Back to Journals » Neuropsychiatric Disease and Treatment » Volume 15
Role of paliperidone palmitate 3-monthly in the management of schizophrenia: insights from clinical practice
Received 19 February 2018
Accepted for publication 26 November 2018
Published 11 February 2019 Volume 2019:15 Pages 449—456
DOI https://doi.org/10.2147/NDT.S140383
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Alicia Lopez, Jose Rey
Department of Pharmacy Practice, Nova Southeastern University, Fort Lauderdale, FL, USA
Abstract: Schizophrenia is a complex, chronic psychiatric disorder associated with reduced quality of life and shortened life span. The majority of patients with schizophrenia will relapse within 1 year following an acute episode. The ultimate goals of treatment are to improve functional capabilities, minimize residual symptoms during periods of remission, and decrease relapse frequency and duration, as each relapse brings with it the possibility of a worsening prognosis. Maintaining therapeutic continuity is essential for long-term, positive patient outcomes in schizophrenia. Medication nonadherence and symptomatic relapses magnify the disease burden associated with this disorder. Medication adherence in chronic disease states generally improves with a decrease in dosing frequency. Long-acting injectable (LAI) antipsychotics were developed to improve patient outcomes secondarily to improving medication adherence. Paliperidone palmitate 3-monthly injection (PP3M) is the only LAI available with a quarterly dosing interval. PP3M has been US Food and Drug Administration-approved for use in the long-term maintenance treatment of schizophrenia in patients already controlled on once-monthly PP LAI (paliperidone palmitate once-monthly injection [PP1M]) for a minimum of 4 months. As current evidence supports the efficacy and tolerability of PP3M compared to PP1M and placebo, PP3M appears to be a viable treatment option for patients previously maintained on PP1M. However, to truly establish the place of PP3M in therapy relative to other oral antipsychotics and LAIs, more research is needed. This narrative review aims briefly to describe the pharmacotherapeutic characteristics of PP3M and summarize current literature pertaining to the use of PP3M in the management of schizophrenia.
Keywords: Trinza, Invega, long-acting, antipsychotic, LAI
Introduction
Schizophrenia is a complex, chronic psychiatric disorder characterized by active psychosis (eg, delusions, hallucinations, and disorganized thoughts), as well as deficits in cognitive and psychosocial functioning.1,2 This debilitating disorder is associated with reduced quality of life and shortened life span.2 While psychotherapeutic interventions can improve insight and functional abilities in individuals with schizophrenia, pharmacotherapy is a fundamental component of any treatment plan.3 Unfortunately, complete remission of symptoms is unlikely. Consequently, the ultimate goals of treatment are to improve functional capabilities, minimize residual symptoms during periods of remission, and decrease relapse frequency and duration.3
It is estimated that >85% of patients with schizophrenia will relapse within 1 year following an acute episode.3,4 With each relapse comes the possibility of a worsening prognosis, which is why preventing relapse is one of the primary treatment goals of the management of schizophrenia.5–7 The appropriate use of maintenance antipsychotic (AP) medications improves (reduces) relapse rates. APs have been found to decrease the 1-year relapse rate to 18%–32%.3,4 For APs to be effective, they must be prescribed and taken appropriately with good adherence to the treatment plan. Patient nonadherence in schizophrenia is estimated at 40%–80%.8,9 Nonadherence is multifactorial in nature. Potential causes may include poor insight into the illness and thus the need for medications, concern regarding actual or potential side effects, persistent residual symptoms, costs to the patient, stigma regarding schizophrenia, or the misbelief that medications are no longer needed once remission is attained.10 Maintaining therapeutic continuity is believed to be essential for long-term, positive patient outcomes.11 Nonadherence is one of the greatest challenges faced by clinicians, families, and persons with this complicated psychiatric disorder.
Medication nonadherence and symptomatic relapses magnify the disease burden associated with schizophrenia.12,13 For the patient, this may be experienced as lost productivity, missed working hours, disruption to the family and living environment, and diminished quality of life.14 This burden can be far-reaching. A systematic review evaluating the global economic impact of schizophrenia identified an annual cost per country of US$94 million up to $102 billion, depending on the country.12 The annual economic impact in the US alone is predicted to range from $25 billion up to $102 billion, depending on the study.12,13 These figures include direct costs (eg, medical care and social services), indirect costs, (eg, unemployment and premature mortality), and intangible costs (eg, reduced quality of life for patients, their families, and caregivers).12
It has been established that medication adherence in chronic disease states generally improves with a decrease in dosing frequency.15,16 Long-acting injectable (LAI) APs were developed to improve patient outcomes secondary to improving medication adherence by providing a sustained therapeutic effect that requires less frequent dosing.17 Whether or not LAIs improve adherence or decrease relapse rates in schizophrenia is not entirely clear, due to conflicting results in randomized controlled trials; however, mirror-image studies appear to favor the use of LAIs for these reasons.6,18–21 A recent claim-based analysis of posthospitalization adherence and rehospitalization outcomes in Medicaid patients with schizophrenia found that patients initiated on an LAI were less likely to be nonadherent (adjusted OR 0.35, 95% CI 0.27–0.46; P<0.001) or rehospitalized (adjusted OR 0.73, 95% CI 0.54–0.99; P=0.041) than patients receiving oral medications. While first-generation AP (FGA) and second-generation AP (SGA) LAIs both appeared to improve adherence, only SGA LAIs resulted in a lower risk of rehospitalization.21
Extended dosing intervals of LAIs are more convenient than the daily dosing required of oral APs (OAPs).17 Additionally, as LAIs must be administered by a health care provider, they provide clinicians with the ability to monitor adherence objectively.6,9 While multiple LAIs are available with biweekly and monthly dosing intervals, including both FGAs and SGAs, paliperidone palmitate 3-monthly injection (PP3M) is the only LAI available with a quarterly dosing interval given every 12 weeks.17,22,23 This narrative review aims briefly to describe the pharmacotherapeutic characteristics of PP3M and summarize current literature pertaining to the use of PP3M in the management of schizophrenia and its clinical utility.
Pharmacological properties
Paliperidone (9-hydroxyrisperidone), the primary active metabolite of risperidone, is a benzisoxazole of the SGA class. Like risperidone, paliperidone blocks serotonin 5HT2A receptors, D2 receptors, α1 and α2 adrenoceptors, and H1 receptors.24 Paliperidone is available as a once-daily oral tablet (Invega), a once-monthly injection (Invega Sustenna), and a 3-monthly injection (Invega Trinza in the US and Trevicta in the EU) manufactured by Janssen Pharmaceuticals with formulation development provided by Alkermes.17,22,23 The available PP3M administration dosage strengths of 273 mg, 410 mg, 546 mg, and 819 mg PP correspond to actual doses of 175 mg, 263 mg, 350 mg, and 525 mg PP, respectively.14 To increase the dosing interval, the particle size of the nanocrystal technology utilized in paliperidone palmitate once-monthly injection (PP1M) has been increased. PP is the palmitate salt ester of paliperidone.17,22 It is slightly soluble in polar solvents.24 PP3M is available as an aqueous suspension with nanocrystals dispersed throughout.24 Once injected intramuscularly, the nanocrystals dissolve slowly.14 They are subsequently hydrolyzed to paliperidone before diffusing into the circulatory system.14 After injection, PP3M begins systemic release immediately, and continues for up to 18 months.14
Approved indications
PP3M has been US Food and Drug Administration (FDA)-approved for use in the long-term maintenance treatment of schizophrenia. Individuals being considered for treatment with PP3M should be adequately treated and stable on PP1M for a minimum of 4 months prior to initiation of PP3M.24
Dosage and administration
General guidance
PP3M may be initiated once a patient is established and stable on PP1M for at least 4 months. For the purpose of determining an adequate maintenance dose, at least the last two doses of PP1M should have remained consistent. PP3M can be given at the time the next PP1M would be due, at an equivalent of 3.5-fold-higher dose (Table 1). The actual date of the first injection of PP3M can be given within 7 days, before or after, of when the PP1M would be due. PP3M should be administered by a health care professional on a quarterly basis. It is intended for intramuscular injection in either the deltoid or gluteal muscles. The entire dose should be given as a single injection using the manufacturer-provided needles. When preparing to give the injection, PP3M should be mixed thoroughly before the needle is attached to the syringe. With cap still attached, shake vigorously with a loose wrist in a vertical up-and-down motion for at least 15 seconds to provide an even distribution of this aqueous suspension. Injection sites should be rotated to minimize the risk of injection-site reaction.14,24
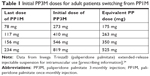  | Table 1 Initial PP3M doses for adult patients switching from PP1M |
Once established on PP3M, subsequent injections should be given every 3 months. Dose adjustments can be made within the range of 273–819 mg based on individual patient tolerability and response. It should be taken into consideration that the full response to a change in PP3M dose may not be seen for several months. If a follow-up injection of PP3M is missed, the planned dose can still be administered as long as it is <4 months since the last injection. If it has been at least 4 months, and not >9 months since the last injection, a modified dosing regimen will be required using PP1M (Table 2). If more than 9 months has passed since the last PP3M, it is recommended to reestablish treatment with PP1M for at least 4 months before considering reinitiating PP3M. Additionally, it is important that patients still be followed closely for clinical monitoring and psychosocial focused behavioral therapy. Even though they will require fewer interactions pertaining to medication administration, their mental health providers should not see them any less frequently than they would for any patients being treated with other AP regimens.
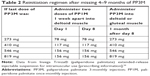  | Table 2 Reinitiation regimen after missing 4–9 months of PP3M |
Special populations
Renal and hepatic impairment
Use of PP3M in patients with renal or hepatic impairment has not been well studied. As per the manufacturer, PP3M should not be used in moderate–severe renal impairment, defined as creatinine clearance of <50 mL/min. In patients with creatinine clearance of ≥50 mL/min but <80 mL/min, the dose of PP3M should be based on the previously established dose of PP1M. Recommendations for use in hepatic impairment are based on studies of oral paliperidone. Paliperidone has not been studied in severe hepatic impairment. In mild–moderate hepatic impairment, no dose adjustment of oral paliperidone was required.24
Pregnancy and lactation
Due to the extended dosing interval associated with PP3M, the likelihood of fetal exposure is increased when compared to other AP-dosage forms. Two case reports have been published detailing the use of PP1M during pregnancy.25,26 In both cases, PP1M appears to have been well tolerated, with no fetal or neonatal complications apparent at time of publication.25,26
In human studies with risperidone, the primary active metabolite, paliperidone, was excreted in breast milk.24,27 Similarly, paliperidone was excreted in breast milk in animal studies with paliperidone.24 Considering the potential impact of fetal and neonatal exposure to APs and the lack of solid information available to guide the decision-making process, the decision to use PP in pregnancy and lactation needs to be made carefully with full awareness of the risks and benefits to the patient and the fetus. Since PP3M was approved in 2015 in the US market, it has not carried a simple pregnancy category (A, B, C, D, X) like many of the other APs, due to the FDA doing away with this category system at the beginning of 2015.
Geriatrics
Clinical trials for PP3M have not included many subjects aged 65 years and above.24 As such, it is difficult to predict differences in treatment response between elderly patients and those <65 years of age. Since PP3M is known to be substantially excreted by the kidney, careful monitoring of renal function is recommended by the manufacturer and doses adjusted accordingly.15
Cost assessment
The cost of PP3M is dose-dependent.41 Though the per-dose cost of PP3M is greater than that of the equivalent PP1M dose, costs will average out and be equivalent when calculated over a 3-month period for each drug (Table 3).41 Since LAIs must be injected by a health care provider, PP3M will cost less overall, due to the need for fewer injections, even though the total drug cost of PP1M and PP3M is equivalent. While the frequency of follow-up care should not change just because the dosing interval of PP3M is extended, the actual health care-associated costs should be slightly reduced.42,43
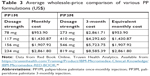  | Table 3 Average wholesale-price comparison of various PP formulations (US$) |
A recent economic analysis assessing the cost-utility and cost-effectiveness of PP3M in the Netherlands found PP3M to be superior to the comparators PP1M, risperidone LAI, haloperidol LAI, and oral olanzapine. PP3M had the fewest total relapses/patient (0.36, 0.94, 1.39, 1.21, and 1.70), hospitalizations (0.11, 0.46, 0.40, 0.56, and 0.57), and emergency-room visits (0.25, 0.48, 0.99, 0.65, and 1.14), and the most quality-adjusted life-years (QALYs) gained (0.847, 0.735, 0.709, 0.719, and 0.656).42 Similarly, an economic analysis assessing the cost utility of that PP3M compared to PP1M in Spain found that PP3M had fewer relapses (0.080 vs 0.161), hospitalizations (0.034 vs 0.065), and emergency-room visits (0.045 vs 0.096) and more QALYs gained (0.677 vs 0.625).43 Similar studies evaluating the economic impact of PP3M on the US health system should be conducted in the future.
Current evidence
The extended dosing interval afforded by PP3M is novel. Approved by the FDA in 2015, PP3M remains the only LAI on the market with a quarterly dosing schedule.28 As a result, PP3M has garnered much attention from the medical and scientific communities, and multiple review articles have been published since PP3M entered the clinical landscape. Daghistani et al published one of the first narrative reviews evaluating the place of PP3M in therapy.17 The authors concluded that the novel, 3-monthly dosing regimen afforded by PP3M may improve clinical and economic outcomes for patients, caregivers, and the health system at large.17 Lamb et al concluded in a subsequent narrative review that PP3M is comparable to PP1M in both safety and efficacy, making it a viable alternative for patients for whom a longer interval between dosing is preferred.23 More recently, a comprehensive review including observational data and post hoc analyses of three clinical trials was published.29 The authors concurred with the previously mentioned conclusions, but also asserted the need for more comprehensive research into the long-term and real-world impact of PP3M in clinical practice.29 To date, three clinical trials and one observational study evaluating the use of PP3M have been completed and reported in the literature.17,23,29–32 Post hoc analyses of these initial studies have provided additional insight into the potential impact of PP3M on clinical practice.7,32–36 These studies will briefly be described in the following sections.
Primary studies
Ravenstijn et al
This open-label, Phase I, multicenter, randomized, parallel-group study assessed the pharmacokinetics, safety, and tolerability of PP3M in the context of schizophrenia or schizoaffective disorder (n=328).31 The study design included four randomized panels (A–D) of patients, each receiving a single dose intramuscular injection of 1 mg PP immediate release, followed by a washout period of 7–21 days and a subsequent intramuscular injection of PP3M. The dose of PP3M varied for each randomized group. Total study duration for panels A and C was 53–58 weeks. Total study duration for panels B and D was 79–84 weeks. A limited amount of pharmacokinetic data was reported, due to injection issues in a portion of the study participants. Peak plasma concentration occurred between days 23 and 34. Half-life appeared to be 2–4 months. A dose-dependent response was noted for mean plasma AUC∞ and maximum concentration. PP3M had a bioavailability of ~100%, irrespective of dose or injection site. Safety and tolerability of PP3M were comparable to those of PP1M. The most commonly reported treatment-emergent adverse events (TEAEs) were headache and nasopharyngitis. Other notable TEAEs included weight gain, back pain, and anxiety. Rare but serious TEAEs included QTc prolongation and psychiatric events. A total of seven patients withdrew from the study due to TEAEs, with the majority of these being due to psychiatric symptoms. Safety and tolerability of PP3M were found to be comparable to those of PP1M.
Berwaerts et al
This Phase III, randomized, multicenter trial evaluated the efficacy and safety of PP3M compared to placebo in schizophrenia.30 The study design included a 3-week screening phase, flexible-dose 17-week open-label transition phase to PP1M, 12-week open-label maintenance phase with PP3M, and then an open-ended double-blind phase. Of the 506 enrolled patients, 160 were randomized to PP3M during the double-blind phase. Of those patients not randomized to the double-blind phase, 16 PP1M patients were excluded due to TEAEs compared to ten PP3M patients. This study was terminated early, based on findings from an independent advisory board, due to significantly fewer relapses in the treatment group than the placebo group (7% vs 23%, HR 3.45, 95% CI 1.73–6.88; P<0.001). TEAEs were more common in the PP3M group than the placebo group, with headache (9% vs 4%), weight increase (9% vs 3%), nasopharyngitis (6% vs 1%), and akathisia (4% vs 1%) being the most common TEAEs reported. The placebo group experienced serious TEAEs at a greater rate than the study group, which generally resulted from worsening psychiatric symptoms. An elevated transaminase level in the placebo group was the only TEAE resulting in early study discontinuation. The results of this study suggest PP3M may result in a delayed time to relapse in patients with schizophrenia without an increased safety risk compared with other currently available PP formulations.
Savitz et al
This Phase III, double-blind, parallel-group, multicenter study compared PP1M with PP3M in adult patients (aged 18–70 years) with schizophrenia.37 Patients were initially stabilized on PP1M during a 17-week, flexible-dose, open-label phase, before being randomized 1:1 to either PP1M or PP3M for a 48-week double-blind phase. Relapse rates between groups were similar (PP3M, n=37, 8%; PP1M, n=45, 9%). Tolerability profiles were also similar between groups, with increased weight being the most common TEAE. Other TEAE profiles mimicked those seen in the Berwaerts et al trial. Both study groups reported a dropout rate of 3% during the double-blind phase due to serious TEAEs, which were generally the result of worsening psychiatric symptoms. PP3M was found to be noninferior to PP1M.
Joshi et al
This observational, retrospective, longitudinal, cohort study described real-world baseline characteristics and treatment patterns of patients with schizophrenia initiated on PP3M by evaluating pharmacy and medical claims data.35 PP3M was generally initiated following stabilization with PP1M, as per recommended prescribing guidelines. Most patients were initiated on a starting dose of 819 mg and remained on a stable dose during follow-up. Stabilization and adherence were measured by assessing time between claims, proportion of days covered, and hospitalizations. Among patients with ≥4 months of follow-up after the first dose, 85%–88% had a second dose. Among those with ≥4 months of follow-up after the second dose, 87%–90% received a third dose. Overall, the proportion of days covered for all patients increased, while health care-resource utilization decreased.
Secondary analyses
Katz et al
The authors utilized a survey to ascertain clinical trial participants’ and investigators’ judgments relating to importance of efficacy and safety parameters associated with APs.36 Subjects from the Ravenstijn et al and Savitz et al studies were included. Patients (n=214) and physicians (n=438) responded regarding preferences for hypothetical AP profiles defined by efficacy, safety, and mode of administration. Complete improvement in positive symptoms was rated the most important attribute by both patients and physicians. LAIs were universally preferred over OAPs (P<0.05). Physicians in particular identified a preference for 3-month LAIs over 1-month LAIs for nonadherent patients. Physicians were willing to trade efficacy in favor of adherence.
Chirila et al
This study compared occupational status and health care-resource use between treatment groups in the trials by Ravenstijn et al and Savitz et al.33 Though a low percentage of patients were employed at baseline for each study, the PP3M group was more likely than the placebo or PP1M groups to change occupational status positively. Subjects in the placebo groups were also more likely to be hospitalized during the study period, leading to decreased productivity. No significant between-group differences were identified pertaining to hospitalization rates for the PP1M group compared to the PP3M group (OR 1.16, 95% CI 0.70–1.93).
Gopal et al
A pooled analysis34 of the Ravenstijn et al and Savitz et al trials looked for predictors of changes to schizophrenia-related caregiver burden following treatment with PP1M or PP3M.34 A targeted questionnaire was sent to caregivers to quantify their schizophrenia-related burden. The majority of caregivers with considerable burden identified improvements in urging, worrying, tension, and supervision domains by the end of the trials. The improvements were related to relapse status, patient age, and age of diagnosis (P<0.001). Baseline LAI use and psychiatric hospitalization were not identified as being correlated to decreased caregiver burden. Switching from an OAP to an LAI also appeared to result in improved caregiver burden.
Weiden et al
A post hoc analysis of pooled data from multiple clinical trials evaluated times to relapse following discontinuation of oral PP, PP1M, and PP3M.7 A total of 449 patients were included, with 101 from oral PP groups, 203 from PP1M groups, and 145 from PP3M groups. Postwithdrawal median (95% CI) days to relapse were 58 (42–114) for oral PP, 172 (134–222) for PP1M, and 395 (274–not reached) for PP3M (P<0.0001, pairwise comparisons). At least half the patients remained relapse-free for approximately 2 months (oral PP), 6 months (PP1M), and 13 months (PP3M). LAIs appear to provide a protective benefit in time to relapse following discontinuation of therapy.
Savitz et al
This analysis built upon the results of the 2016 Savitz et al study by assessing symptomatic and functional remission in schizophrenia following transition to PP3M in patients previously stabilized on PP1M in a 48-week double-blind phase.32,37 Symptomatic remission was achieved in PP3M: 50.3% of the PP3M group and 50.8% of the PP1M group. Functional remission was achieved in PP3M: 42.5% of the PP3M group and 43.9% of the PP1M group. Combined symptomatic and functional remission was seen in 25.1% of the PP3M group and 26.6% of the PP1M group. Total rates of symptomatic and functional remission were similar between the PP1M and PP3M groups.
Ongoing and future research
Stronger evidence based on head-to-head clinical trials between LAIs and OAPs is needed to improve clinical decision-making. The results of several ongoing studies will hopefully add to the current body of evidence available to clinicians. EULAST, which compares oral and LAI formulations of aripiprazole and paliperidone, aims to investigate possible advantages of LAIs over OAPs (NCT02146547).38 Another ongoing investigation is DREAM (NCT02431702).39 This trial is comparing PP1M, PP3M, oral PP, and other OAPs to assess differences in time to relapse, as well as structural and functional changes in cognition. To push the dosing-interval boundary even further, a 6-month flexible dosing regimen of PP LAI is under investigation (NCT03345342).40 Hopefully, these studies and others like them will expand the scope of evidence-based medicine in the treatment of schizophrenia.
Efficacy and tolerability of PP3M have to this point primarily been established in highly controlled clinical trial settings. By their nature, these studies do not always provide an accurate representation of the real-world patients that will eventually be the target population for these medications. For example, the aforementioned Berwaerts et al study excluded patients without a stable residence, recent substance dependence, or clinically significant medical diagnoses.30 In addition to excluding patients with recent substance dependence or clinically significant medical diagnoses, Savitz et al also excluded patients at risk of suicide.37 Schizophrenia is a complicated diagnosis that often coincides with a variety of social, medical, and psychiatric concerns.2 To provide a more complete picture of the place of PP3M in therapy, additional studies are needed that include patient populations more representative of those seen in clinical practice, studies of longer duration, and studies that take place in real-world settings. Alternative study designs that have been proposed to increase the body of evidence for PP3M have included mirror studies involving real-world patients and multiarm head-to-head trials.29
Conclusion
PP3M remains a novel therapeutic option for the treatment of schizophrenia, being the only LAI on the market with a quarterly dosing schedule. Current evidence supports the efficacy and tolerability of PP3M compared to PP1M and placebo. As such, PP3M is a viable treatment option for patients previously maintained on PP1M. However, to establish the place of PP3M in therapy truly relative to other OAPs and LAIs, more research is needed. PP3M is currently approved for use in schizophrenia only. It would be worthwhile to assess efficacy and tolerability in other psychiatric conditions, such as schizoaffective disorder or bipolar disorder. Further evaluation in special populations is also needed. More comprehensive research into the long-term and real-world impact of PP3M in clinical practice will provide much-needed insight into the clinical utility of PP3M in relation to other available APs. Such studies would be of value to clinicians trying to understand the place of PP3M in practice.
Disclosure
JR has received payments from Janssen Pharmaceuticals’ speakers bureau and served on a Janssen-supported advisory board. AL reports no commercial or financial interests in regard to this article. The authors report no other conflicts of interest in this work.
References
Crismon ML, Kattura RS, Buckley PF, et al. Schizophrenia. In: DiPiro JT, Talbert RL, Yee GC, et al, editors. Pharmacotherapy: A Pathophysiologic Approach, 10e. New York, NY: McGraw-Hill Education; 2017. | ||
APA. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. | ||
Buchanan RW, Kreyenbuhl J, Kelly DL, et al; Schizophrenia Patient Outcomes Research Team (PORT). The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr Bull. 2010;36(1):71–93. | ||
Osser DN, Roudsari MJ, Manschreck T. The psychopharmacology algorithm project at the Harvard South Shore Program: an update on schizophrenia. Harv Rev Psychiatry. 2013;21(1):18–40. | ||
Kane JM. Improving patient outcomes in schizophrenia: achieving remission, preventing relapse, and measuring success. J Clin Psychiatry. 2013;74(9):e18. | ||
Leucht C, Heres S, Kane JM, Kissling W, Davis JM, Leucht S. Oral versus depot antipsychotic drugs for schizophrenia – a critical systematic review and meta-analysis of randomised long-term trials. Schizophr Res. 2011;127(1–3):83–92. | ||
Weiden PJ, Kim E, Bermak J, Turkoz I, Gopal S, Berwaerts J. Does half-life matter after antipsychotic discontinuation? a relapse comparison in schizophrenia with 3 different formulations of paliperidone. J Clin Psychiatry. 2017;78(7):e813–e820. | ||
Mert DG, Turgut NH, Kelleci M, Semiz M. Perspectives on reasons of medication nonadherence in psychiatric patients. Patient Prefer Adherence. 2015;9:87–93. | ||
Valenstein M, Blow FC, Copeland LA, et al. Poor antipsychotic adherence among patients with schizophrenia: medication and patient factors. Schizophr Bull. 2004;30(2):255–264. | ||
Velligan DI, Weiden PJ, Sajatovic M, et al. The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. J Clin Psychiatry. 2009;70 Suppl 4:1–46; quiz 47–48. | ||
Keith SJ, Pani L, Nick B, et al. Practical application of pharmacotherapy with long-acting risperidone for patients with schizophrenia. Psychiatr Serv. 2004;55(9):997–1005. | ||
Chong HY, Teoh SL, Wu DB, Kotirum S, Chiou CF, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016;12:357–373. | ||
Desai PR, Lawson KA, Barner JC, Rascati KL. Identifying patient characteristics associated with high schizophrenia-related direct medical costs in community-dwelling patients. J Manag Care Pharm. 2013;19(6):468–477. | ||
Gopal S, Vermeulen A, Nandy P, et al. Practical guidance for dosing and switching from paliperidone palmitate 1 monthly to 3 monthly formulation in schizophrenia. Curr Med Res Opin. 2015;31(11):2043–2054. | ||
Medic G, Higashi K, Littlewood KJ, Diez T, Granström O, Kahn RS. Dosing frequency and adherence in chronic psychiatric disease: systematic review and meta-analysis. Neuropsychiatr Dis Treat. 2013;9:119–131. | ||
Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15(6):e22–e33. | ||
Daghistani N, Rey JA. Invega Trinza: The first four-times-a-year, long-acting injectable antipsychotic agent. P T. 2016;41(4):222–227. | ||
Pilon D, Joshi K, Tandon N, et al. Treatment patterns in medicaid patients with schizophrenia initiated on a first- or second-generation long-acting injectable versus oral antipsychotic. Patient Prefer Adherence. 2017;11:619–629. | ||
Kane JM, Kishimoto T, Correll CU. Non-adherence to medication in patients with psychotic disorders: epidemiology, contributing factors and management strategies. World Psychiatry. 2013;12(3):216–226. | ||
Correll CU, Citrome L, Haddad PM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J Clin Psychiatry. 2016;77(suppl 3):1–24. | ||
Marcus SC, Zummo J, Pettit AR, Stoddard J, Doshi JA. Antipsychotic adherence and rehospitalization in schizophrenia patients receiving oral versus long-acting injectable antipsychotics following hospital discharge. J Manag Care Spec Pharm. 2015;21(9):754–769. | ||
Ostuzzi G, Papola D, Gastaldon C, Barbui C. New EMA report on paliperidone 3-month injections: taking clinical and policy decisions without an adequate evidence base. Epidemiol Psychiatr Sci. 2017;26(3):231–233. | ||
Lamb YN, Keating GM. Paliperidone palmitate intramuscular 3-monthly formulation: a review in schizophrenia. Drugs. 2016;76(16):1559–1566. | ||
Invega Trinza® (paliperidone palmitate) extended-release injectable suspension for intramuscular use: US [prescribing information]. Titusville, NJ: Janssen Pharmaceuticals Inc.; 2015. | ||
Özdemir AK, Pak ŞC, Canan F, Geçici Ö, Kuloğlu M, Gücer MK. Paliperidone palmitate use in pregnancy in a woman with schizophrenia. Arch Womens Ment Health. 2015;18(5):739–740. | ||
Zamora Rodríguez FJ, Benítez Vega C, Sánchez-Waisen Hernández MR, Guisado Macías JA, Vaz Leal FJ. Use of paliperidone palmitate throughout a schizoaffective disorder patient’s gestation period. Pharmacopsychiatry. 2017;50(1):38–40. | ||
Ilett KF, Hackett LP, Kristensen JH, Vaddadi KS, Gardiner SJ, Begg EJ. Transfer of risperidone and 9-hydroxyrisperidone into human milk. Ann Pharmacother. 2004;38(2):273–276. | ||
Johnson JUS. FDA approves Invega Trinza first and only four-timesa-year treatment for schizophrenia. 2015. Available from: https://www.jnj.com/media-center/press-releases/us-fda-approves-invega-trinza-first-and-only-four-times-a-year-treatment-for-schizophrenia. Accessed November 06, 2018. | ||
Brasso C, Bellino S, Bozzatello P, Montemagni C, Rocca P. Role of 3-monthly long-acting injectable paliperidone in the maintenance of schizophrenia. Neuropsychiatr Dis Treat. 2017;13:2767–2779. | ||
Berwaerts J, Liu Y, Gopal S, et al. Efficacy and safety of the 3-month formulation of paliperidone palmitate vs placebo for relapse prevention of schizophrenia: a randomized clinical trial. JAMA Psychiatry. 2015;72(8):830–839. | ||
Ravenstijn P, Remmerie B, Savitz A, et al. Pharmacokinetics, safety, and tolerability of paliperidone palmitate 3-month formulation in patients with schizophrenia: A phase-1, single-dose, randomized, open-label study. J Clin Pharmacol. 2016;56(3):330–339. | ||
Savitz AJ, Xu H, Gopal S, Nuamah I, Hough D, Mathews M. Paliperidone palmitate 3-month treatment results in symptomatic remission in patients with schizophrenia: a randomized, multicenter, double-blind, and noninferiority study. Int Clin Psychopharmacol. 2017;32(6):329–336. | ||
Chirila C, Nuamah I, Woodruff K. Health care resource use analysis of paliperidone palmitate 3 month injection from two phase 3 clinical trials. Curr Med Res Opin. 2017;33(6):1083–1090. | ||
Gopal S, Xu H, McQuarrie K, et al. Caregiver burden in schizophrenia following paliperidone palmitate long acting injectables treatment: pooled analysis of two double-blind randomized phase three studies. NPJ Schizophr. 2017;3(1):23. | ||
Joshi K, Lafeuille MH, Brown B, et al. Baseline characteristics and treatment patterns of patients with schizophrenia initiated on once-every-three-months paliperidone palmitate in a real-world setting. Curr Med Res Opin. 2017;33(10):1763–1772. | ||
Katz EG, Hauber B, Gopal S, et al. Physician and patient benefit-risk preferences from two randomized long-acting injectable antipsychotic trials. Patient Prefer Adherence. 2016;10:2127–2139. | ||
Savitz AJ, Xu H, Gopal S, et al. Efficacy and safety of paliperidone palmitate 3-month formulation for patients with schizophrenia: a randomized, multicenter, double-blind, noninferiority study. Int J Neuropsychopharmacol. 2016;19(7):pyw018. | ||
Utrecht U. European Long-acting Antipsychotics in Schizophrenia Trial (EULAST). Available from: https://clinicaltrials.gov/ct2/show/NCT02146547. Accessed November 06, 2018. | ||
Janssen Scientific Affairs L. A study to compare disease progression and modification following treatment with paliperidone palmitate long-acting injection or oral antipsychotics in participant’s with recent-onset schizophrenia or schizophreniform (DREaM). 2018. Available from: https://clinicaltrials.gov/ct2/show/NCT02431702. Accessed November 06, 2018. | ||
Janssen Research & Development, LLC. A Study of Paliperidone Palmitate 6-Month Formulation. 2018. Available from: https://clinicaltrials.gov/ct2/show/NCT03345342. Accessed November 06, 2018. | ||
Red Book Online. Truven Health Analytics. Available from: https://truvenhealth.com/Training/Product/IBM-Micromedex-Clinical-Knowledge/IBM-Micromedex-RED-BOOK. Accessed November 1, 2017. | ||
Einarson TR, Bereza BG, Tedouri F, van Impe K, Denee TR, Dries PJT. Cost-effectiveness of 3-month paliperidone therapy for chronic schizophrenia in the Netherlands. J Med Econ. 2017;20(11):1187–1199. | ||
Einarson TR, Bereza BG, Llinares GI, Gonzalez Martin Moro B, Tedouri F, Van Impe K. Cost-effectiveness of 3-month paliperidone treatment for chronic schizophrenia in Spain. J Med Econ. 2017;20(10):1039–1047. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
