Back to Journals » Journal of Pain Research » Volume 15
Salvage of Failed Lateral Sacroiliac Joint Fusion with a Novel Posterior Sacroiliac Fusion Device: Diagnostic Approach, Surgical Technique, and Multicenter Case Series
Authors Sayed D , Khatri N , Rupp A , Bovinet C, Azeem N, Li S , Josephson Y, Pope J
Received 5 January 2022
Accepted for publication 6 May 2022
Published 12 May 2022 Volume 2022:15 Pages 1411—1420
DOI https://doi.org/10.2147/JPR.S357076
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Erika Petersen
Dawood Sayed,1 Nasir Khatri,1 Adam Rupp,1 Christopher Bovinet,2 Nomen Azeem,3 Sean Li,4 Youssef Josephson,5 Jason Pope6
1Department of Anesthesiology, University of Kansas, Kansas City, KS, USA; 2The Spine Center of Southeast Georgia, Brunswick, GA, USA; 3Florida Spine & Pain Specialists, Riverview, FL, USA; 4Premier Pain Centers, Shrewsbury, NJ, USA; 5National Spine & Pain Centers, Voorhees Township, NJ, USA; 6Evolve Restorative Center, Santa Rosa, CA, USA
Correspondence: Dawood Sayed, Department of Anesthesiology, University of Kansas, Kansas City, KS, USA, Email [email protected]
Background: Studies have found that up to one-third of patients with LBP have sacroiliac joint (SIJ) dysfunction as a contributing cause. Historically, the management of SIJ dysfunction has been plagued by ineffectiveness or significant morbidity. In 2008, minimally invasive lateral SIJ fusion was developed. While this procedure is a safe and effective treatment, there is still a significant proportion of patients who will not experience therapeutic success. There is a paucity of data in the literature regarding the management of these patients. Recently, a novel posterior sacroiliac joint fusion device has been developed which minimizes complications compared to lateral approaches and may serve to salvage therapeutic failures in this patient population.
Objective: Determine the efficacy and feasibility of a posterior SIJ fusion device as a salvage technique in patients who have not experienced therapeutic success following lateral SIJ fusion.
Design: Multi-center retrospective observational study.
Methods: Patients who had previously undergone lateral SIJ fusion and had persistent LBP were evaluated and diagnosed to have persistent primary SIJ pathology. All patients underwent posterior SIJ fusion utilizing a machined allograft transfixing sacroiliac fusion device. Demographic data and patient reported pain scores were collected.
Results: A total of 7 patients who had undergone lateral SIJ fusion were included in the study and underwent posterior SIJ fusion. The mean patient reported pain improvement following posterior fusion was 80% with an average follow-up time of 10 months. Median morphine milliequivalents were 20 pre-procedure and 0 post-procedure.
Conclusion: We were able to show significant reductions in pain scores and opioid consumption, which suggests that minimally invasive posterior SIJ utilizing a novel implant and technique may be a viable treatment option to salvage pain relief in this patient population. Further, the favorable safety profile of this posterior technique uniquely positions it to be an appropriate first-line surgical therapy.
Keywords: sacroiliac joint pain, posterior SIJ fusion, lateral SIJ fusion, salvage, low back pain
Introduction
Background
Low back pain is one of the world’s largest contributors to healthcare spending.1–3 Of patients with chronic low back pain, it has been estimated that up to one-third may have concomitant sacroiliac joint pathology contributing to the pain.1–3 This proportion may be even higher given the difficulty in diagnosing a primary etiology of chronic low back pain due to concurrent painful spinal pathologies with overlapping symptoms.4 While the use of history and physical examination are key to the accurate diagnosis of sacroiliac joint dysfunction, studies have found that provocative maneuvers such as Fortin’s, FABER (Flexion, Abduction and External Rotation), or Patrick’s Test, Gaenslen’s, thigh thrust, and Lateral Compression Test, among others, improve the specificity and accuracy of the diagnosis.2,5 The gold standard for diagnosis, however, is fluoroscopically guided intraarticular diagnostic block.5
Once the diagnosis has been established, traditional management of SIJ pain first starts with conservative management.2,6 Patients who have failed interventional therapies, such as SIJ steroid injections and lateral branch ablation, are typically referred for consideration of surgery. Historically, sacroiliac fusion was performed via an open approaches with variable outcomes.6 Over the past decade the minimally invasive lateral fusion has become increasingly more popular focusing on improved VAS and ODI scores, reduced operative times, blood loss, complications and shorter hospital stays.1,2,7 Lateral fusion is performed using the transiliac approach by placing 1–3 implants across the joint to fix the sacroiliac joint for long-term arthrodesis.7,8
Biomechanics
The SI complex is a diarthrodial joint that functions primarily for stability.9 The joint works simultaneously on three axes to allow flexion/extension, rotation and translation. However, there are minimal degrees or sub-millimeter movements throughout the joint.9 This small motion in multiple planes allows for a large transfer of energy from the lumbar spine to the lower extremities. When working properly, the SIJ is a very effective “hub” allowing for smooth ambulation as well as load distribution from the trunk.10 However, any disruptions into the system can lead to force imbalances, malalignment and pain. There are many causes of disruption to the SIJ including infection, arthritis, fracture and stabilizing ligamentous injury. There are also factors that increase the risk of SIJ pathologies such as scoliosis, prior lumbar-sacrum fusion, leg length discrepancies, spinal stenosis, and hip pathologies.2
In 2021, Sayed et al published data on the biomechanical effects of a novel posterior sacroiliac approach.11 In a cadaveric study evaluating six SI joint specimens, the effects of a posterior SIJ fixation utilizing a novel cortical allograft were studied. They found that unilateral and bilateral fixations generated sacroiliac joint ROM reductions in flexion-extension, lateral bending, and axial rotation. Further, it was noted that posterior fixation of the SIJ shifted the instantaneous axis of rotation of the joint to the graft implantation site, underscoring the importance of graft placement. In all, the findings from this study suggest that posterior SIJ fusion stabilizes the joint both by reducing the total ROM of the joint as well as by shifting the axis of rotation. By doing so, the novel cortical allograft allows for minimal motion at the implantation site, which promotes fusion in the region.11
Lateral Fusion Data
While the minimally invasive lateral approach to sacroiliac joint fusion has a remarkably improved safety profile as compared to the open approach first described in 1921, there is still an up to 16.4% risk of adverse events.1 In a systematic review by Shamrock et al evaluating fourteen studies, there was found to be a 2% incidence of wound infection and 1.6% incidence of nerve root impingement.12 Furthermore, weight-bearing restrictions for up to six weeks post-operatively could lead to increased morbidity. As such, there has been motivation to develop a novel therapeutic approach to treat sacroiliac joint dysfunction with an even lower risk profile.
Evidence for the lateral approach has mostly been positive for improving low back pain with the lateral SIJ fusion technique having two large prospective randomized controlled trials. In a prospective, randomized control trial conducted by Polly et al, 148 patients were randomly assigned to either minimally invasive SIJ fusion or conservative management.13 The surgical arm reported an improvement of 55.4 points on a 100-point VAS scale, as compared to a 12.2-point improvement in the conservative treatment arm. 68% of patients had an improvement in ODI greater than 15 points at 24 months, as compared to 7.5% in the conservative arm.13 Similarly, Dengler et al found both a statistically and clinically significant difference in pain, disability, and quality of life as compared to conservative management.14
However, despite the positive evidence in support of lateral SIJ fusion, there is sufficient data in the literature to conclude that a subset of patients have refractory pain despite appropriate diagnosis and treatment with this therapy. A prospective, randomized control trial by Smith et al evaluating 141 subjects who underwent lateral SIJ fusion found that 30% of patients did not meet the minimum clinically importance difference (MCID) for VAS change (>20 points) between 6 and 24 months follow-up.8 Similarly, a prospective single-arm study evaluating 172 patients who underwent lateral SIJ fusion found that 16% of patients failed to meet VAS MCID at 6–24 months follow-up.12 Further, the MCID for ODI (>15 points) was not met in either trial in 27% and 34% of patients, respectively.8,12 This data reveals that while minimally invasive lateral SIJ fusion is a more efficacious and safe procedure as compared to the open approach, roughly one-third of patients undergoing lateral fusion will not have clinically satisfactory outcomes.
Emergence of Posterior Technique and Evidence
Recent advances in surgical techniques to treat sacroiliac joint pathologies have resulted in the development of novel posterior and posterior oblique approaches.2 For the purposes of this discussion, we will be discussing a single-point posterior implantation technique utilizing a novel allograft.
Whereas the literature currently supports the use of the well-established lateral approach, there is a growing body of evidence supporting the efficacy and safety of the posterior approach. Pyles et al presented the earliest data on the efficacy of a single ridged cortical allograft in a 7 patient case series. They found an average NRS reduction of 6.5 with a 94.2% pain reduction at up to 5 months post-op.15 Lam et al presented a retrospective chart review of 62 patients across several institutions and reported an average of 83.3% pain relief at 3-months, along with a significant number of patients reporting a decrease in opioid use as well.16 Interestingly, in both studies, no device-related adverse events were reported and the same posterior approach was utilized.
More recently, Sayed et al published a retrospective analysis of 110 patients across multiple institutions and reported outcomes on long-term follow-up.3 The average NRS was 6.98 pre-fusion and 3.06 at last follow-up, which was on average 612 days from the date of implant. Patients with a history of prior lumbar fusion had an even higher percentage of pain relief in NRS scores.3
Deer et al published a case series on the utilization of posterior SIJ fusion as a salvage technique in patients who had previously undergone advanced interventional pain therapies.17 A total of 111 patients with history and physical exam consistent with SIJ pathology who had previously undergone spinal cord stimulation, interspinous spacer, intrathecal drug delivery, or minimally invasive lumbar decompression and had persistent LBP were studied. The mean patient reported pain relief following SI joint fusion was 67.5% following implant at last follow-up, which was on average 290 days from the date of implant for the index area of pain. In patients with a diagnosis of failed back surgery syndrome, the pain relief was even more significant. This subset of patients reported 76.5% pain relief with an average follow-up duration of 394.4 days.17 There were no device related major adverse events or complications in either study.
These studies highlight the emerging evidence supporting the safety and long-term efficacy of posterior SIJ fusion. However, given that lateral SIJ fusion remains the primary surgical technique utilized for SIJ dysfunction, further evidence comparing the two techniques head-to-head are warranted. The favorable safety profile of the posterior technique uniquely positions it to be an appropriate first-line surgical therapy. Further, this case series will describe the utility of posterior SIJ fusion as a salvaging technique in patients who previously underwent lateral SIJ fusion with lack of pain relief.
Diagnostic Algorithm
Currently, there is not a well-established clinical diagnostic approach for patients with persistent pain after previous lateral sacroiliac fusion. The authors of this manuscript utilized a combination of history, physical exam findings, radiographic studies, and response to local anesthetic injection into the sacroiliac joint. It should be noted that because patients have received previous sacroiliac fusion, physical exam maneuvers for sacroiliac dysfunction can be difficult to assess. The authors felt that significant pain relief following a diagnostic sacroiliac joint injection was the most helpful indicator that the sacroiliac joint was still the major source of pain. Radiographic imaging, especially CT scan, was also considered helpful if lucency around the implant or lack of bony bridging was observed [Table 1].
 |
Table 1 Proposed Prognostic Indicators for SI Joint as Primary Source of Pain in Patients with Previous Lateral Fusion |
Methods
Study Design
This study was a retrospective review of 7 patients across 5 different centers in the United States. The aim was to establish the feasibility and efficacy of a novel posterior SIJ fusion device, specifically LinqTM (PainTeq, Tampa, FL, USA) in patients who have failed to have pain improvement after minimally invasive lateral SIJ fusion. An IRB waiver was granted by WIRB-Copernicus Group, Inc. Institutional Review Board to the primary investigator who provided oversight of this study. (IRB # 1-1500728-1) All collected patient data was de-identified and kept confidential in compliance with the Declaration of Helsinki. Data acquisition was in accordance with the legal guidelines set forth by the locality of each pain management center.
Data Collection
Demographic data as well as numeric rating scale (NRS) pain scores were extracted from the electronic medical record (EMR) for each subject enrolled into the study. Baseline pain scores were obtained at the pre-operative clinic visit, following lateral SIJ fusion and prior to posterior SIJ fusion salvage therapy. Post-operative pain score was obtained at the last follow-up. The time between the two procedures, morphine milliequivalents (MME) prior to and after posterior SIJ fusion and whether a diagnostic SIJ injection was performed, were also extracted from the EMR. All data was entered in a de-identified fashion into a secure database, which was created and maintained by the corresponding author. The study included a total of 6 patients who met inclusion criteria. All patients were at least 6 months post-operation from lateral SIJ fusion at the time of salvage therapy.
Inclusion Criteria
Subjects included in this study had previously undergone minimally invasive lateral SIJ fusion with persistent ipsilateral SIJ pain for a minimum of 6 months post-operation. Subjects met all pre-implantation evaluation criteria required for posterior SIJ fusion. This includes non-radicular low back pain primarily below the belt line, at least 3 out of 5 provocative exam maneuvers for SIJ dysfunction (distraction, thigh thrust, Patrick’s maneuver, lateral compression, and Ganslen’s), and >50% reduction in pain after diagnostic SIJ injection with local anesthetic.
Statistical Analysis
A univariate statistical analysis was performed to report the outcomes. Results are reported for each individual patient. Continuous outcomes were reported as mean as well as a range and categorical outcomes as frequency (%). Patient reported pain scores and opioid consumption following posterior SIJ fusion were compared to baseline, which was defined as at the last clinic visit prior to posterior SIJ fusion.
Surgical Technique for Posterior SIJ Fusion in Patients with Previous Lateral Sacroiliac Fusion
Posterior SIJ fusion is a fluoroscopically guided surgical procedure.2 The patient is brought into the operating room and placed in the prone position on a radiolucent flat top or Jackson table Chest rolls and table flexion are utilized to allow the hips 20 degrees of flexion, which levels off the pelvis on fluoroscopy. An oblique tilt of the c-arm is utilized to superimpose the posterior and anterior sacroiliac joint lines. After obtaining the proper starting image, a Steinman pin is placed into the sacroiliac joint. Ideally, placement of the Steinman pin will occur in the middle one-third of the sacroiliac joint. This is confirmed with lateral fluoroscopic images. In the case of previous lateral instrumentation, variations in craniocaudal tilt with the fluoroscope may need to be obtained to obtain a clear view of the sacroiliac joint.
Following appropriate placement of the Steinman pin, a two-part dilator and working cannula is advanced over the pin until it is seated into the joint [Figure 1]. The implanting physician should obtain multiple views of the open working cannula to ensure that it is appropriately positioned within the sacroiliac joint. In this case series, the physicians then utilized a drill-less box-cutter to decorticate the joint space to prepare the sacrum and ilium for implantation of the implant for arthrodesis. Care must be taken during decortication as advancing too far anterior may damage previously placed lateral implants. As such, final placement of the posterior implant should be posterior to the most dorsal lateral implant [Figure 2]. In a modification to the technique for a typical posterior fusion, the implanting physicians recommend a final implant position posterior to where implantation would occur without previous lateral sacroiliac instrumentation. Prior to placement of the implant, suction tubing can be inserted through the guide retraction tube to clear the tube of blood that has accumulated after decortication. Finally, demineralized bone matrix (DBM) and the novel cortical allograft are placed across the sacroiliac joint using an inserter [Figure 2]. Following this, all the instruments are removed, leaving only the allograft implanted into the joint [Figure 3].2
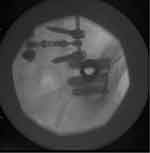 |
Figure 1 Anteroposterior “down the barrel” fluoroscopic view of the guide retraction tube within the sacroiliac joint in a patient with three lateral triangular titanium implants. |
 |
Figure 2 Lateral image depicting the implant being inserted into the sacroiliac joint in a patient with three lateral triangular titanium implants. |
 |
Figure 3 Lateral (A) image of Linq implant seated within the sacroiliac joint posterior to the three lateral triangular titanium implants. |
From an anesthetic perspective, the procedure is most commonly performed under monitored anesthesia care (MAC), however general anesthesia or local anesthetic only are also viable anesthetic options.
Results
A total of 7 patients were included in this retrospective review. Baseline demographic and clinical data are shown in Table 2. The mean age was 66.5 with a range from 50 to 81. 4 patients were female and 3 were male. The mean BMI was 29 with a range from 21 to 36. All of the patients had right sided pain. 100% of patients had a positive result from a diagnostic SIJ injection on the affected side. The average duration of time in months between lateral SIJ fusion and salvage with posterior SIJ fusion was 19.7 but ranged from 6 to 26.
 |
Table 2 Baseline Clinical and Demographic Variables of Included Patients |
Utilizing a univariate statistical analysis, the mean pre-procedure patient reported pain score prior to salvage with posterior SIJ fusion was 8. At the last follow-up, the mean post-procedure patient reported pain score was 2. This represents an 80% reduction in pain score, a clinically significant reduction. The median MME for patients in this study was 20. Following posterior SIJ fusion, the median MME was zero. Three of the patients who were previously on chronic opioids were able to completely wean off and two had a greater than 50% reduction in their opioid usage. The average follow-up period in months was 10 but ranged from 3 to 16 [Table 3].
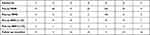 |
Table 3 Clinical Outcomes Following Salvage with Posterior SIJ Fusion |
During the pre-operative work-up of one patient (Patient ID 4) who had persistent SIJ pain despite having undergone minimally invasive lateral SIJ fusion, a lumbar CT scan was obtained and showed no evidence of osseous fusion [Figure 4]. However, a follow-up lumbar CT scan after salvage with a posterior SIJ fusion device found evidence of osseous fusion [Figure 5]. This finding was documented by the radiologist on the report of both studies.
 |
Figure 4 Lumbar CT scan depicting no osseous fusion or bridging of the right SI joint. Accompanying radiology report noting the same. |
 |
Figure 5 Lumbar CT scan depicting radiographic evidence of bony bridging and partial fusion of the right SI joint. Accompanying radiology report noting the same. |
Discussion
Given the significant burden of sacroiliac joint dysfunction in society and the healthcare system, there has been an ongoing effort to develop effective therapies with the least amount of morbidity possible. While the minimally invasive lateral SIJ fusion is a far less morbid and safe procedure as compared to the open approach, there is sufficient data in the literature to suggest that complications are not uncommon and that there is a relatively high non-responder rate. This is particularly difficult to reconcile, given the cost and invasiveness of the procedure, risks associated with it, and recovery time for patients.
While a relatively new therapy, there is emerging evidence in the literature supporting the safety and long-term efficacy of posterior SIJ fusion. However, the evidence to date has been in patients who have not previously undergone sacroiliac joint fusion of any type. Our results describe the first published case series demonstrating the feasibility and efficacy of a novel posterior SIJ fusion technique as a salvage therapy for patients who have not had therapeutic success with the lateral SIJ fusion. Further, this data not only notes the improvement in NRS pain scores but also a significant reduction in opioid consumption. As there is a continued worldwide emphasis on opioid-sparing pain therapies, this is a vital consideration of this surgical therapy for SIJ dysfunction. It is also particularly interesting to note that Patient 4 in the case series had an initial CT scan with no radiographic evidence of bony fusion within the SIJ following minimally invasive lateral fusion. However, following posterior SIJ fusion, an updated CT scan found evidence of bony fusion within the joint. This is the first published description of such a finding on radiographic imaging, and further supports the utility of posterior SIJ fusion as a salvage technique in this patient population. Also, worth discussion is both the immediate stabilization via distraction as well as long-term relief via arthrodesis utilizing this posterior technique. These dual mechanisms are supported in this case series demonstrated by significant improvement in pain by patients at both short- and long-term follow-up. The authors conclude these findings as noteworthy as most patients are treated with lateral sacroiliac fusion as “last resort” without any other treatment available if they do not experience therapeutic success. This manuscript describes a viable treatment option for the many patients seeking further treatment options who continue to suffer from pain and dysfunction after lateral sacroiliac fusion.
The authors note certain technical aspects and pearls of performing posterior sacroiliac fusion in patients with previous lateral instrumentation. Preoperative review of CT or MRI is critical to ensure proper trajectory and implant depth intraoperatively. Additionally, multiple views of the access cannula utilizing cranial and caudal tilts can be very helpful as the normal sacroiliac anatomy can be obscured by previous lateral instrumentation. The implanting physicians also recommend a more posterior final implant position of the transfixing posterior implant then what is typical of posterior implantation to avoid damage or fracture of the previously implanted lateral instrumentation. The authors also find it noteworthy that this case series validates a surgical technique that can be performed minimally invasively without removal or revision of the previously implanted hardware.
Despite a wide range in follow-up period, we saw significant improvement in patient reported pain scores as well as opioid use at all follow-up levels. As has previously been described, bony fusion of the SIJ with this novel cortical allograft can take several months. However, patients reported improvement in pain shortly after cortical allograft implantation. We suspect that this phenomenon is due to distraction and immediate fixation of the SIJ, which has been proven in a previous biomechanical study of this particular implant. This is also consistent with the clinical literature that has previously been published with this approach.
Additionally, posterior and posterolateral SIJ fusion techniques frequently lend themselves to critique by proponents of the lateral technique. There is a misconception that the posterior fusion is not actually fixating the joint or that it is not a true arthrodesis. This case series illustrates that by placing a cortical transfixing machined allograft and demineralized bone matrix (DBM) within the sacroiliac joint, the joint is both distracted and bony fusion occurs. This is further evidenced by Figure 4. We also present radiographic evidence in Figure 3 that lateral SIJ fusion does not necessarily always result in bony fusion, and that the lack of fusion may in part contribute to a lack of therapeutic success, though more research is needed on this.
Limitations
Conclusions from our case series are limited by the low number of patients, the retrospective nature of this study, a relatively short follow-up time for some patients, and the lack of a control group. However, given that lateral SIJ fusion remains the primary surgical technique utilized for SIJ dysfunction, the results of this study emphasize the need to develop more prospective data so that the various techniques for stabilizing the sacroiliac joint can be better evaluated. Further, our case series did not include health-related quality of life outcomes and Oswestry Disability Index scores, which are important outcomes to consider for all pain therapies and should be assessed in future studies.
Conclusion
This is the first manuscript evaluating the feasibility of utilizing a posterior SIJ fusion device in patients who have failed lateral SIJ fusion. While there are limitations to this case series, these results suggest that posterior SIJ fusion is an effective treatment option in the management of this patient population. The favorable safety profile of the posterior technique uniquely positions it to be an appropriate first-line surgical therapy. Future research should focus on comparing the safety and efficacy of minimally invasive lateral and posterior SIJ fusion.
Disclosure
Dr Dawood Sayed reports personal fees from PainTeq, outside the submitted work. Dr Christopher Bovinet reports personal fees from PainTEQ, outside the submitted work. Dr Nomen Azeem reports personal fees from Painteq, LLC, outside the submitted work. Dr Sean Li is a consultant for Abbott, reports grants from Boston Scientific, grants, received research grant from Averitas Pharma, grants from SGX Medical, received research grant from Saluda Medical, received research grant from Nalu, received research grant from Nevro, received research grant from SPR Therapeutics, received research grant from Avanos, received research grant from PainTeq, is speaker bureau for Scilex Pharma, received research grant from Biotronik, is a consultant for Vertos, outside the submitted work. Dr Jason Pope reports has stock option and a consultant for Painteq, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Lee DW, Patterson DG, Sayed D. Review of current evidence for minimally invasive posterior sacroiliac joint fusion. Int J Spine Surg. 2021;15(3):514–524. doi:10.14444/8073
2. Falowski S, Sayed D, Pope J, et al. A review and algorithm in the diagnosis and treatment of sacroiliac joint pain. J Pain Res. 2020;13:3337–3348. doi:10.2147/JPR.S279390
3. Sayed D, Balter K, Pyles S, Lam CM. A multicenter retrospective analysis of the long-term efficacy and safety of a novel posterior sacroiliac fusion device. J Pain Res. 2021;14:3251–3258. doi:10.2147/JPR.S326827
4. Hansen HC, McKenzie-Brown AM, Cohen SP, Swicegood JR, Colson JD, Manchikanti L. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007;10(1):165–184. doi:10.36076/ppj.2007/10/165
5. van der Wurff P, Hagmeijer RH, Meyne W. Clinical tests of the sacroiliac joint. A systematic methodological review. Part 1: reliability. Man Ther. 2000;5(1):30–36. doi:10.1054/math.1999.0228
6. Rashbaum RF, Ohnmeiss DD, Lindley EM, Kitchel SH, Patel VV. Sacroiliac Joint Pain and Its Treatment. Clin Spine Surg. 2016;29(2):42–48. doi:10.1097/BSD.0000000000000359
7. Kaye AD, Edinoff AN, Scoon L, et al. Novel interventional techniques for chronic pain with minimally invasive arthrodesis of the sacroiliac joint: (INSITE, iFuse, Tricor, Rialto, and others). Rheumatol Ther. 2021;8(3):1061–1072. doi:10.1007/s40744-021-00350-8
8. Smith AG, Capobianco R, Cher D, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res. 2013;7(1):14. doi:10.1186/1750-1164-7-14
9. Harrison DE, Harrison DD, Troyanovich SJ. The sacroiliac joint: a review of anatomy and biomechanics with clinical implications. J Manipulative Physiol Ther. 1997;20(9):607–617.
10. Kiapour A, Joukar A, Elgafy H, Erbulut DU, Agarwal AK, Goel VK. Biomechanics of the sacroiliac joint: anatomy, function, biomechanics, sexual dimorphism, and causes of pain. Int J Spine Surg. 2020;14(Suppl 1):3–13. doi:10.14444/6077
11. Sayed D, Amirdelfan K, Naidu RK, Raji OR, Falowski S. A cadaver-based biomechanical evaluation of a novel posterior approach to sacroiliac joint fusion: analysis of the fixation and center of the instantaneous axis of rotation. Med Devices. 2021;14:435–444. doi:10.2147/MDER.S347763
12. Shamrock AG, Patel A, Alam M, Shamrock KH, Al Maaieh M. The safety profile of percutaneous minimally invasive sacroiliac joint fusion. Global Spine J. 2019;9(8):874–880. doi:10.1177/2192568218816981
13. Polly DW, Swofford J, Whang PG, et al. Two-year outcomes from a randomized controlled trial of minimally invasive sacroiliac joint fusion vs. non-surgical management for sacroiliac joint dysfunction. Int J Spine Surg. 2016;10:28. doi:10.14444/3028
14. Dengler J, Kools D, Pflugmacher R, et al. Randomized trial of sacroiliac joint arthrodesis compared with conservative management for chronic low back pain attributed to the sacroiliac joint. J Bone Joint Surg. 2019;101(5):400–411. doi:10.2106/JBJS.18.00022
15. Pyles S, Ortiz A, Lam C, et al. LINQ SI Fusion for pain relief in SCS patient: a case series.
16. Lam CM, Pyles S, Balter K, Sayed D. Multi-center outcomes in minimally invasive sacroiliac fusion.
17. Deer TR, Rupp A, Budwany R, et al. Pain relief salvage with a novel minimally invasive posterior sacroiliac joint fusion device in patients with previously implanted pain devices and therapies. J Pain Res. 2021;14:2709–2715. doi:10.2147/JPR.S325059
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
