Back to Journals » Medical Devices: Evidence and Research » Volume 13
Safety and Efficacy of an Oxytocin Gel and an Equivalent Gel but Without Hormonal Ingredients (Vagivital® Gel) in Postmenopausal Women with Symptoms of Vulvovaginal Atrophy: A Randomized, Double-Blind Controlled Study
Authors Fianu Jonasson A, Bixo M, Sundström Poromaa I, Åstrom M
Received 22 July 2020
Accepted for publication 17 September 2020
Published 5 October 2020 Volume 2020:13 Pages 339—347
DOI https://doi.org/10.2147/MDER.S265824
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Aino Fianu Jonasson,1 Marie Bixo,2 Inger Sundström Poromaa,3 Mikael Åstrom4
1Department of Clinical Sciences, Intervention and Technology, Division of Obstetrics and Gynecology, Karolinska Institute, Stockholm, Sweden; 2Department of Clinical Sciences, Obstetrics and Gynecology, Umea University, Umea, Sweden; 3Research Group; Reproductive Health, Department of Women’s and Children’s Health, Uppsala University, Uppsala, Sweden; 4StatCons, Malmo, Sweden
Correspondence: Aino Fianu Jonasson
Department of Clinical Science, Intervention and Technology, Division of Obstetrics and Gynecology, Karolinska Institute, Stockholm 171 77, Sweden
Tel +4670 483 60 28
Fax +4608 31 11 01
Email [email protected]
Purpose: The primary objective was to compare the efficacy of 12 weeks of daily treatment with Aqueous Hypromellose-based vaginal (Vagivital®) gel versus Aqueous Hypromellose-based vaginal gel plus 400 IU oxytocin gel in reducing the severity of the most bothersome vulvovaginal atrophy symptoms (MBS: itching, dysuria, bleeding, and pain/discomfort during vaginal sexual activity) observed at baseline. The secondary objectives were to evaluate the other vulvovaginal atrophy symptoms, vaginal pH, superficial squamous cells, and the safety and tolerability of both gels.
Patients and Methods: This double-blind, randomized study evaluated the safety and efficacy of subjects randomly assigned to 12 weeks of daily intravaginal oxytocin gel (n=79) or Aqueous Hypromellose-based vaginal gel (n=78). The efficacy evaluation was performed using data from all included subjects who fulfilled entry criteria.
Results: Both treatments induced statistically significant reductions in the severity of the MBS from baseline until 4 weeks (Vagivital mean reduction 0.90, p=0.0000; Oxytocin mean reduction 0.82, p=0.0000) and 12 weeks post baseline (Vagivital mean reduction 1.28, p=0.0000; Oxytocin mean reduction 1.16, p=0.0000), but the reduction of MBS severity was not significantly different between the treatment groups at either time point. No serious adverse events were reported in the Aqueous Hypromellose-based vaginal gel group during the treatment period, but one (breast cancer) was reported in the oxytocin gel group (assessed as unlikely related to the study compound).
Conclusion: Significant reductions in the severity of the MBS were seen in both the Aqueous Hypromellose-based vaginal gel and the oxytocin gel groups, but with no significant differences in severity reduction seen between the groups. Both gels were safe and well tolerated. Given the benefits of avoiding the use of hormones, Aqueous Hypromellose-based vaginal gel is an attractive first choice in the treatment of postmenopausal women with vulvovaginal atrophy symptoms.
Keywords: most bothersome vulvovaginal atrophy symptoms, MBS, non-hormonal therapy, dyspareunia, vaginal dryness
Introduction
Up to 50% of postmenopausal women frequently suffer from atrophic vaginitis or vulvovaginal atrophy (VVA). The most bothersome symptoms (MBS) of VVA include itching, dysuria, bleeding, and vaginal dryness/discomfort, which can make intercourse difficult or painful.1 Vulvovaginal atrophy is a consequence of the lining tissue of the vagina becoming thinner, drier, and less elastic due to the reduced production of estrogen associated with menopause.2 In addition, VVA is associated with an increased vaginal pH which creates an environment more susceptible to infection.3,4 The mucosal squamous epithelium shows signs of severe senile atrophy and cytological examination demonstrates increased number of basal and parabasal cells along with reduced number of superficial cells.5 Unlike some other menopausal symptoms, such as hot flushes, vaginal symptoms generally persist or worsen with age.6
Local intravaginal administration of estrogen is the first-line treatment in women experiencing symptoms of VVA.7–9 Due to the lack of evidence on long-term safety, systemic absorption of vaginal estrogen is still a safety concern and may be a basis for a contradiction for the use of intravaginal estrogen for some women (such as breast cancer survivors). Oxytocin is a pituitary hormone that induces mitosis and stimulates cell proliferation.10,11 One study found that oxytocin had significantly positive histological and cytological effects, but no significant effect upon VVA reduction in postmenopausal women,12 while two studies with small populations have shown that oxytocin reduces VVA in post-menopausal woman.13,14 Oxytocin lowers blood pressure and lowers heart rate, but raises gastrointestinal and pancreatic activity (thus influencing insulin secretion).11 A review of clinical trials of the effect of oxytocin on VVA in postmenopausal women reported that no particular short-term side effects were observed, but noted that further studies must be conducted to determine the possible long-term effects of oxytocin.15 For women who want to avoid the potential long-term adverse effects of hormones such as estrogen and oxytocin, local non-hormonal treatments for vaginal atrophy, such as Aqueous Hypromellose-based vaginal (Vagivital®) gel or other vaginal moisturizers, are typically employed.16,17 Vaginal moisturizers help to maintain the appropriate vaginal pH18,19 and increase vaginal moisture as they contain both water and polymers that insure hypo-osmolality of the moisturizer and that water adheres to the vaginal mucosa.19 Local non-hormonal treatments, such as vaginal moisturizers, do not affect follicle-stimulating hormone or estradiol serum concentrations and have thus been shown to be safe for long-term use.20,21 This benefits the population of menopausal women who wish to, or must, avoid hormonal treatment.20,22
This Phase 2b study (OXYPEP202 [EudraCT number: 2016-000158-36]) double-blind, randomized study was designed to evaluate the efficacy of non-oxytocin gel, Aqueous Hypromellose-based vaginal gel, compared to an equivalent gel also containing oxytocin gel, in treating the MBS in postmenopausal women with VVA.
Materials and Methods
This study was conducted in compliance with the International Conference on Harmonization Harmonized Tripartite Guideline for GCP guidelines and in accordance with the ethical principles originating from the Declaration of Helsinki. The protocol was reviewed and approved by the Independent Ethics Committee (IEC) in Stockholm, Sweden (approval registration number 2016/601-32), and all participants provided written informed consent.
Between April and November 2016, the study recruited subjects from three sites in Sweden (Karolinska University Hospital in Huddinge, Uppsala University Hospital in Uppsala, and Norrland’s University Hospital in Umeå) and comprised of 5 visits: screening visit/week −3 to week 0 (Visit 0), randomization visit/week 0 (Visit 1), treatment follow-up visit/week 4 (Visit 2), end-of-treatment visit/week 12 (Visit 3), and a telephone follow-up visit/week 14 (Visit 4). The subjects were enrolled to the study by a research nurse or one of the investigators.
The gels were produced under GMP conditions at Apotek Produktion & Laboratorier AB, Kungens Kurva, Stockholm. The Aqueous Hypromellose-based vaginal gel was the same as the oxytocin gel, but the latter one also included 400 IU of oxytocin per dose.
Study Design
The study was a multi-center, randomized, parallel group, double-blind study, with a follow- up of 12 weeks daily treatment. The primary objective was to evaluate the efficacy of oxytocin gel and Aqueous Hypromellose-based vaginal gel in reducing the severity of the self-identified Most Bothersome Symptom (MBS) of VVA associated with menopause after 12 weeks of daily treatment, and the secondary objective was to evaluate safety and tolerability of 400 IU of oxytocin gel and Aqueous Hypromellose-based vaginal gel. Additional secondary endpoints included severity of the MBS of VVA symptoms at 4 weeks, vaginal pH, percentage of superficial squamous cells, severity of each individual VVA symptom, percentage of parabasal cells and maturation value at 4 and 12 weeks, and Quality of Life questions analyzed at 12 weeks compared with start point. Following screening and baseline assessments, the participants were randomized to one of the treatments: Aqueous Hypromellose-based vaginal gel (1 x 1 mL) (with the same composition, appearance, and route of administration as oxytocin gel, but without oxytocin) daily for 12 weeks administered intravaginally or oxytocin vaginal gel (1 x 1 mL/400 IU) daily for 12 weeks administered intravaginally.
This was a double-blind study and hence subjects, the investigators, and study site personnel remained blinded to study treatment throughout the study. The packaging of the treatment compounds was identical in appearance to maintain blinding. Neither the subjects nor the investigators could identify the treatment from the packaging or label of the IMP. Treatment code envelopes, indicating the treatment randomization for each randomized subject, were available to the investigators at the study sites. No treatment code envelopes were broken until after declaration of clean file and database lock of the study.
Study Population
Females aged 40–65 years who were either postmenopausal or had undergone surgical bilateral oophorectomy, with ≤5% superficial cells in vaginal smear cytology, a vaginal pH >5.0, a body mass index ≤32 kg/m2, an endometrial thickness of <4 mm, and at least one moderate to severe VVA symptom, but who were otherwise in good health and had provided signed informed consent, were considered eligible to participate in the study. In addition, women were to abstain from vaginal sexual activity and the use of vaginal douching within 24 hours prior to vaginal pH measurements. Further, women with an intact uterus were required to have an acceptable result from a Pap smear conducted within 6 months prior to the initial dose of study medication.
Women were not permitted to use estrogen alone or estrogen/progestin for any of the following time periods: (a) Vaginal hormonal products (rings, creams, gels, vaginal suppositories) within 12 weeks prior to the screening visit, (b) transdermal estrogen alone or estrogen/progestin products including percutaneous estrogen gels for at least 12 weeks prior to the screening visit, (c) oral estrogen and/or progestin therapy within 12 weeks prior to the screening visit, (d) intrauterine progestin therapy within 12 weeks prior to the screening visit, (e) progestin implants and estrogen alone injectable drug therapy within 12 weeks prior to the screening visit, and (f) estrogen pellet therapy or pregestational injectable drug therapy within 6 months prior to the screening visit.
Use of concomitant medications was allowed; however, use of any herbal products, nutritional supplements, vaginal lubricants, and moisturizers with known estrogenic effects and/or known or suspected to interact with oxytocin therapy was not permitted.
Assessments
Efficacy measurements included evaluation of VVA symptoms including the MBS, assessments of vaginal pH, and vaginal cytology (% superficial cells).
The VVA symptoms used to identify MBS at baseline were (all recorded on a 4 graded scale: none, mild, moderate, or severe):
- Vaginal dryness
- Vaginal and/or vulvar irritation/itching
- Pain, burning, or stinging when urinating
- Vaginal discomfort and/or pain associated with vaginal sexual activity
The levels of VVA symptoms including vaginal dryness, vaginal/vulvar irritation/itching, dysuria, and dyspareunia were self-assessed by subjects at Screening (visit 0), Visits 2 and 3 using a 4-point scale (none, mild, moderate, and severe) using the VVA symptoms self-assessment questionnaire. The absence or presence of any vaginal bleeding associated with vaginal sexual activity was also noted in the same questionnaire. In addition, the subjects were to specify the symptom that she identified as the MBS.
Vaginal pH was measured at screening and visits 2 and 3, using a pH indicator, ECPH601PLUS (Thermo Fisher Scientific). The accuracy of the technique was ± 0.01 units. Vaginal fluid was collected before the vaginal smears were obtained and was applied to the pH indicator for measurement of pH by the staff. Vaginal cytology was assessed at Screening and Visits 2 and 3 to determine the percentage of superficial, intermediate, and parabasal cells. Vaginal smears were collected from the lateral vaginal walls according to laboratory instructions to evaluate vaginal cytology.
Safety was evaluated throughout the study, including adverse event (AE) reporting, vital signs at each visit, and at baseline and week 12 via clinical laboratory tests, transvaginal ultrasound (including endometrial thickness), Pap smear, and physical and gynecological examinations.
Statistical Analysis
Data from a similar study were used to determine the standard deviation needed to estimate the number of subjects to be included. The number of fully evaluable subjects needed in each treatment group to reach 80% power using a two-sided test at 5% significance level was estimated to be 80.
Eligible subjects were randomized at Visit 1 (Day 0). The randomization code was created by an independent statistician using a computer-generated randomization schedule prepared prior to the start of the study. The randomization was made in blocks (Block size = 4) and stratified by center. The subject numbers were allocated sequentially.
The efficacy evaluation was performed using data from all included subjects who fulfilled the entry criteria, who were dispensed study medication, and who had at least one efficacy assessment after randomization, ie an Intention-To-Treat (ITT) approach, as well as identification of a Per Protocol (PP) subset who did not have any major protocol violations. The data were analyzed according to an ITT approach. Similar results were obtained with the PP approach, as only four patients were excluded in the analysis using the PP approach. The safety evaluation included all subjects who took at least one dose of the study treatment.
Comparisons between the groups were done using the Wilcoxon rank-sum test. The Wilcoxon signed-rank test was used when comparing post-baseline data with baseline data within each group. A p-value below 5% was considered significant. As the p-values when comparing the groups were above 5%, the conclusion was drawn that it could not be excluded that the treatments were similar and, as a result, the focus was then on analyzing the change from baseline in the Aqueous Hypromellose-based vaginal gel group.
Change from baseline to week 4 in severity of the VVA symptoms that has been self-identified by the subject as being the MBS to her at baseline, as well as change from baseline to week 4 and week 12 in severity of individual VVA symptoms, were analyzed using the Wilcoxon signed-rank test (which is the same method as used for the primary efficacy endpoint).
Results
A total of 157 subjects were randomized in the study (oxytocin gel vs Aqueous Hypromellose-based vaginal gel: 79 vs 78, see Figure 1) and included in the statistical analyses. The women had an average age of 58 and 59 years (Table 1). The demographic and baseline characteristics were comparable between the oxytocin gel and Aqueous Hypromellose-based vaginal gel groups. The study was ended according to protocol after all subjects had completed their last study visit at week 12 in February 2017.
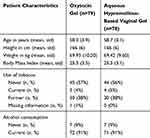 |
Table 1 Subject Demographic and Baseline Characteristics (Mean, Standard Deviation or Number of Observation and Percent) |
 |
Figure 1 Subject disposition. |
Primary Efficacy Endpoint
Most Bothersome VVA Symptom
Highly significant (p<0.0001, See Table 1) improvements from baseline at both 4 weeks and 12 weeks follow-up for the most bothersome VVA symptom, of which dyspareunia and vaginal dryness were the most frequently occurring, were noted in both groups. There was no statistically significant difference between the oxytocin gel and Aqueous Hypromellose-based vaginal gel groups in the change from baseline to week 4 and week 12 in severity of the most bothersome VVA symptom see Table 2. Statistical analysis revealed no significant effect of patient age or study site upon the effects of the Aqueous Hypromellose-based vaginal gel upon the most bothersome VVA symptoms.
 |
Table 2 MBS: Comparison of Oxytocin Gel versus Aqueous Hypromellose-Based Vaginal Gel Using the Change from Baseline Within (Wilcoxon Signed Rank Test) and Between (Wilcoxon Rank Sum Test) the Groups |
Secondary Efficacy Endpoints
Vaginal pH
There was no statistically significant difference between the two treatment groups in change from baseline to either week 4 or week 12 in vaginal pH. However, there was a highly significant (see Table 3) decrease from baseline in both treatment groups at week 4 and week 12 (Mean changes: oxytocin gel: −0.38, Aqueous Hypromellose-based vaginal gel: −0.53) and week 12 (oxytocin gel: −0.46, Aqueous Hypromellose-based vaginal gel: −0.73), showing a positive effect of both treatments.
 |
Table 3 pH: Comparison of Oxytocin Gel versus Aqueous Hypromellose-Based Vaginal Gel Using the Change from Baseline Within (Wilcoxon Signed Rank Test) and Between (Wilcoxon Rank Sum Test) the Groups |
Vaginal Cytology (Superficial Cells)
There was no statistically significant difference between the two treatment groups in change from baseline to either week 4 or week 12 in % of superficial cells, see Table 4. However, there was a highly significant (see Table 4) increase from baseline in both treatment groups at week 4 and week 12 (Mean changes: oxytocin gel: +2.86, Aqueous Hypromellose-based vaginal gel: +2.33) and week 12 (oxytocin gel: +3.77 Aqueous Hypromellose-based vaginal gel: +1.94), showing a positive effect of both treatments.
Vaginal Dryness
Highly statistically significant improvement from baseline at both 4 weeks and 12 weeks follow-up was noted in both groups. There was no statistically significant difference between the oxytocin gel and Aqueous Hypromellose-based vaginal gel groups in the change from baseline to week 4 and week 12 in severity of the vaginal dryness, see Table 5.
Dyspareunia
Highly statistically significant improvements from baseline at both 4 weeks and 12 weeks follow-up were noted in both groups. There was no statistically significant difference between the oxytocin gel and Aqueous Hypromellose-based vaginal gel groups in the change from baseline to week 4 and week 12 in severity of the Dyspareunia, see Table 6.
Other Individual VVA Symptoms
There was no statistically significant difference between the two treatment groups in change from baseline to week 4 or week 12 in severity of any of the other individual VVA symptom (vulvar/vaginal irritation and itching, dysuria, and vaginal bleeding)
However, there were highly significant improvements from baseline in both treatment groups at week 4 and Week 12 for all variables (Table 7).
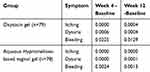 |
Table 7 Two-Sided p-values for the Other Individual VVA Symptoms (All Changes are Improvements) |
Safety
A total of 27 subjects (33.8%) reported 39 AEs in the Aqueous Hypromellose-based vaginal gel group compared to 32 subjects (39.5%) in the oxytocin gel group reporting 49 AEs. During the treatment period, one serious adverse event (SAE, breast cancer) was reported by one subject in the oxytocin gel group and was assessed as unlikely related to the study compound. No SAEs were reported by subjects in the Aqueous Hypromellose-based vaginal gel group during the treatment period.
The most frequently reported AEs were vaginal discharge, urinary tract infection, and vaginal odor. About twice as many subjects reported these AEs in the oxytocin gel group as compared to the Aqueous Hypromellose-based vaginal gel group. No safety and tolerability concerns were noted based on vital signs, physical examinations and clinical laboratory evaluations, gynecological examinations, breast examinations, transvaginal ultrasound (including endometrial thickness), and Pap smear evaluations. Occasional abnormal clinically significant findings were noted.
Three subjects prematurely stopped the investigational medicine product (IMP) treatment due to AEs (all of them in the oxytocin gel group; assessed as possibly related, not related, and unlikely related to the IMP). None were assessed as probably related to the IMP. All these AEs were deemed as resolved by study completion except one (atrial fibrillation) that was assessed as not related to the IMP treatment.
Discussion
This was a randomized, parallel group, double-blind Phase 2b study designed to evaluate the efficacy of Aqueous Hypromellose-based vaginal gel and oxytocin gel in treating postmenopausal women with VVA symptoms. The primary objective was to evaluate the efficacy in reducing the severity of the MBS of VVA associated with menopause after 12 weeks of treatment. The results showed that both Aqueous Hypromellose-based vaginal gel and oxytocin gel had statistically significant positive effects. The results showed that treatment with oxytocin gel had no statistically significant effect compared to Aqueous Hypromellose-based vaginal gel. Similar results were obtained when examining the main secondary efficacy endpoints (vaginal pH and % superficial cells).
The results of this study are possible to generalize to a population fulfilling the entry criteria for the study. The main entry criteria for the women possible to include were age 40–65 years who were postmenopausal, <5% superficial cells in vaginal smear cytology, vaginal pH > 5.0, moderate to severe vulvovaginal atrophy symptoms, and otherwise in good health.
Both Aqueous Hypromellose-based vaginal gel and oxytocin gel treatments resulted in improvements over time in the severity of the most bothersome VVA symptom, as well as in vaginal pH and % superficial cells measurements. The magnitude of the effect of Aqueous Hypromellose-based vaginal gel on MBS was on the same level as has been reported for eg, estrogen-based products23. Hence, it is not surprising that oxytocin as add-on did not show an additional effect on these parameters. Earlier studies indicating the efficacy of oxytocin alone13,14 were based upon small populations and small groups for internal analysis.
In order to rule out any suspicions about possible mix-ups between the Aqueous Hypromellose-based vaginal gel and oxytocin gel (oxytocin syringes/tubes), mistakes during the manufacturing, labelling and packaging, or handling of syringes/tubes, a number of control tests have been performed by the Sponsor, such as examination of unused IMP packaging and content (data available upon request). The results of these tests indicate that the labelling was correct. Further, the data from the two pharmacokinetic evaluations performed by the Sponsor during the clinical study indicate that oxytocin has been released from the gel containing oxytocin, as confirmed by an increased serum oxytocin level in subjects that were treated with oxytocin gel (data available upon request). No corresponding increase in serum oxytocin levels was observed in subjects treated with Aqueous Hypromellose-based vaginal gel, hence, indicating that a) there was no mix-up, and b) the vaginal mucosa was exposed to oxytocin during the course of treatment in the oxytocin gel treatment arm.
No safety or tolerability concerns were identified in this study in subjects treated with either oxytocin gel or Aqueous Hypromellose-based vaginal gel. There were no major differences in AE reporting between the two treatment groups. One SAE during the treatment period was reported (in the oxytocin gel group, assessed as unlikely related to the IMP). The most frequently reported AEs in both treatment-groups were vaginal discharge, vaginal odor (possibly related), and urinary tract infection (not related). These are similar findings as to what was obtained from a previous Phase 2b double-blind placebo-controlled multi-dose study (OXYPEP201) that evaluated the 12-week efficacy of oxytocin gel in postmenopausal women with symptoms of VVA.24 It is likely that experience of symptoms of vaginal discharge and vaginal odor are correlated to a certain extent. There are two plausible reasons for the increased vaginal discharge; it may be a consequence of increased physiological function or vaginal secretion. In some of the subjects, the odor was due to bacterial vaginosis, and the subjects were treated with antibiotics. The reason for developing vaginal vaginosis could be that during Screening, week 4, and week 12 visits, the doctor took vaginal smear cytology samples for analysis at a central lab. In many of these women, it is rather difficult to get samples and the vaginal wall is very thin. During the smear sample collection, the wall could have sometimes been damaged and started to bleed. In this circumstance, there may be a higher risk of bacterial vaginosis.
A limitation of the current study is that it involved only postmenopausal women and did not determine the effects of the Aqueous Hypromellose-based vaginal gel upon vaginal dryness in premenopausal women. Future research will include premenopausal women as well as women who have survived breast cancer or other forms of cancer, breastfeeding women, and women with vestibulitis.
Conclusion
Overall, this study showed equally good outcomes for both the gel containing oxytocin (ie, oxytocin gel) and the gel not containing oxytocin (ie, Aqueous Hypromellose-based vaginal gel) in treating postmenopausal women with VVA symptoms. Both oxytocin gel and Aqueous Hypromellose-based vaginal gel treatment reduced the severity of the most bothersome VVA symptom, lowered vaginal pH, and increased the percentage of superficial cells of the vaginal mucosa. In addition, no safety or tolerability concerns were identified. In conclusion, given the benefits of avoiding the use of hormones, Aqueous Hypromellose-based vaginal gel is an attractive first choice of treatment before hormone-containing gels are considered for the treatment of VVA symptoms.
Abbreviations
AE, adverse event; IMP, investigational medicine product; ITT; intention-to-treat; MBS, most bothersome symptoms; PP, per protocol; SAE, serious adverse event; VVA, vulvovaginal atrophy.
Ethics Approval and Informed Consent
This study was conducted in compliance with the International Conference on Harmonization Harmonized Tripartite Guideline for GCP guidelines and in accordance with the ethical principles originating from the Declaration of Helsinki. The protocol was reviewed and approved by the Independent Ethics Committee (IEC) in Stockholm, Sweden (approval registration number 2016/601-32), and all participants provided written informed consent.
Acknowledgments
Medical writing assistance for this publication was provided by Elisabeth Liljensten, DDS, PhD, Devicia AB, Sweden.
Funding
This work was funded by Peptonic Medical AB, Sweden.
Disclosure
Dr Inger Sundström Poromaa reports personal fees from Peptonics, during the conduct of the study; personal fees from Bayer AB, Shire/Takeda, and Gedeon Richter, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Iosif CS, Bekassy Z. Prevalence of genito-urinary symptoms in the late menopause. Acta Obstet Gynecol Scand. 1984;63:257–260. doi:10.3109/00016348409155509
2. Lethaby A, Ayeleke RO, Roberts H. Local oestrogen for vaginal atrophy in postmenopausal women. Cochrane Database Syst Rev. 2016;2016:Cd001500. doi:10.1002/14651858.CD001500.pub3
3. Henriksson L, Stjernquist M, Boquist L, Cedergren I, Selinus I. A one-year multicenter study of efficacy and safety of a continuous, low-dose, estradiol-releasing vaginal ring (Estring) in postmenopausal women with symptoms and signs of urogenital aging. Am J Obstet Gynecol. 1996;174:85–92. doi:10.1016/s0002-9378(96)70378-2
4. Caillouette JC, Sharp CF
5. Bachmann GA. The clinical platform for the 17beta-estradiol vaginal releasing ring. Am J Obstet Gynecol. 1998;178:S257–S260. doi:10.1016/s0002-9378(98)70558-7
6. Grady D. Clinical practice. Management of menopausal symptoms. N Engl J Med. 2006;355:2338–2347. doi:10.1056/NEJMcp054015
7. Cano A, Estévez J, Usandizaga R, et al. The therapeutic effect of a new ultra low concentration estriol gel formulation (0.005% estriol vaginal gel) on symptoms and signs of postmenopausal vaginal atrophy: results from a pivotal Phase III study. Menopause. 2012;19:1130–1139. doi:10.1097/gme.0b013e3182518e9a
8. Freedman M, Kaunitz AM, Reape KZ, Hait H, Shu H. Twice-weekly synthetic conjugated estrogens vaginal cream for the treatment of vaginal atrophy. Menopause. 2009;16:735–741. doi:10.1097/gme.0b013e318199e734
9. Fernandes T, Costa-Paiva LH, Pedro AO, Baccaro LFC, Pinto-Neto AM. Efficacy of vaginally applied estrogen, testosterone, or polyacrylic acid on vaginal atrophy: a randomized controlled trial. Menopause. 2016;23(7):792–798. doi:10.1097/gme.0000000000000613
10. Kallak TK, Uvnäs-Moberg K. Oxytocin stimulates cell proliferation in vaginal cell line Vk2E6E7. Post Reprod Health. 2017;23:6–12. doi:10.1177/2053369117693148
11. Uvnas-Moberg K, Petersson M. [Oxytocin, a mediator of anti-stress, well-being, social interaction, growth and healing] [Original text in German]. Z Psychosom Med Psychother. 2005;51:57–80. doi:10.13109/zptm.2005.51.1.57
12. Al-Saqi SH, Jonasson AF, Naessén T, Uvnäs-Moberg K. Oxytocin improves cytological and histological profiles of vaginal atrophy in postmenopausal women. Post Reprod Health. 2016;22:25–33. doi:10.1177/2053369116629042
13. Al-Saqi SH, Uvnäs-Moberg K, Jonasson AF. Intravaginally applied oxytocin improves post-menopausal vaginal atrophy. Post Reprod Health. 2015;21:88–97. doi:10.1177/2053369115577328
14. Torky HA, Taha A, Marie H, et al. Role of topical oxytocin in improving vaginal atrophy in postmenopausal women: a randomized, controlled trial. Climacteric. 2018;21:174–178. doi:10.1080/13697137.2017.1421924
15. Ghorbani Z, Mirghafourvand M. The efficacy and safety of intravaginal oxytocin on vaginal atrophy: A systematic review. Post Reprod Health. 2020;2053369120946645. doi:10.1177/2053369120946645.
16. Society NAM. Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20:
17. 1177 Vårdguiden. Klimakteriebesvär [Health Care Guide. Menopausal Symptoms]; 2017. Available from: https://www.1177.se/Fakta-och-rad/Sjukdomar/Klimakteriebesvar1/.
18. Ayehunie S, Wang YY, Landry T, Bogojevic S, Cone RA. Hyperosmolal vaginal lubricants markedly reduce epithelial barrier properties in a three-dimensional vaginal epithelium model. Toxicol Rep. 2018;5:134–140. doi:10.1016/j.toxrep.2017.12.011
19. Edwards D, Panay N. Treating vulvovaginal atrophy/genitourinary syndrome of menopause: how important is vaginal lubricant and moisturizer composition? Climacteric. 2016;19:151–161. doi:10.3109/13697137.2015.1124259
20. Lima SM, Bernardo BFA, Yamada SS, et al. Effects of Glycine max (L.) Merr. soy isoflavone vaginal gel on epithelium morphology and estrogen receptor expression in postmenopausal women: a 12-week, randomized, double-blind, placebo-controlled trial. Maturitas. 2014;78(3):205–211. doi:10.1016/j.maturitas.2014.04.007
21. Jokar A, Davari T, Asadi N, Ahmadi F, Foruhari S. Comparison of the hyaluronic acid vaginal cream and conjugated estrogen used in treatment of vaginal atrophy of menopause women: a randomized controlled clinical trial. Int J Community Based Nurs Midwifery. 2016;4:69–78.
22. Lima SMRR, Yamada SS, Reis BF, et al. Effective treatment of vaginal atrophy with isoflavone vaginal gel. Maturitas. 2013;74(3):252–258. doi:10.1016/j.maturitas.2012.11.012
23. Vagifem. Vagifem® (estradiol vaginal inserts) 10 mcg; 2017. Available from: https://www.vagifem.com/.
24. Vagitocin [Investigator’s Brochure] Edition 7.0.; Peptonic Medical. March 2016.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



