Back to Journals » International Journal of Women's Health » Volume 6
Satisfaction and health-related quality of life in women with heavy menstrual bleeding; results from a non-interventional trial of the levonorgestrel-releasing intrauterine system or conventional medical therapy
Authors Xu L, Lee BS, Asif S, Kraemer P, Inki P
Received 13 November 2013
Accepted for publication 25 December 2013
Published 27 May 2014 Volume 2014:6 Pages 547—554
DOI https://doi.org/10.2147/IJWH.S57470
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Ling Xu,1 Byung Seok Lee,2 Shaheena Asif,3 Peter Kraemer,4 Pirjo Inki5
1Department of Gynecology and Obstetrics, Peking Union Medical College Hospital, Beijing, People’s Republic of China; 2Department of Obstetrics and Gynecology, Yonsei University College of Medicine, Gangnam Severance Hospital, Seoul, Korea; 3Department of Gynaecology and Obstetrics, Surgimed Hospital, Lahore, Pakistan; 4Global Medical Affairs Excellence and Operations, 5Global Medical Affairs Women's Healthcare, Bayer HealthCare, Berlin, Germany
Purpose: To evaluate the patient satisfaction and health related quality of life (HRQoL) for levonorgestrel-releasing intrauterine system (LNG-IUS) versus conventional medical treatments ([CMTs] combined oral contraceptives, oral progestins, and antifibrinolytics, alone or in combination) in Asian women with heavy menstrual bleeding (HMB).
Patients and methods: A total of 647 patients diagnosed with HMB were recruited to this non-interventional study from the eight participating countries in Asia. Patient satisfaction was recorded at the last visit (at 12 months or premature discontinuation). At each visit (at 3, 6, and 12 months), patients completed the menorrhagia multi-attribute scale (MMAS) to assess HRQoL.
Results: A total of 83.5% of patients on the LNG-IUS were “very satisfied” or at least “satisfied” with the therapeutic effect of HMB treatment, compared with 59.2% of patients with CMTs (P<0.05). The mean (± standard deviation) MMAS score increased from 41.4±24.5 to 87.7±21.4 in the LNG-IUS arm, and from 44.1±24.9 to 73.1±25.3 in the CMTs arm. This increase was significantly higher in patients on the LNG-IUS, as compared with those on CMTs (P<0.05). The improvement in HRQoL in both treatment groups correlated with the body mass index of the patient, with larger improvement obtained in women with a higher body mass index.
Conclusion: The majority of women using the LNG-IUS or CMTs for HMB were satisfied with their treatment, and both treatment modalities were associated with significant improvements in HRQoL over time. The improvement was greater with the LNG-IUS, compared with CMTs.
Keywords: HRQoL, MMAS, menorrhagia, tranexamic acid, dysfunctional uterine bleeding
Introduction
Heavy menstrual bleeding (HMB) is defined as excessive menstrual blood loss, which may occur alone or in combination with other symptoms, and which has a negative impact on a woman’s physical, social, emotional, and/or material quality of life (QoL).1 The perceived impact of bleeding on health-related quality of life (HRQoL) is one of the basic reasons why a patient with HMB seeks medical help, even if the menstrual blood loss is below the stipulated cut-off value of 80 mL per cycle.1–3 Hence, the primary aim in any treatment for HMB should be improved HRQoL.2 Yet most studies on treatment of HMB in the literature focus on the reduction of menstrual blood loss rather than HRQoL.4–11 In addition, many of the currently available HRQoL measures such as the Short Form 36 are not specific for HMB.12
The levonorgestrel-releasing intrauterine system (LNG-IUS) has been shown to improve HRQoL to a similar extent to hysterectomy in a long-term randomized comparative study.13 Until recently, little data existed regarding the effect of commonly used therapies, such as oral contraceptives and tranexamic acid, on HRQoL of women suffering from HMB. Furthermore, these studies have generally been conducted in Europe or the US, and the data regarding Asian women’s experience of HMB is limited. In January 2013, the main results from the UK-based ECLIPSE trial (Effectiveness and cost-effectiveness of Levonorgestrel containing Intrauterine system in Primary care against Standard treatment for Menorrhagia) were published.14 This randomized comparative study of the LNG-IUS versus usual treatment used the validated HMB-specific QoL measure, the Menorrhagia Multi-Attribute Scale (MMAS),15 and showed that improvements in MMAS scores were significantly greater among women assigned to the LNG-IUS than among those assigned to usual treatment. As this study was conducted in the UK, it is not known whether the results can be extrapolated to the Asia-Pacific population. The Mirena or conventional medical treatment (MiCo) for HMB study (conventional medical treatment [CMT], combined oral contraceptives, oral progestins and antifibrinolytics, alone or in combination), a large non-interventional study in the Asia-Pacific region, was initiated to address these knowledge gaps. The results regarding the continuation rate and treatment efficacy of the MiCo study have been reported earlier by our group.16 The present study reports the patient satisfaction and HRQoL data from the MiCo study using the HMB-specific MMAS QoL measure.
Material and methods
Study design
This study design and methodology has been reported previously.16 In brief, this was a prospective observational cohort study with a non-interventional model. Informed consent was obtained from patients, and independent ethics committee or institutional review board approval was sought where necessary. The choice of treatment modality was not influenced by participation in the study and enrollment in the study did not warrant additional investigations. The study population was women between age 18 and 45 years who were not intending to become pregnant during the next year, with complaint of HMB over several consecutive cycles, without structural or histological abnormalities of the uterus, and who were eligible for pharmacological treatment. Patients who had contraindications and warnings regarding the study drugs; those on hormone therapy or with symptoms such as intermenstrual or postcoital bleeding (unless pathology was excluded via an endometrial biopsy); those with abdominally palpable fibroids, intracavitary fibroids, or a uterine length of more than 12 cm on ultrasound or hysteroscopy; and those on anticoagulants or other treatments known to cause menorrhagia (eg, copper intrauterine device) were excluded from the study. Investigators were asked to recruit consecutive patients from their routine clinical practice in the People’s Republic of China, Taiwan, Hong Kong, Indonesia, Malaysia, Pakistan, South Korea, and Thailand between September 2008 and December 2010. The primary outcome measure was the cumulative continuation rate at 12 months stratified by the history of previous treatment(s) for HMB. The secondary outcome parameters were bleeding pattern, patient satisfaction at end of documentation, HRQoL, and safety profile. Subject satisfaction was recorded using a four-point Likert-like scale (very satisfied to dissatisfied) at the last visit (at 12 months or at premature discontinuation). In cases where the patient had received previous HMB treatment, the investigators were requested to compare the previous treatment and actual treatment (LNG-IUS or CMTs), rating the experience as “much better,” “better,” “the same,” or “worse” based on retrospective recall.
Evaluation of HRQoL
At each visit, patients enrolled in the study were asked to complete the MMAS to assess the impact of therapy in terms of HRQoL.15 The MMAS questionnaire includes statements in six different domains; practical difficulties, impact on social life, psychological health, physical health, working life, and family life. Patients were asked to tick one statement in each of these domains. Each ticked statement corresponded to a score, and the addition of the six different scores provided the final MMAS score (0–100; 0= worst affected, 100= unaffected). It was mandatory to complete a questionnaire at both the initial visit and at least one follow-up visit, while it was voluntary on other visits. The mean MMAS score at baseline and the mean change over the course of the study was calculated. In addition, the results were stratified by treatment group, age group, body-mass-index (BMI) group, and country. The analyses used all available data. The mean change in MMAS score from baseline to the 12-month follow-up visit in both treatment groups (LNG-IUS or CMT) was evaluated using analysis of variance. Mean changes were also evaluated according to the BMI and age group.
Results
Patients
A total of 647 patients (LNG-IUS, n=483; CMTs, n=164) were recruited from the eight participating countries. Three countries (Pakistan, South Korea, and the People’s Republic of China) contributed approximately 80% of the recruited patients. All patients were included in the safety analysis (full analysis set), while the per-protocol sample of 572 patients (LNG-IUS, n=437; CMTs, n=135) were included in the efficacy analysis (Table 1). Because investigators recruited consecutive patients diagnosed with HMB to this non-interventional study, the number of subjects enrolled in each group could not be predetermined, thus resulting in an unequal size of the two treatment groups. The demographic and baseline characteristics, efficacy and safety results, as well as the study flow chart have been published previously.16 In brief, the mean (± standard deviation) age of the patients was 37.8±4.9 years, their mean BMI was 23.5±4.6, and 58% had not received previous treatment for HMB, while 36.2% had received at least one treatment and data were missing for 5.8%. In the conventional HMB therapy group (n=135), 75 patients (55.6%) received hormonal treatment, whereas 33 (24.4%) and 25 (18.5%) patients were on antifibrinolytic treatment or a combination of both hormonal and antifibrinolytic treatment, respectively.
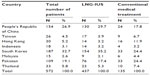  | Table 1 Patient disposition (per protocol population) |
Satisfaction with treatment
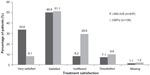
In the LNG-IUS group, over 80% of patients were “very satisfied” or “satisfied” with their therapy for HMB, compared with 59.2% of the patients using CMTs (Figure 1). The difference between treatment groups was statistically significant (two-sided Fisher’s exact test for satisfaction at last visit documented: P<0.05; logrank test for time-to-event: P<0.0001). In the CMTs group, there were no marked differences in the satisfaction rates within individual treatments (hormonal versus antifibrinolytic versus combined).
Previous HMB treatment, that was applied for at least 2 months, was recorded for 156/437 LNG-IUS patients (35.7%) and for 60/135 patients with CMTs (44.4%, not significant between treatment groups). Figure 2 displays the comparison of current therapy to previous therapy (women without previous therapy are included in the “missing” category). In the LNG-IUS group, more than one-third of the patients reported their current therapy as “much better” and more than 25% as “better” than previous therapy, while approximately 6% reported it to be “the same” and only 2% reported it as “worse”. In the CMTs group, <10% of patients on CMTs rated their current treatment to be “much better” than previous therapy, and approximately 30% reported their current treatment to have “better” efficacy than their previous treatment (Figure 2). The difference between groups was statistically significant (P<0.05, post-hoc Wilcoxon rank sum test).
Evaluation of HRQoL
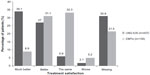
The majority of the patients (74.1% and 62.2% LNG-IUS and CMTs, respectively) completed the MMAS questionnaires at all four visits, while 15% of the overall population (14.9% and 15.6% LNG-IUS and CMTs, respectively) completed three questionnaires, 7.3% (5.9% and 11.9% LNG-IUS and CMTs, respectively) completed two questionnaires, and 3.0% (2.1% and 5.9% LNG-IUS and CMTs, respectively) completed only one questionnaire. No questionnaires were returned by 3.1% (18/572) women: 12 in the LNG-IUS and six in the CMTs group. The baseline mean (± standard deviation) MMAS score was 41.4±24.5 in the LNG-IUS arm and 44.1±24.9 in the CMTs arm. In both treatment groups, the MMAS score significantly increased over the study period (P<0.05). At 12 months, the mean increase in the MMAS score from baseline to 12 months was 51.1 in the LNG-IUS group and 29.9 in the CMTs group (Figure 3), and this difference was statistically significant (P<0.05).
The baseline scores of the patients in different BMI categories were fairly similar for both treatment groups, except that the score tended to be lower for patients with a BMI ≥30 kg/m2 compared with the other BMI groups (Figure 4). Both the treatment modality group (P<0.05) and the BMI group (P<0.05) had a significant effect on the change in the MMAS score from baseline to 12 months. The LNG-IUS was superior to CMTs and the greatest improvement was seen in those with a BMI ≥30 kg/m2 (Figure 4). With regard to the different age groups and treatment modalities, there was a significant change in the MMAS score from baseline to 12 months (P<0.05). There was an overall difference in the level of the MMAS score for the different age groups, but age group had no significant effect on the change in the MMAS score from baseline to 12 months (Figure 5).
Discussion
The present study describes real-life treatment patterns and satisfaction in a large group of women treated for HMB in the Asia-Pacific region. The results indicate that both the LNG-IUS and CMTs improve the QoL of women suffering from HMB. Compared with women using CMTs, women using the LNG-IUS for HMB have a higher satisfaction rate and increase in QoL as measured by the MMAS scores. The results on the LNG-IUS are in line with Western data on HRQoL, reported by the SF36-questionnaire, with the LNG-IUS therapy in HMB.17 The literature regarding QoL with CMTs is scarce, but the results from the ECLIPSE trial14 are in line with the results of the current study. Further stratification of the data based on the BMI shows that the heaviest women (BMI ≥30 kg/m2) derived the greatest benefit from both treatments. This is interesting, as obesity is considered to be a risk factor for HMB.
A systematic review published in 2002 on HRQoL instruments for HMB concluded that there is a need to develop methodologically sound disease-specific QoL instruments in HMB focusing both on face validity and measurement properties.18 Only two out of 19 studies used disease-specific QoL instruments, while the majority used the Short Form 36 Health Survey Questionnaire (SF36).18 However, several questions on the SF36 questionnaire have been shown to be inappropriate or difficult to answer for women with HMB as symptoms are not generally constant, but cyclical. Therefore, the authors concluded that, if used on its own, the SF36 is inappropriate as a patient-based outcome measure in HMB. Our study used the disease-specific MMAS score, which has been used in other HMB trials.
A recent review on the cost-effectiveness and QoL of the LNG-IUS in treatment of HMB found 16 studies reporting on the QoL after treatment with the LNG-IUS for HMB.19 Of note, none of these studies were performed in an Asian population. The authors concluded that, with a small number of exceptions, most HRQoL measurements improve with the LNG-IUS treatment, and that these improvements are, in most cases, at least similar to those achieved with hysterectomy or endometrial ablation.
The results in the current study on the improvement of HRQoL with LNG-IUS are in line with the published literature. The HRQoL data were available for the vast majority of subjects continuing treatment at any time point (see Results section); however, as the continuation rate was significantly lower with CMTs than with the LNG-IUS,16 the information was available for a lower proportion in the CMTs group. Although our study was not randomized, the results are remarkably similar compared with those recently reported in the ECLIPSE study.14 In the ECLIPSE study, greater improvements in MMAS were observed for the LNG-IUS from baseline to 6 months compared with usual treatment (P<0.001), and these improvements were maintained over a 2-year period (P<0.001). Improvements were noted across all the MMAS domains, including social life, family life, and work and daily routine. Importantly, after 2 years, more women continued using the LNS-IUS than their usual treatment (64 versus 38%; P<0.001).14 While the baseline MMAS scores were similar to those in our study (around 40 points), the magnitude of increase was somewhat lower in the ECLIPSE study, and the scores at 12 months were approximately 80 and 60 in the LNG-IUS group and the usual treatment groups, compared with 92.5 and 74 in the present study, respectively. This would indicate that the improvement of QoL achieved by treatment for HMB may be even greater in Asia-Pacific populations compared with the UK female population.
Obese women (BMI ≥30 kg/m2) tended to have a lower baseline QoL than women with a normal BMI or overweight women (BMI 25–29 kg/m2), both in our study and in the ECLIPSE study.14 In both studies, the greatest improvements in MMAS scores were obtained in obese women using the LNG-IUS.
In a prospective study of 56 morbidly obese women, the LNG-IUS was found to be an effective treatment in 75% of women.20 In our study, the HRQoL of obese women improved to an equal level to that of normal and overweight women after 12 months of follow-up with the LNG-IUS. Although, in women treated with CMTs, the improvement in the HRQoL score after 12 months also correlated with the BMI, it remained lower in the obese group as compared to the normal weight group. These results suggest that treatment with the LNG-IUS results in an equally high HRQoL status, regardless of BMI. In contrast, the final HRQoL may not be optimal in overweight and obese women treated with CMTs. This could be explained by the fact that the endometrial effects of the LNG-IUS are equally strong regardless of BMI, while the treatment effect may be less in overweight and obese women treated with CMTs as compared to lean and normal-weight women due to the higher distribution volume of the latter group. It can also be speculated that higher doses of CMTs (where feasible) should be used for overweight/obese women.
The major limitations of this study relate to its setting as an observational cohort study. Due to the nature of this setting, the two treatment cohorts can never be completely identical; however, with regard to the baseline characteristics, the two cohorts were very similar in this study. Nevertheless, our results were remarkably similar to those observed in the UK-based randomized ECLIPSE study; we therefore consider the results of our study representative of the improvement of HRQoL in Asia-Pacific women. The treatment satisfaction was recorded by the treating physician to the study documents; therefore, a “courtesy bias” is possible. Another limitation is that the MMAS questionnaire was not fully linguistically validated. However, the vast majority of women who continued treatment at any time point filled out the questionnaire, indicating that they did not have major problems in understanding the questionnaire. In addition, to the best knowledge of the authors, no local norm data exist for the participating countries for HRQoL by MMAS, therefore preventing any comparisons with previous data.
Conclusion
In conclusion, these study results indicate that HMB has significant negative impact on HRQoL in women from the Asia-Pacific region, echoing the experience from the European and North American studies. Patient satisfaction data in this study indicate that a significant proportion of women in the Asia-Pacific region do not attain optimal satisfaction with CMTs for HMB, and the LNG-IUS may offer considerable improvement in the overall treatment outcomes in these patients. While HRQoL improved in women treated both with CMTs and the LNG-IUS, the level of HRQoL that was reached with the LNG-IUS was higher compared to that reached with CMTs. After 12 months of follow-up, the HRQoL that was reached with the LNG-IUS was similar in women in all BMI categories, whereas the HRQoL that was reached with CMTs was lower in overweight and obese women, compared to normal-weight and lean women.
Acknowledgments
The present study was funded by an unrestricted educational grant from Bayer HealthCare Pharmaceuticals. The authors thank all investigators involved in the study for their valuable contribution.
Disclosure
PK and PI are employees of Bayer HealthCare Pharmaceuticals. The study was sponsored by Bayer HealthCare, which was also involved in protocol development. Data analysis was conducted by an external clinical research organization (Institute Dr Schauerte, Oberhaching, Germany). For this study, the English questionnaire was translated into the respective local language and then back-translated into English, wherever needed, according to standard local requirements. BSL, XL, and SA report no conflicts of interest in this work.
References
National Institute for Health and Clinical Excellence. Heavy Menstrual Bleeding. NICE Clinical Guideline 44. National Institute for Health and Clinical Excellence; 2007. Available from: http://www.nice.org.uk/nicemedia/pdf/CG44NICEGuideline.pdf. Accessed May 5, 2014. | |
Roy SN, Bhattacharya S. Benefits and risks of pharmacological agents used for the treatment of menorrhagia. Drug Saf. 2004;27:75–90. | |
Wyatt KM, Dimmock PW, Walker TJ, O’Brien PM. Determination of total menstrual blood loss. Fertil Steril. 2001;76:125–131. | |
Shaaban MM, Zakherah MS, El-Nashar SA, Sayed GH. Levonorgestrel-releasing intrauterine system compared to low dose combined oral contraceptive pills for idiopathic menorrhagia: a randomized clinical trial. Contraception. 2011;83:48–54. | |
Jensen J, Mansour D, Lukkari-Lax E, Inki P, Burock K, Fraser IS. Bleeding patterns with the levonorgestrel-releasing intrauterine system when used for heavy menstrual bleeding in women without structural pelvic pathology: a pooled analysis of randomized controlled studies. Contraception. 2013;87:107–112. | |
Leminen H, Hurskainen R. Tranexamic acid for the treatment of heavy menstrual bleeding: efficacy and safety. Int J Womens Health. 2012;4:413–421. | |
Fraser IS, Porte RJ, Kouides PA, Lukes AS. A benefit-risk review of systemic haemostatic agents: part 2: in excessive or heavy menstrual bleeding. Drug Saf. 2008;31:275–282. | |
Lethaby A, Irvine G, Cameron I. Cyclical progestogens for heavy menstrual bleeding. Cochrane Database Syst Rev. 2008;(1):CD001016. | |
Chelmow D. Levonorgestrel-releasing intrauterine system or medroxyprogesterone for heavy menstrual bleeding: a randomized controlled trial. Obstet Gynecol. 2010;116:1455–1456. | |
Micks E, Jensen JT. Estradiol valerate and dienogest: a novel four-phasic oral contraceptive pill effective for pregnancy prevention and treatment of heavy menstrual bleeding. Womens Health (Lond Engl). 2011;7:513–524. | |
Farquhar C, Brown J. Oral contraceptive pill for heavy menstrual bleeding. Cochrane Database Syst Rev. 2009;(4):CD000154. | |
Jenkinson C, Peto V, Coulter A. Making sense of ambiguity: evaluation in internal reliability and face validity of the SF 36 questionnaire in women presenting with menorrhagia. Qual Health Care. 1996;5:9–12. | |
Kaunitz AM, Inki P. The levonorgestrel-releasing intrauterine system in heavy menstrual bleeding: a benefit-risk review. Drugs. 2012;72:193–215. | |
Gupta J, Kai J, Middleton L, et al. Levonorgestrel intruterine system versus medical therapy for menorrhagia. N Eng J Med. 2013;368:128–137. | |
Shaw RW, Brickley MR, Evans L, Edwards MJ. Perceptions of women on the impact of menorrhagia on their health using multi-attribute utility assessment. Br J Obstet Gynaecol. 1998;105:1155–1159. | |
Lee BS, Ling X, Asif S, Kraemer P, Hanisch JU, Inki P. Levonorgestrel-releasing intrauterine system versus conventional medical therapy for heavy menstrual bleeding in the Asia-Pacific region. Int J Gynaecol Obstet. 2013;121:24–30. | |
Hurskainen R, Teperi J, Rissanen P, et al. Clinical outcomes and costs with the levonorgestrel-releasing intrauterine system or hysterectomy for treatment of menorrhagia: randomized trial 5-year follow-up. JAMA. 2004;291:1456–1463. | |
Clark TJ, Khan KS, Foon R, Pattison H, Bryan S, Gupta JK. Quality of life instruments in studies of menorrhagia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2002;104:96–104. | |
Blumenthal PD, Dawson L, Hurskainen R. Cost-effectiveness and quality of life associated with heavy menstrual bleeding among women using the levonorgestrel-releasing intrauterine system. Int J Gynaecol Obstet. 2011;112:171–178. | |
Vilos GA, Marks J, Tureanu V, Abu-Rafea B, Vilos AG. The levonorgestrel intrauterine system is an effective treatment in selected obese women with abnormal uterine bleeding. J Minim Invasive Gynecol. 2011;18:75–80. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.