Back to Journals » Clinical Epidemiology » Volume 13
Second Primary Cancers After Gastric Cancer, and Gastric Cancer as Second Primary Cancer
Authors Zheng G , Sundquist K, Sundquist J , Chen T , Försti A , Hemminki A , Hemminki K
Received 28 January 2021
Accepted for publication 1 March 2021
Published 2 July 2021 Volume 2021:13 Pages 515—525
DOI https://doi.org/10.2147/CLEP.S304332
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Vera Ehrenstein
Guoqiao Zheng,1– 3 Kristina Sundquist,3– 5 Jan Sundquist,3– 6 Tianhui Chen,7 Asta Försti,1,3,8,9 Akseli Hemminki,10,11 Kari Hemminki1– 3,12
1Division of Molecular Genetic Epidemiology, German Cancer Research Center (DKFZ), Heidelberg, Germany; 2Division of Cancer Epidemiology, German Cancer Research Center (DKFZ), Heidelberg, Germany; 3Center for Primary Health Care Research, Lund University, Malmö, Sweden; 4Department of Family Medicine and Community Health; 5Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, USA; 6Center for Community-Based Healthcare Research and Education (CoHRE), Department of Functional Pathology, School of Medicine, Shimane University, Matsue, Shimane, Japan; 7Department of Cancer Prevention, Cancer Hospital of the University of Chinese Academy of Sciences (Zhejiang Cancer Hospital), Institute of Basic Medicine and Cancer, Chinese Academy of Sciences, Hangzhou, 310022, People’s Republic of China; 8Hopp Children’s Cancer Center (KiTZ), Heidelberg, Germany; 9Division of Pediatric Neurooncology, German Cancer Research Center (DKFZ), German Cancer Consortium (DKTK), Heidelberg, Germany; 10Cancer Gene Therapy Group, Translational Immunology Research Program, University of Helsinki, Helsinki, Finland; 11Comprehensive Cancer Center, Helsinki University Hospital, Helsinki, Finland; 12Biomedical Center, Faculty of Medicine and Biomedical Center in Pilsen, Charles University in Prague, Pilsen, 30605, Czech Republic
Correspondence: Kari Hemminki
Biomedical Center, Charles University Medical Faculty in Pilsen, Pilsen, 30605, Czech Republic
Email [email protected]
Background: Second primary cancers (SPCs) are increasing, which may negatively influence patient survival. Gastric cancer (GC) has poor survival and when it is diagnosed as SPC it is often the cause of death. We wanted to analyze the risk of SPCs after GC and the risk of GC as SPC after any cancer. Such bidirectional analysis is important in relation to fatal cancers because SPCs may be under-reported in the short-term survival period.
Methods: Cancers were obtained from the Swedish Cancer Registry from years 1990 through 2015. Standardized incidence ratios (SIRs) were used to estimate bidirectional relative.
Results: We identified 23,137 GC patients who developed 1042 SPCs (4.5%); 2158 patients had GC as SPC. While the risk for three SPCs was increased after GC, seven first primary cancers were followed by an increased risk of GC as SPC, including esophageal, colorectal, bladder, squamous cell skin and breast cancers and non-Hodgkin lymphoma. Breast cancer, which was followed by a diagnosis of second GC, showed an excess of lobular histology.
Conclusion: Multiple primary cancers in the same individuals may signal genetic predisposition. Accordingly, the association of GC with breast cancer may be related to mutations in the CDH1 gene, and clustering of colorectal, small intestinal and bladder cancers could be related to Lynch syndrome. The third line of findings supports a contribution of immune dysfunction on the increased risk of GC as SPC after skin cancer and non-Hodgkin lymphoma. Early detection of GC in the risk groups could save lives.
Keywords: cancer incidence, relative risk, second primary cancer, cancer etiology, stomach cancer
Introduction
Gastric (stomach) cancer (GC) has historically been the most common cancer in the world.1–3 Although the incidence of GC has gradually fallen it is still among the main fatal cancers, however with a large international variation.4 Although survival rates in GC have been improving, prognosis remains poor; the 5-year survival rate is at 20–25%.5,6 In Sweden, GC 5-year survival has increased in men from 12 to 24% between 1967 and 2016, and in women from 13 to 28% according to the NORDCAN database (https://www-dep.iarc.fr/NORDCAN/english/frame.asp). Survival is better in Japan and South Korea where population screening has been implemented.7,8 The anatomic location of the tumor has important pathophysiological implications. Tumors in the cardia at the gastroesophageal junction are rarer than non-cardia tumors; obesity and the related gastroesophageal reflux are risk factors for cardia cancer, while for non-cardia disease Helicobacter pylori infection and dietary factors (see below) are important.4 Distant metastases from GC are most commonly found in the liver; cardia tumors additionally metastasize to the lung, nervous system and bone, whereas non-cardia cancers more frequently metastasize within the peritoneum.9 Treatment of GC involves endoscopic mucosal resection for localized disease and gastrectomy for advanced disease, supplemented with chemotherapy and radiotherapy, and in Her2 positive cases targeted therapy.10 The declining trend in GC incidence has been ascribed to the falling rates of non-cardia cancer concomitant with declining rates in H. pylori infections as a result of improved household hygiene and widespread antibiotic use.7 Other risk factors include tobacco smoking, high-salt diet, poorly preserved food, excess alcohol intake, obesity, and low intake of fresh fruits and vegetables.10 Family history is another rare risk factor; hereditary GC is associated with mutations in the CDH1 gene, and GC is manifested in Lynch syndrome related to mutations in mismatch repair genes.11–14 Next-generation sequencing studies have identified rare germline variants in several other genes, including BRCA2 and many other DNA repair genes.15–17
Second primary cancers (SPCs) are increasing as improving survival increases the likelihood of being diagnosed with another cancer.18 Because survival in GC is poor, SPCs are less common and these may also be underreported as the care is focused on GC.19,20 Population-based literature on SPCs after GC is not extensive. Portugal is a high-risk area of GC, and an increase in SPCs was observed for esophageal, small intestinal and colon cancers in both sexes.21 The same authors reported an increased risk of GC as SPC when esophageal and colon cancers were first primary cancers (FPCs).22 In a Swedish study, the risk of GC as SPC was increased after esophageal, breast, ovarian, cervical, testicular and squamous cell skin cancers and non-Hodgkin lymphoma, Hodgkin lymphoma and myeloma.23 Patients diagnosed with colon and breast cancers as FPC and with a family history of these cancers experienced an increased risk of second GC.23 In a nation-wide analysis in Taiwan, increased risks for SPCs were found for cancer overall and cancers of the head and neck, esophagus, colon and rectum, bones and soft tissues, ovaries, bladder and kidneys, as well as non-Hodgkin lymphoma;24 radiotherapy and particularly chemotherapy were independent risk factors.
Considering the modestly improved survival in GC we decided to examine the risks of any cancer after GC, and also systematically bidirectionally, the risk of GC as SPC after any FPC. Because of the concerns of possible underreporting of SPCs after GC, it is instructive to compare results to the inverse association, GC as SPC.20 Cardia and non-cardia cancers were assessed separately.
Patients and Methods
Nation-wide population and cancer data were obtained from Statistics Sweden and the Swedish Cancer Registry, and these were delivered to us in a pseudonymized format. We have no access to any keys of the pseudonymized data including personal information, such as name, address, or personal ID numbers. GC was identified by the codes of the International Classification of Diseases revision 7 (ICD-7 and later revisions) distinguishing cardia and other parts (ie, non-cardia). Lauren’s classification into diffuse and intestinal types was not used. Practically all cancers, including SPCs, are histologically verified in the Swedish Cancer Registry.25 This should in most cases distinguish recurrences from independent primaries.
Data on GC and other cancers covered years 1990 through 2015. The other cancers include any of 23 common male and 24 female FPCs or SPCs. Patients were followed up from 1990 onward from the diagnosis of FPC until the end of 2015 or diagnosis of SPC, immigration or death, whichever came earliest. Only discordant (different) FPC-SPC pairs were included. Upper aerodigestive tract (UAT) included lip, oral cavity, pharynx and larynx. Kidney cancer included only renal cell carcinoma; renal pelvic and ureteral cancers were also considered but case numbers were few and not reported. For skin cancer, only melanoma and squamous cell carcinoma (SCC) were included.
Standardized incidence ratios (SIRs) for SPCs were estimated through the observed number of SPCs divided by the expected number of cases. The expected numbers of cancers were estimated by the person-years after first primary cancer diagnosis, multiplied by the incidence of the same cancer as FPC in the general population. The estimation was done for both sexes combined and separately, and adjusted for age, calendar year, place of residence and socioeconomic factors. The 95% confidence interval (95% CI) for SIR was calculated by assuming Poisson distribution. Chi-square test, or Fisher exact test if appropriate, was used to test the difference of frequency. The statistical tests were two-tailed and P value < 0.05 was regarded as significant, and an increase in risk was called only when P value was significant. All the analyses were performed in SAS 9.4.
Incidence, mortality and survival data were obtained from the NORDCAN database (https://www-dep.iarc.fr/NORDCAN/english/frame.asp), which is a compilation of data from the Nordic cancer registries, including the Swedish Cancer Registry, as described.26
Results
A dramatic decrease in the incidence (and consequently in mortality) of GC is shown for Sweden in Figure 1, based on the NORDCAN database. Male and female incidence has declined to about 20% within 50 years.
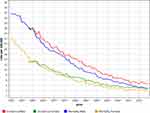 |
Figure 1 Incidence and mortality for gastric cancer among Swedish men and women. The data are derived from the NORDCAN database and are adjusted to the world standard population. |
During the follow-up period of 1990 to 2015, we identified 23,137 GC patients who developed 1042 SPCs (4.5%). Among GCs, 4764 patients had cardia cancer (75.6% male, median diagnostic age 78 years, interquartile range, IQR, 70–84) and 17,927 had non-cardia cancer (56.9% male, median diagnostic age 75 years, IQR 66–81). The total number of other cancers considered was 1,035,682 (51.7% male). The median (IQR) time from first GC to SPC was 34.5 (4–93) months and from FPC to second GC it was 41 (14–87) months.
SIRs for SPCs of combined sexes associated with GC are shown in Table 1. The overall risk for SPCs after GC was decreased (SIR 0.91), based on 1042 cases. Risks for three individual SPCs were significantly increased: small intestinal (4.12), esophageal (2.15) and kidney (1.62) cancers. The SIRs of also three cancers were decreased, including lung and prostate cancers and myeloma. In the reversed order, GC as SPC, the overall SIR was 1.05 with 2158 cases. Risks were increased for GC after seven FPCs, most after esophageal (2.43), skin SCC (1.39) and UAT (1.35) cancers and non-Hodgkin lymphoma (NHL, 1.32). Three FPCs were followed by a decreased risk of GC; these were pancreatic and prostate cancers and melanoma.
 |
Table 1 Risks of SPC After Gastric Cancer and Risks of Gastric Cancer as SPC |
Sex-specific analyses are presented in Tables 2 and 3. There are small differences to Table 1, considering the lower case numbers. Notably, the overall SIR for SPCs was 0.84 for men but it was 1.06 for women. Among women, colorectal cancer (CRC) was bidirectionally associated with GC, and female kidney cancer SIR was 2.38 as SPC.
 |
Table 2 Male Risk of SPC After Gastric Cancer and Risks of Gastric Cancer as SPC |
 |
Table 3 Female Risk of SPC After Gastric Cancer and Risks of Gastric Cancer as SPC |
Table 4 shows bidirectional results for cardia and non-cardia cancers. Cardia cancers are rare and so were significant associations. Esophageal cancer was bidirectionally associated with high SIRs. Risk of cardia cancer was increased after female genital cancer (4.89) and UAT cancer (1.72). After non-cardia cancer, risks of small intestinal and kidney cancers were increased as SPC. Small intestinal cancer showed a bidirectional association. Other FPCs which were associated with non-cardia cancer as SPC were CRC, breast, bladder and skin cancers, and thyroid cancer as a novel association (1.85).
 |
Table 4 Risks of SPC After Gastric (Cardia and Non-Cardia) Cancer and Risks of Gastric Cancer as SPC |
We assessed histological distributions and diagnostic ages of probands for some cancers with increased SIRs when diagnosed after 1990; the hypothesis was to search evidence for mutations in CDH1 (ie, proportion of lobular breast cancer) or BRCA1/2 (ie, proportion of family members with breast cancer who had second breast or ovarian cancer) as genetic predisposing factors. For 246 female breast cancer patients from Table 3, 19.1% (47/246) were diagnosed with lobular histology, while the proportion of lobular breast cancer for all women was 11.2% (13,531/120,810; Chi-square P < 0.0001). These 246 breast cancer patients (Table 3) had 313 female family members, and 12 of them were diagnosed with breast cancer; of them, 4 (25%) were further diagnosed with second breast or second ovarian cancer. For all the women with breast cancer, 245,489 family members were found. Among them, 11,896 had breast cancer and 1400 (11.8%) were further diagnosed with second breast or second ovarian cancer; the difference to the GC probands was not significant (Fisher P=0.11).
Discussion
GC is a fatal cancer which is diagnosed at a high age (median age at diagnosis 76 years compared to all cancers of 70 years). According to the present results, it is likely that SPCs after GC are underreported among men as the overall SIR for SPCs was below 1.00 (0.84) while for women it was 1.06. SIRs below 1.00 were noted for fatal cancers (lung, pancreas, myeloma) or cancers in elderly men (prostate). This may imply some underestimation of risks for male SPCs after GC. For women, there was no such indication of underreporting but their overall case numbers were smaller than those for men and statistical power was accordingly lower. In addition to the previously reported increases for esophageal and small intestinal cancers as SPCs, for which the anatomic proximity and the same kind of intestinal lining are likely to play a role, an association was observed for kidney cancer, particularly among women and at the non-cardia location. As the association was noted only for kidney cancer as SPC, and not in reverse order, it may be a fortuitous finding during GC diagnostic work-up; carcinogenic effects of adjuvant radiation/chemoradiation for GC could also play a role.
GC is an associated cancer in Lynch syndrome, in which cumulative risk for GC in individuals with germline mutations in mismatch repair genes MLH1 and MSH2 was increased about 9-fold by age 75 years; yet the increased risk was observed only in patients aged 70 or more years.13 The observed associations of second GC with CRC, small intestinal (in non-cardia GC) and bladder cancers could be due to shared predisposition to mutations in mismatch repair genes.13 Yet the lacking risk of endometrial cancer contradicts this hypothesis. However, an explanation may be the relatively early median age of onset for endometrial cancer in Lynch syndrome (48 years).27,28 Thus, CRC with a median age of onset at 44 years, and a much commoner cancer than GC in Lynch syndrome, would be the likeliest SPC after endometrial cancer.28
The association of GC with breast cancer poses the question if CDH1 mutations may be involved, as lobular breast cancer manifests in CDH1-related cancers.11 Indeed, lobular breast cancer was in excess as FPCs followed by GC, supporting the likelihood of CDH1 predisposition. We tested also if some evidence for the role of BRCA1/2 could be found, but low case numbers for pathognomonic clustering of cancers did not allow conclusions.
A further cluster of FPCs that showed a risk for GC as SPCs was skin SCC and NHL. High risk for this combination of neoplasms is known for immunocompromised individuals, such as kidney transplant patients.29–31 An increased risk of GC as SPC has been found in studies analyzing SPCs after NHL and skin SCC.32,33 It was also shown that family history of GC increased the likelihood of second GC in NHL patients.34 We thus consider plausible that the increased risk for second GCs after skin SCC and NHL may have an immunological component. As an additional contributing factor could be mucosa-associated lymphoid tissue (MALT) lymphoma, for which the most commonly affected organ is the stomach. The underlying mechanism is chronic gastritis induced by H. pylori.35 The Swedish Cancer Registry does not consider affected organs for lymphomas, and thus any MALT lymphoma would be classified under NHL. The median diagnostic age of MALT lymphoma is 67 years and it is quite possible that GC would be diagnosed after MALT lymphoma.36 Even though MALT lymphoma is less than 10% of all NHL, the reported risk of GC (4.3) is relatively high.37
Limitations of the study are several. A cancer registry has no information on individual treatment nor on lifestyle factors. However, we were able to adjust for socioeconomic factors, which reflect many aspects of lifestyle. While the overall reporting of SPCs is high, we have no specific information on reporting after GC.25,38 As the distribution of GC has a large geographical variation, the results may be generalized only to regions with a similar GC incidence as Sweden. Finally, there is no information on the population frequency of CDH1 mutations in Sweden. This being the case, it is not possible to evaluate how applicable the proposed guidelines for the management of mutation carriers would be.39
In conclusion, multiple primary cancers in the same individual are one of the hallmarks of genetic predisposition, which in the present study suggested contribution by hereditary CDH1-related GC and Lynch syndrome. Lobular breast cancer is a manifestation of CDH1 predisposition and we showed that breast cancers, which preceded GC had an over-representation of lobular histology. The signs of Lynch syndrome were found in an increased risk of second GC after CRC, small intestinal and bladder cancers. The third line of findings suggested immune dysfunction as a contributing mechanism for the excess GC as SPC after skin SCC and NHL. While GC is fatal as FPC, it is so also as SPC; for example, most breast or ovarian cancer and NHL patients who were diagnosed with second GC also died of GC.34,40,41 Even though Western countries, as opposed to Asian countries, have not adopted population screening for GC, application of early detection methods, such as gastroscopy, could be considered for risk groups.8 According to the present results, such risk groups could be breast and intestinal cancer patients with a family history of gastric cancer.
Statement on Ethics
The study was approved on 25 January, 2013 by the Regional Ethical Review Board in Lund without the requirement for informed consent (registration number 2012/795). Instead, the Ethical Review Board obliged us to advertise in the newspapers in order to inform the public that their data would be used for secondary purposes. After that, around 40 individuals were excluded (≈40 excluded individuals/≈10 million individuals in the Swedish population).
Acknowledgments
G.Z was a doctoral student supported by the China Scholarship Council (201606100057).
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Supported by the European Union’s Horizon 2020 research and innovation programme, grant No 856620 (Chaperon), the Swedish Research Council, the Swedish Research Council, Jane and Aatos Erkko Foundation, Sigrid Juselius Foundation, Finnish Cancer Organizations, University of Helsinki, Helsinki University Central Hospital, Novo Nordisk Foundation, Päivikki and Sakari Sohlberg Foundation.
Disclosure
A.H. is a shareholder in Targovax ASA. A.H. reports personal fees and is an employee and shareholder in TILT Biotherapeutics Ltd. The other authors declared no conflicts of interest.
References
1. Peery TM. The new and old diseases: a study of mortality trends in the United States, 1900–1969 Ward Burdick award address. Am J Clin Pathol. 1975;63(4):453–474. doi:10.1093/ajcp/63.4.453
2. Wingo PA, Cardinez CJ, Landis SH, et al. Long-term trends in cancer mortality in the United States, 1930–1998. Cancer. 2003;97(S12):3133–3275. doi:10.1002/cncr.11380
3. Balakrishnan M, George R, Sharma A, Graham DY. Changing trends in stomach cancer throughout the world. Curr Gastroenterol Rep. 2017;19(8). doi:10.1007/s11894-017-0575-8
4. Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric cancer. Lancet. 2020;396(10251):635–648. doi:10.1016/s0140-6736(20)31288-5
5. Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64(1):9–29. doi:10.3322/caac.21208
6. Munro AJ. Comparative cancer survival in European countries. Br Med Bull. 2014;110(1):5–22. doi:10.1093/bmb/ldu009
7. Etemadi A, Safiri S, Sepanlou SG, et al. The global, regional, and national burden of stomach cancer in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease study 2017. Lancet Gastroenterol Hepatol. 2020;5(1):42–54. doi:10.1016/s2468-1253(19)30328-0
8. Suh YS, Yang HK. Screening and early detection of gastric cancer: east versus west. Surg Clin North Am. 2015;95(5):1053–1066. doi:10.1016/j.suc.2015.05.012
9. Riihimaki M, Hemminki A, Sundquist K, Sundquist J, Hemminki K. Metastatic spread in patients with gastric cancer. Oncotarget. 2016;7(32):52307–52316. doi:10.18632/oncotarget.10740
10. Marghalani AM, Bin Salman TO, Faqeeh FJ, Asiri MK, Kabel AM. Gastric carcinoma: insights into risk factors, methods of diagnosis, possible lines of management, and the role of primary care. J Family Med Prim Care. 2020;9(2659–2663). doi:10.4103/jfmpc.jfmpc_527_20
11. Shenoy S. CDH1 (E-Cadherin) mutation and gastric cancer: genetics, molecular mechanisms and guidelines for management. Cancer Manag Res. 2019;11(10477):10477–10486. doi:10.2147/cmar.S208818
12. Kharazmi E, Babaei M, Fallah M, et al. Importance of tumor location and histology in familial risk of upper gastrointestinal cancers: a nationwide cohort study. Clin Epidemiol. 2018;10(1169):1169–1179. doi:10.2147/clep.S168152
13. Møller P, Seppälä TT, Bernstein I, et al. Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age: a report from the prospective lynch syndrome database. Gut. 2018;67(7):1306–1316. doi:10.1136/gutjnl-2017-314057
14. Marwitz T, Hüneburg R, Spier I, et al. Hereditary diffuse gastric cancer: a Comparative Cohort Study according to pathogenic variant status. Cancers. 2020;12(12):3726. doi:10.3390/cancers12123726
15. Zhu Z, Fu H, Wang S, et al. Whole-exome sequencing identifies prognostic mutational signatures in gastric cancer. Ann Transl Med. 2020;8(22):1484. doi:10.21037/atm-20-6620
16. Iyer P, Moslim M, Farma JM, Denlinger CS. Diffuse gastric cancer: histologic, molecular, and genetic basis of disease. Transl Gastroenterol Hepatol. 2020;5(52):52. doi:10.21037/tgh.2020.01.02
17. Slavin TP, Weitzel JN, Neuhausen SL, et al. Genetics of gastric cancer: what do we know about the genetic risks? Transl Gastroenterol Hepatol. 2019;4(4):55. doi:10.21037/tgh.2019.07.02
18. Travis LB, Demark Wahnefried W, Allan JM, Wood ME, Ng AK. Aetiology, genetics and prevention of secondary neoplasms in adult cancer survivors. Nat Rev Clin Oncol. 2013;10(5):289–301. doi:10.1038/nrclinonc.2013.41
19. Chen T, Fallah M, Jansen L, et al. Distribution and risk of the second discordant primary cancers combined after a specific first primary cancer in German and Swedish cancer registries. Cancer Lett. 2015;369(1):152–166. doi:10.1016/j.canlet.2015.08.014
20. Liu H, Hemminki K, Sundquist J, et al. A population-based comparison of second primary cancers in Germany and Sweden between 1997 and 2006: clinical implications and etiologic aspects. Cancer Med. 2013;2(5):718–724. doi:10.1002/cam4.116
21. Morais S, Antunes L, Bento MJ, Lunet N. Risk of second primary cancers among patients with a first primary gastric cancer: a population-based study in North Portugal. Cancer Epidemiol. 2017;50(85):85–91. doi:10.1016/j.canep.2017.08.007
22. Morais S, Antunes L, Bento MJ, Lunet N. Second primary gastric cancers in a region with an overall high risk of gastric cancer. Gac Sanit. 2020;34(4):393–398. doi:10.1016/j.gaceta.2018.08.010
23. Ji J, Hemminki K. Second gastric cancers among patients with primary sporadic and familial cancers in Sweden. Gut. 2006;55(6):896–898. doi:10.1136/gut.2005.090118
24. Chen SC, Liu C-J, Hu Y-W, et al. Second primary malignancy risk among patients with gastric cancer: a nationwide population-based study in Taiwan. Gastric Cancer. 2016;19(2):490–497. doi:10.1007/s10120-015-0482-3
25. Pukkala E, Engholm G, Højsgaard Schmidt LK, et al. Nordic cancer Registries - an overview of their procedures and data comparability. Acta Oncol. 2018;57(4):440–455. doi:10.1080/0284186x.2017.1407039
26. Engholm G, Ferlay J, Christensen N, et al. NORDCAN–a Nordic tool for cancer information, planning, quality control and research. Acta Oncol. 2010;49(5):725–736. doi:10.3109/02841861003782017
27. Meyer LA, Broaddus RR, Lu KH. Endometrial cancer and Lynch syndrome: clinical and pathologic considerations. Cancer Control. 2009;16(1):14–22. doi:10.1177/107327480901600103
28. Ryan NAJ, Morris J, Green K, et al. Association of mismatch repair mutation with age at cancer onset in lynch syndrome: implications for stratified surveillance strategies. JAMA Oncol. 2017;3(12):1702. doi:10.1001/jamaoncol.2017.0619
29. Birkeland S, Storm HH, Lamm LU, et al. Cancer risk after renal transplantation in the Nordic countries, 1964–1986. Int J Cancer. 1995;60(2):183–189. doi:10.1002/ijc.2910600209
30. Hortlund M, Arroyo Mühr LS, Storm H, et al. Cancer risks after solid organ transplantation and after long-term dialysis. Int J Cancer. 2017;140(5):1091–1101. doi:10.1002/ijc.30531
31. Rama I, Grinyo JM. Malignancy after renal transplantation: the role of immunosuppression. Nat Rev Nephrol. 2010;6(9):511–519. doi:10.1038/nrneph.2010.102
32. Chattopadhyay S, Sud A, Zheng G, et al. Second primary cancers in non-Hodgkin lymphoma: bi-directional analyses suggesting role for immune dysfunction. Int J Cancer. 2018;143(10):2449–2457. doi:10.1002/ijc.31801
33. Chattopadhyay S, Hemminki A, Försti A, et al. Second primary cancers in patients with invasive and in situ squamous cell skin carcinoma, Kaposi sarcoma and Merkel cell carcinoma: role for immune mechanisms? J Invest Dermatol. 2020;140(1):48–55.e1. doi:10.1016/j.jid.2019.04.031
34. Chattopadhyay S, Zheng G, Sud A, et al. Second primary cancers in non-Hodgkin lymphoma: family history and survival. Int J Cancer. 2020;146(970–976). doi:10.1002/ijc.32391
35. Mullangi S, Lekkala MR. StatPearls (StatPearls PublishingCopyright © 2020). StatPearls Publishing LLC; 2020.
36. Matysiak-Budnik T, Jamet P, Ruskoné-Fourmestraux A, et al. Gastric MALT lymphoma in a population-based study in France: clinical features, treatments and survival. Aliment Pharmacol Ther. 2019;50(6):654–663. doi:10.1111/apt.15409
37. Palmela C, Fonseca C, Faria R, et al. Increased risk for metachronous gastric adenocarcinoma following gastric MALT lymphoma-A US population-based study. United European Gastroenterol J. 2017;5(4):473–478. doi:10.1177/2050640616671643
38. Frödin J-E, Ericsson J, Barlow L. Multiple primary malignant tumors in a national cancer registry: reliability of reporting. Acta Oncol. 1997;36(5):465–469. doi:10.3109/02841869709001300
39. Blair VR, McLeod M, Carneiro F, et al. Hereditary diffuse gastric cancer: updated clinical practice guidelines. Lancet Oncol. 2020;21(8):e386–e397. doi:10.1016/s1470-2045(20)30219-9
40. Zheng G, Hemminki A, Försti A, et al. Second primary cancer after female breast cancer: familial risks and cause of death. Cancer Med. 2019;8(1):400–407. doi:10.1002/cam4.1899
41. Zheng G, Chattopadhyay S, Forsti A, Sundquist K, Hemminki K. Familial risks of second primary cancers and mortality in ovarian cancer patients. Clin Epidemiol. 2018;10(1457):1457–1466. doi:10.2147/clep.S174173
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
