Back to Journals » Vascular Health and Risk Management » Volume 15
Screening for obstructive sleep apnea among patients undergoing coronary catheterization in Jordan
Authors Jarrah MI , Yassin AM , Ibdah RK , Ibnian AM , Eyadeh AA , Khassawneh BY
Received 29 January 2019
Accepted for publication 11 April 2019
Published 1 May 2019 Volume 2019:15 Pages 109—113
DOI https://doi.org/10.2147/VHRM.S203307
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Daniel Duprez
Mohamad I Jarrah,1 Ahmed M Yassin,2 Rasheed K Ibdah,1 Ali M Ibnian,1 Ahmad A Eyadeh,1 Basheer Y Khassawneh1
1Department of Internal Medicine, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 2Department of Neuro sciences, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan
Aims: This study aimed to utilize a validated sleep questionnaire as a screening tool for symptoms and risk of obstructive sleep apnea in patients undergoing coronary catheterization in Jordan.
Materials and methods: A cross-sectional design was used to screen adult patients undergoing coronary catheterization for obstructive sleep apnea (OSA). The Berlin sleep questionnaire was used to record nocturnal and daytime symptoms of OSA and to stratify patients into “low-risk” or “high-risk” for OSA. Coronary artery disease was defined as ≥50% intraluminal stenosis in at least one coronary vessel.
Results: A total of 398 patients were studied, mean age was 58.7 years (SD=10.70), ranging from 21–92 years, and 68.6% were males. Based on the Berlin sleep questionnaire’s definition, 176 patients (44.2%) were at high-risk for obstructive sleep apnea. Snoring was reported by 61%; loud in 42.1%, and frequent in 62%. Daytime sleepiness was reported by 36%, and 18.9% had fallen asleep while driving. Witnessed apnea during sleep was less reported (7.8%). Prevalence of symptoms and risk of OSA were not different between patients with and without coronary artery disease, P>0.05. In addition, logistic regression indicated that there was no significant association between risk of OSA and coronary artery disease, adjusted (odds ratio=0.93, 95% Confidence Interval=0.60–1.44, P=0.752).
Conclusions: Symptoms and risk of obstructive sleep apnea were common among adult Jordanians undergoing coronary catheterization. There was no association between risk of obstructive sleep apnea and coronary artery disease. Larger studies are needed to assess the role of screening for obstructive sleep apnea in this patient population.
Keywords: obstructive sleep apnea, coronary artery disease, snoring, screening, Berlin sleep questionnaire, coronary catheterization
Introduction
Obstructive sleep apnea (OSA) is the most common sleep breathing disorder. It is characterized by repetitive cessation of airflow in the upper airways during sleep with consequent oxygen desaturations, fragmented sleep, and excessive daytime sleepiness.1 In an earlier study, 17% of adult Jordanians attending primary care clinics were at high-risk of having OSA, and the majority were not diagnosed.2 Coronary artery disease (CAD) is the leading cause of mortality in adults, and it remains responsible for about one-third or more of all deaths in individuals over age 35 years.3,4 Epidemiological studies have shown a strong association between OSA and hypertension and metabolic syndrome as major risk factors for CAD. Moderate-to-severe OSA has been shown to increase the risk and mortality from cardiovascular diseases (CVD), including fatal and non-fatal CAD.5–7
OSA has been associated with increased morbidity and mortality and increased risk of cardiovascular events including CAD, atrial fibrillation, and stroke.8–11 More specifically, the estimated prevalence of OSA in patients with CAD ranges between 26% and 69%.12 In Saudi Arabia, the overall prevalence of OSA was 56.4% in patients with CAD.13 Moreover, poor and fragmented sleep in subjects with OSA may result in cognitive impairment,14 and increased risk of road traffic accidents.15 Despite the significant impact of OSA on the affected individuals, it is still largely underdiagnosed and undertreated.2,16
There is a scarcity in the studies that assess the risk of OSA among patients undergoing coronary catheterization (CATH). Therefore, this study aimed to use a validated sleep screening questionnaire to describe the prevalence of symptoms of OSA and to estimate the risk of OSA in patients undergoing CATH. Identifying subjects at high-risk of OSA will facilitate proper referral for a diagnostic sleep study, and initiate appropriate therapy.
Materials and methods
Study design and setting
A cross-sectional descriptive study was conducted among patients who were planned to undergo CATH at Princess Mona Cardiac center, King Abdullah University Hospital, Irbid, Jordan. The center includes two CATH units and a cardiac surgery unit. This study was approved and conducted in accordance with the Declaration of Helsinki and the ethical standards of the Institutional Review Board of Jordan University of Science and Technology, Irbid, Jordan.
Sample and sampling technique
A convenient sampling method was used to recruite a convenience sample of adult patients (≥18 years old) who were planned to undergo CATH from April to June 2017. Screening was done during the initial evaluation for the CATH (n=480), and 82 patients were excluded for unstable condition, emergency CATH during the off hours and the weekends, and those with incomplete questionnaire items. The power analysis calculation indicated that a minimum of 375 patients was required, with the confidence interval of 4%, 95% confidence level, and estimated number of 1,000 patients admitted annually to the hospital and underwent CATH. An additional 23 participants were added to have 398 patients in the final sample size.
Data collection procedure
All participants who met the eligible criteria were invited to participate in the study and to complete the consent form. Patients who agreed to participate were asked to fill the study questionnaire before the CATH was performed and during a face-to-face interview by the primary investigator. The Arabic version of Berlin sleep questionnaire was used.17 The original version was adopted and validated as a self-report screening instrument for OSA.18 It consists of ten questions, divided into three categories. The first category addresses the presence of snoring, its loudness, frequency, whether it bothers other people, and the frequency of witnessed apnea. The second category addresses the frequency of feeling tired or fatigued after sleep and during wake time, and the tendency and frequency to falling asleep while driving a vehicle. The third category addresses the presence of hypertension and obesity [body mass index (BMI) ≥30 kg/m2]. The validated scoring system of the questionnaire was used to stratify patients into either “low-risk” or “high-risk” for having OSA.18 Subjects who scored positive in two or more categories were considered as “high-risk” for OAS, otherwise they were considered “low-risk”. The findings of the CATH were reported by the interventional cardiologist, and CAD was defined as having at least one coronary vessel with >50% intraluminal stenosis.
Statistical analysis
Data were analyzed using IBM Statistical Package for Social Sciences software (SPSS) for Windows, Version 24.0 (IBM Corp, Armonk, NY). Data were described using means (M) and standard deviation (SD) for continuous variables, and the number and percentages for categorical variables. Differences between categorical values were analyzed using chi-square test. Independent t-test was used to compare means of continuous variables. Multivariate logistic regression analysis was performed to identify potential association between CAD and risk of OSA. A P-value of <0.05 was considered statistically significant.
Results
During the study period, 398 were included in the analysis. Mean age was 58.7 years (SD=10.7) (range=21–92 years), and 273 (68.6%) were males. Most of the participants had hypertension (66.6%), and 28.6% were obese. A total of 265 patients (66.6%) were found to have CAD. Their demographics and clinical characteristics are shown in Table 1.
 | Table 1 Demographics of the study population according to obstructive sleep apnea risk stratification (n=398) |
Based on the Berlin questionnaire scoring criteria, 176 patients (44.2%) were at high-risk for OSA. Snoring was reported by 60%, and described as loud in 25% and frequent in 37%. Witnessed apneas were reported less (7.8%). Daytime sleepiness was reported by 35.9%, and 13% reported falling asleep while driving. Table 2 describes the findings of all items of the Berlin Questionnaire according to CAD status. There were no significant differences in the prevalence of all items of the BSQ between patients with CAD or without CAD.
 | Table 2 The findings of the Berlin Sleep Questionnaire and coronary artery disease status (n=398) |
Multivariate logistic regression analysis was performed to identify any potential association between risk of OSA and having CAD. Odds ratio (OR) was adjusted for risk factors of CAD including age, male gender, diabetes mellitus, and cigarettes smoking. There was no significant association between OSA and CAD, (adjusted OR=0.93, 95% CI=0.60–1.44, P=0.752) (Table 3).
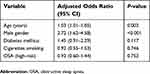 | Table 3 Multivariate logistic regression model of the association between risk of OSA and coronary artery disease adjusted for major risk factors for coronary artery diseases (n=398) |
Discussion
This study used the well-known Berlin sleep questionnaire to describe symptoms and risk of OSA among patients undergoing CATH. Nearly half of these patients were at high-risk of having OSA. Major symptoms of OSA (snoring and daytime sleepiness) were also common. However, the results did not show a significant association between risk of OSA and the presence of CAD.
Our findings are consistent with previous reports of high prevalence of OSA in patients with CAD compared with the general population. The estimated risk for OSA in the US general population is 5–15%.19,20 In Jordan, 16.8% of individuals attending primary care were at high risk for OSA, 28.7% reported having snoring, and 34% had daytime sleepiness.2 The prevalence of OSA is higher among patients with CAD (26–69%).12 Similarly, a regional study from Saudi Arabia showed high prevalence of OSA among patients with CAD, with 82% of their patients at risk of OSA and 56.4% had polysomnography confirmed OSA.13 Our study showed similar results, with almost one in two patients with angiographically proven CAD at high-risk for OSA. Also, the main symptoms of OSA were similarly common. However, there was no difference in the prevalence of symptoms and risk of OSA between those with and without angiographic evidence of CAD. The lack of this association can be partly explained by the nature of the “no CAD” group. They were individuals with multiple risk factors of CAD with subclinical and minimal coronary stenosis. Previous studies have shown an increased risk of OSA among these individuals in the absence of clinically significant CAD.21,22 Also, patients with acute coronary syndrome who tend to have higher prevalence of OSA (63–82%) were not included in this study, which may have contributed to the lower prevalence of OSA than previously reported.23 Another contributing factor may be related to the underpowered cross-sectional design of this study. Longitudinal studies on the impact of OSA on CAD have shown mixed results. OSA diagnosed early after revascularization was an independent predictor of adverse cardiac events after 2-years of follow-up.24 On the other hand, 1-year after adequate revascularization, the outcome of patients with acute coronary syndrome who had OSA was favorable and like those without OSA.25 Finally, a large longitudinal study followed adults with OSA who did not have CAD or heart failure for 7.7–9.3 years, and showed that only men aged ≤70 years had an adjusted increase in incident CAD.26
The increasing evidence of the association between OSA and increasing age, male gender, obesity, and hypertension may indicate that increasing numbers of undiagnosed OSA are to be expected among patients undergoing CATH.16 Indeed, our patients population were mostly older obese males. Implementing a screening protocol for OSA in patients planned for CATH may be a cost-effective way of identifying patients that should be referred for proper diagnosis using polysomnography. In one study, 70% of high risk patients were confirmed to have OSA by polysomnography.13 Even in the absence of a cardiovascular comorbidity, OSA is a disorder with associated increased morbidity and mortality and, hence, high-risk subjects should be referred for proper diagnosis before starting proper therapy.27
This study has some limitations that should be mentioned. The cross-sectional study design and convenience sampling may affect the external validity of the findings. Also, limiting the study to Jordan may create a threat to the generalizability of the results. Therefore, larger two-step studies (screening followed by polysomnography for the high risk group) may be needed.
Conclusion
Symptoms and risk of obstructive sleep apnea were common among adult Jordanians undergoing coronary catheterization. There was no association between the risk of obstructive sleep apnea and coronary artery disease. Larger studies are needed to assess the role of screening for obstructive sleep apnea in this patient population.
Disclosure
The authors report no conflicts of interest related to this work.
References
1. Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383:736–747. doi:10.1016/S0140-6736(13)61612-8
2. Khassawneh B, Ghazzawi M, Khader Y, et al. Symptoms and risk of obstructive sleep apnea in primary care patients in Jordan. Sleep Breath. 2009;13:227–232. doi:10.1007/s11325-008-0240-4
3. Lloyd-Jones D, Adams RJ, Brown TM, et al. Executive summary: heart disease and stroke statistics-2010 update: a report from the American Heart Association. American Heart Association Statistics committee and stroke statistics subcommittee. Circulation. 2010;121:948. doi:10.1161/CIRCULATIONAHA.109.192666
4. Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014;35::2950. doi:10.1093/eurheartj/ehu152
5. Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y. Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;169:207–214.
6. Dong JY, Zhang YH, Qin LQ. Obstructive sleep apnea and cardiovascular risk: meta-analysis of prospective cohort studies. Atherosclerosis. 2013;229:489–495.
7. Bhattacharyya N. Sleep and health implications of snoring: A populational analysis. Laryngoscope. 2015;125:2413–2416. doi:10.1002/lary.25346
8. Yeboah J, Redline S, Johnson C, et al. Association between sleep apnea, snoring, incident cardiovascular events and all-cause mortality in an adult population: MESA. Atherosclerosis. 2011;219:963–968. doi:10.1016/j.atherosclerosis.2011.08.021
9. Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi:10.1164/ajrccm.163.1.2001008
10. Gami AS, Pressman G, Caples SM, et al. Association of atrial fibrillation and obstructive sleep apnea. Circulation. 2004;110:364–367. doi:10.1161/01.CIR.0000136587.68725.8E
11. Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353:2034–2041. doi:10.1056/NEJMoa043104
12. De Torres-Alba F, Gemma D, Armada-Romero E, et al. Obstructive sleep apnea and coronary artery disease: from pathophysiology to clinical implications. Pulm Med. 2013;2013:768064. doi:10.1155/2013/768064
13. Wali SO, Alsharif MA, Albanji MH, et al. Prevalence of obstructive sleep apnea among patients with coronary artery disease in Saudi Arabia. J Saudi Heart Assoc. 2015;27:227–233. doi:10.1016/j.jsha.2015.03.004
14. Quan SF, Wright R, Baldwin CM, et al. Obstructive sleep apnea-hypopnea and neurocognitive functioning in the Sleep Heart Health Study. Sleep Med. 2006;7:498–507. doi:10.1016/j.sleep.2006.02.005
15. Young T, Blustein J, Finn L, Palta M. Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults. Sleep. 1997;20:608–613.
16. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–1239.
17. Saleh AB, Ahmad MA, Awadalla NJ. Development of Arabic version of Berlin questionnaire to identify obstructive sleep apnea at risk patients. Ann Thorac Med. 2011;6:212–216. doi:10.4103/1817-1737.84775
18. Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–491.
19. Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM. Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. Wmj. 2009;108:246–249.
20. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177:1006–1014. doi:10.1093/aje/kws342
21. Sorajja D, Gami AS, Somers VK, Behrenbeck TR, Garcia-Touchard A, Lopez-Jimenez F. Independent association between obstructive sleep apnea and subclinical coronary artery disease. Chest. 2008;133:927–933. doi:10.1378/chest.07-2544
22. Young T, Shahar E, Nieto FJ, et al.;
23. Leão S, Conde B, Fontes P, Calvo T, Afonso A, Moreira I. Effect of obstructive sleep apnea in acute coronary syndrome. Am J Cardiol. 2016;117:1084–1087. doi:10.1016/j.amjcard.2015.12.053
24. Loo G, Tan AY, Koo CY, Tai BC, Richards M, Lee CH. Prognostic implication of obstructive sleep apnea diagnosed by post-discharge sleep study in patients presenting with acute coronary syndrome. Sleep Med. 2014;15:631–636. doi:10.1016/j.sleep.2014.02.009
25. Zeng Y, Yang S, Wang X, Fan J, Nie S, Wei Y. Prognostic impact of residual SYNTAX score in patients with obstructive sleep apnea and acute coronary syndrome: a prospective cohort study. Respir Res. 2019;20:43. doi:10.1186/s12931-019-1030-1
26. Gottlieb DJ, Yenokyan G, Newman AB, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010;122:352–360. doi:10.1161/CIRCULATIONAHA.109.901801
27. Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American academy of sleep medicine clinical practice guideline. J Clin Sleep Med. 2017;13:479–504. doi:10.5664/jcsm.6506
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
