present the same phenomenon, and found a remarkably high degree (71%) of correspondence with MTrPs and acupoints. Dorsher found strong anatomic (92%), clinical (79.5%), and meridian-referred pain (76%) correspondences of trigger and acupoints in his study, and suggested acupuncture meridians were shown not only to exist conceptually but also to be physiologic (and possibly anatomic) entities.34,35
Selection of acupoints
We chose acupoints based on the traditional Chinese medicine theory of yin and yang, as well as that of meridians and collaterals. Significant improvement in the spasticity of the elbow joint was observed.
Botulinum toxin is the most promising blocking agent used for focal treatment of spasticity. When injected intramuscularly, botulinum toxin works at the end-plate level by blocking the release of acetylcholine into the synaptic cleft.36 A study has shown that intramuscular injections of botulinum toxin A in upper-limb muscle groups reduced the spasticity and associated disabilities in patients who had had a stroke.8 Since Botulinum toxin injection for upper-extremity spasticity treatment targeted at end-plate within injected muscle. Given the high correspondence of acupoints MTrPs, and end-plate zone, the acupoints we used to treat upper-limb spasticity should be near the site of botulinum toxin injection for upper-limb spasticity treatment. Neiguan (PC6) and Shaohai (HT3) should be near the site of botulinum toxin injection to reduce the spasticity at the elbow pronation (motor point of pronater teres and pronator quadricium). Shouzizhu (Ex-UE) should be near the site of botulinum toxin injection to reduce the spasticity when the hands are clenched and when the thumb is placed in the palm (flexor digitorum superficialis and flexor pollicis longus). Zeqian (Ex-UE) should be near the site of botulinum toxin injection to reduce the spasticity of the elbow flexion (Brachioradialis) (Figure 3).37
  | Figure 3 Comparison of acupoints used in this study and motor point of forearm muscle (drawn by Wang). |
Possible mechanism of acupoint selection in spasticity treatment in stroke patients
Several hypotheses about the mechanism of EA in reducing spasticity have been suggested. These hypotheses include the change in neurotransmitter production38–40 and the excitability of the spinal motor neuron.39,41 We may assume that the effect of EA on spasticity may also be related to the stimulation at the motor point of the affected muscle. The correlation between acupoints and motor points was mentioned earlier. Most acupoints in this study were near the motor points of muscles related to elbow movement. No acupoint in this study was near the site of botulinum toxin injection for wrist movement; therefore, there was no significant reduction of spasticity of the wrist joint in this study.
Bedside botulinum toxin injection was mediated via chemical pathway-blocking acetylcholine action on the neuromuscular junction by the botulinum toxin. If EA can achieve a similar effect, it seems to be a better solution for spasticity treatment based on the following reasons: no concern was raised about the side effect caused by medicines, such as muscle weakness caused by inappropriate dose, risk of overdose, nor the possible resistance to botulinum toxin injection treatment because of antibody production.
Liu et al42 have shown that muscle spasticity was significantly decreased and the active range of motion of the wrist joint was increased after a 6-week combined EA treatment and strengthening exercise intervention. The acupoints used in that study were Hegu (LI 4), Houxi (SI 3), Waiguan (TE 5), Quchi (LI 11), Shousanli (LI 10), and Jianyu (LI 15). Most of these acupoints are near the muscle-injection sites for wrist movement; therefore, wrist spasticity could be determined. Therefore, EA can significantly reduce the spasticity in the upper limbs in chronic stroke patients. Moreover, a correlation was observed between acupoints and motor points in treating spasticity.
Possible mechanism of EA treatment for spasticity in stroke patients
The frequency of electrical stimulation can be divided into three categories based on frequency range: low (<10 Hz), middle (10–100 Hz), and high (>100 Hz).38 Studies on acupuncture analgesia have shown that endogenous opioid peptides were released in response to low-frequency electrical stimulation, whereas serotonin and dynorphin were released in high-frequency electrical stimulation.38 Thus, neural mechanisms are dependent on the different frequencies of electrical stimulation. Yu39 and Han et al40 used EA on the surface of two couples of acupoints. They reported that a short-term application (30 minutes) of high-frequency EA (100 Hz) produced an immediate antispastic effect compared with low-frequency EA (2 Hz).39,40 This result might be related to the differences in the released neurotransmitters based on the different frequencies of electrical stimulation.39,40 The mechanism of the effect of EA on spasticity is not fully understood. EA has been proposed to reduce spinal motor-neuron excitability.41 Yu39 inferred that high-frequency EA enhanced the production of dynorphin in the cerebrospinal fluid, and then decreased the excitability of the motor neurons in the anterior horns through kappa-opiate receptors, thereby reduce the muscle spasticity.
Another study on the antispastic effect of EA in stroke patients with elbow spasticity used mid-frequency stimulation (50 Hz). This found that EA temporarily reduced spasticity caused by stroke, and when it was repeatedly applied, the reduction of spasticity was maintained until 5 days after treatment.19 Thus, we used the same frequency stimulation (50 Hz) in the present study, and the results of the present study are in agreement with the previous study, where EA with mid-frequency stimulation had a positive treatment effect on spasticity in stroke patients. Thus, we used different acupoints to prove that the effect of EA was affected not only by frequency but also by acupoint selection. With the same frequency stimulation, our results showed the treatment effect of EA was different at different joints. These differences were related to acupoint selection, where locations near the motor points of the target muscle had a positive treatment effect.
Limitations of this study
A number of spasticity-measuring tools are used, and these range from simple questionnaires and goniometry evaluations to more technologically complicated electromyographic and biomechanical analysis of limb resistance to mechanical displacement and even video-monitoring assessments of joint mobility.5,43,44 The present study was limited because no tool or equipment was used in objectively quantifying spasticity, but the outcome measurements used in this study, such as R1, R2, and R2–R1 over the wrist and elbow joints, have been widely used in previous studies.24
The control group received minimal acupuncture as sham control. Lin et al45 reviewed control-group design in randomized controlled trials of acupuncture. He found that minimal acupuncture had advantages, including the elimination of placebo effect, ensured blinding, and easy manipulation. Its limitation was potential therapeutic effects in the control group. He also mentioned other control design such as transcutaneous electrical nerve stimulation, laser acupuncture, sham-point acupuncture, and placebo needling, with limitations of potential therapeutic effect, inadequate blinding, site limitation, and so forth. A study also showed placebo needling had a greater placebo effect on subjects than placebo pills.46 Therefore, there is need for further research on new techniques or comparisons of sham control design of randomized controlled trials of acupuncture.
Another limitation of the current study is the restrictive sample size. Thus, a larger patient population and incorporating a multicenter trial should be conducted before the treatment is widely promoted. Moreover, the study focused on longer follow-up periods.
Finally, the effect of acupuncture on stroke rehabilitation may be better demonstrated when a subgroup of people with a specific type of stroke is enrolled. Therefore, further research should be performed to confirm our preliminary results.
Conclusion
Our study shows that the combined 6-week EA and SR treatment reduced upper-extremity spasticity and R2–R1 of the elbow joint for chronic stroke survivors. However, no significant effect was observed in the spasticity of wrist joints. The choice of acupoints and the frequency of EA should be varied depending on the target joint to achieve a positive treatment effect, based on the very limited number of patients completed in the study. Furthermore, we provide a preliminary model of acupoint selection where performing EA on motor points would have a treatment effect similar to botulinum toxin injection in reducing spasticity. Further research with longer intervention and larger patient population is needed.
Acknowledgments
This study was supported by a grant from China Medical University Hospital (DMR-98-083 and CTC101-003) and supported in part by the Taiwan Department of Health Clinical Trial and Research Center of Excellence (DOH102-TD-B-111-004).
Disclosure
The authors report no conflicts of interest in this work.
References
Department of Health. 2010 Statistics of Causes of Death. Taipei: Department of Health; 2011:92–98. | |
Lin JH, Chang CM, Huang MH, et al. A follow-up study of first stroke patients after inpatient rehabilitation. Formos J Phys Ther. 2001;26(4):196–204. | |
Yu KW, Lin CL, Hung CC, et al. Effects of electroacupuncture on recent stroke inpatients with incomplete bladder emptying: a preliminary study. Clin Interv Aging. 2012;7:469–474. | |
Sommerfeld DK, Eek EU, Svensson AK, Holmqvist LW, von Arbin MH. Spasticity after stroke: its occurrence and association with motor impairments and activity limitations. Stroke. 2004;35(1):134–139. | |
Braddom RL. Physical Medicine and Rehabilitation. 4th ed. Philadelphia: Elsevier; 2010. | |
Pinedo S, de la Villa FM. Complications in the hemiplegic patient in the first year after the stroke. Rev Neurol. 2001;32(3):206–209. Spanish. | |
Glenn MB, Whyte J. The Practical Management of Spasticity in the Adult and Child. Philadelphia: Lea & Febiger; 1990. | |
Brashear A, Gordon MF, Elovic E, et al. Intramuscular injection of botulinum toxin for the treatment of wrist and finger spasticity after a stroke. N Engl J Med. 2002;347(6):395–400. | |
Zhao JG, Cao CH, Liu CZ, et al. Effect of acupuncture treatment on spastic states of stroke patients. J Neurol Sci. 2009;276(1–2):143–147. | |
Marwick C. Acceptance of some acupuncture applications. JAMA. 1997;278(21):1725–1727. | |
Rabinstein AA, Shulman LM. Acupuncture in clinical neurology. Neurologist. 2003;9(3):137–148. | |
Paek CH, So SW, Kim HS, Ahn KH, Nam SS, Park SK. Antispastic effect of transcutaneous electrical nerve stimulation and acupuncture in the stroke patients. J Korean Acad Rehabil Med. 1997;21(6):1088–1097 Available from: http://www.koreamed.org/SearchBasic.php?RID=0041JKARM/1997.21.6.1088&DT=1. Accessed December 17, 2013. Korean. | |
Sällström S, Kjendahl A, østen PE, Stanghelle JK, Borchgrevink CF. Acupuncture in the treatment of stroke patients in the subacute stage: a randomized, controlled study. Complement Ther Med. 1996;4(3):193–197. | |
Hopwood V. Acupuncture in stroke recovery: a literature review. Complement Ther Med. 1996;4(4):258–263. | |
Naeser MA. Acupuncture in the treatment of paralysis due to central nervous system damage. J Altern Complement Med. 1996;2(1):211–248. | |
Park J, Hopwood V, White AR, Ernst E. Effectiveness of acupuncture for stroke: a systematic review. J Neurol. 2001;248(7):558–563. | |
[No authors listed]. Acupuncture. NIH Consens Statement. 1997;15(5):1–34. | |
Wang DC, Yin JX. China Zhenjiuology. Tianjin: Tianjin Ke Ji Fan Yi Chu Ban Gong Si; 1992. | |
Moon SK, Whang YK, Park SU, et al. Antispastic effect of electroacupuncture and moxibustion in stroke patients. Am J Chin Med. 2003; 31(3):467–474. | |
Schaechter JD, Connell BD, Stason WB, et al. Correlated change in upper limb function and motor cortex activation after verum and sham acupuncture in patients with chronic stroke. J Altern Complement Med. 2007;13(5):527–532. | |
WHO Regional Office for the Western Pacific. WHO Standard Acupuncture Point Locations in the Western Pacific Region. Manila: World Health Organization; 2008. | |
Lee YC. Practical Traditional Chinese Dictionary. Taipei: Jyin; 1996. | |
Cheng DA. China Zhenjiuology. Beijing: People’s Medical; 2008. | |
Singh P, Joshua AM, Ganeshan S, Suresh S. Intra-rater reliability of the modified Tardieu scale to quantify spasticity in elbow flexors and ankle plantar flexors in adult stroke subjects. Ann Indian Acad Neurol. 2011;14(1):23–26. | |
Hsieh RL, Wang LY, Lee WC. Additional therapeutic effects of electroacupuncture in conjunction with conventional rehabilitation for patients with first-ever ischaemic stroke. J Rehabil Med. 2007;39(3):205–211. | |
Dumitru D, Amato AA, Zwarts M. Electrodiagnostic Medicine. Philadelphia: Hanley & Belfus; 1995. | |
Travell JG, Simons DG. Myofascial Pain and Dysfunction: The Trigger Point Manual. Baltimore: Williams & Wilkins; 1983. | |
Simons DG, Travell JG, Simons LS. Myofascial Pain and Dysfunction: The Trigger Point Manual. 2nd ed. Baltimore: Williams & Wilkins; 1999. | |
Gerwin RD, Shannon S, Hong CZ, Hubbard D, Gevirtz R. Interrater reliability in myofascial trigger point examination. Pain. 1997;69(1–2):65–73. | |
Simons DG, Travell J. Myofascial trigger points, a possible explanation. Pain. 1981;10(1):106–109. | |
Simons DG. Review of enigmatic MTrPs as a common cause of enigmatic musculoskeletal pain and dysfunction. J Electromyogr Kinesiol. 2004;14(1):95–107. | |
Cummings M, Baldry P. Regional myofascial pain: diagnosis and management. Best Pract Res Clin Rheumatol. 2007;21(2):367–387. | |
Melzack R, Stillwell DM, Fox EJ. Trigger points and acupuncture points for pain: correlations and implications. Pain. 1977;3(1):3–23. | |
Dorsher PT. Trigger points and acupuncture points: anatomic and clinical correlations. Med Acupunct. 2006;17(3):20–23. | |
Chou LW, Kao MJ, Lin JG. Probable mechanisms of needling therapies for myofascial pain control. Evid Based Complement Alternat Med. 2012;2012:705327. | |
Gracies JM, Lugassy M, Weisz DJ, Vecchio M, Flanagan S, Simpson DM. Botulinum toxin dilution and endplate targeting in spasticity: a double-blind controlled study. Arch Phys Med Rehabil. 2009;90(1):9–16. e2. | |
Henry G, David VD. Gray’s anatomy: descriptive and applied. 33rd ed. London: Longmans;1964. | |
Filshie J, White A. Medical Acupuncture: A Western Scientific Approach. Seoul: KCA; 2001. | |
Yu Y. Transcutaneous electric stimulation at acupoints in the treatment of spinal spasticity: effects and mechanism. Zhonghua Yi Xue Za Zhi. 1993;73(10):593–595, 637. Chinese. | |
Han JS, Chen XH, Yuan Y, Yan SC. Transcutaneous electrical nerve stimulation for treatment of spinal spasticity. Chin Med J (Engl). 1994;107(1):6–11. | |
Kendall DE. A scientific model for acupuncture. Am J Acupunct. 1989;17(3):251–267. | |
Liu W, Mukherjee M, Sun C, Liu H, McPeak LK. Electroacupuncture may help motor recovery in chronic stroke survivors: a pilot study. J Rehabil Res Dev. 2008;45(4):587–595. | |
Burry HC. Objective measurement of spasticity. Dev Med Child Neurol. 1972;14(4):508–510. | |
Norton BJ, Bomze HA, Chaplin H Jr. An approach to the objective measurement of spasticity. Phys Ther. 1972;52(1):15–24. | |
Lin JG, Chen CH, Huang UC, Chen YH. How to design the control group in randomized controlled trials of acupuncture. Evid Based Complement Alternat Med. 2012;2012:875284. | |
Kaptchuk TJ, Stason WB, Davis RB, et al. Sham device v inert pill: randomised controlled trial of two placebo treatments. BMJ. 2006;332(7538):391–397. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

