Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Role of inspiratory capacity on dyspnea evaluation in COPD with or without emphysematous lesions: a pilot study
Authors Cui L , Ji X, Xie M , Dou S , Wang W , Xiao W
Received 17 May 2017
Accepted for publication 1 August 2017
Published 30 September 2017 Volume 2017:12 Pages 2823—2830
DOI https://doi.org/10.2147/COPD.S142016
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Liwei Cui,1 Xiuli Ji,2 Mengshuang Xie,1 Shuang Dou,1 Wei Wang,1 Wei Xiao1
1Department of Respiratory Disease, Qilu Hospital, Shandong University, 2Department of Pulmonary Disease, Jinan Traditional Chinese Medicine Hospital, Jinan, People’s Republic of China
Background: Since forced expiratory volume in 1 second (FEV1) shows a weak correlation with patients’ symptoms in COPD, some volume parameters may better reflect the change in dyspnea symptoms after treatment. In this article, we investigated the role of inspiratory capacity (IC) on dyspnea evaluation among COPD patients with or without emphysematous lesions.
Methods: In this prospective study, 124 patients with stable COPD were recruited. During the baseline visit, patients performed pulmonary function tests and dyspnea evaluation using the modified Medical Research Council (mMRC) scale. Partial patients underwent quantitative computerized tomography scans under physicians’ recommendations, and emphysematous changes were assessed using the emphysema index (EI; low attenuation area [LAA]% −950). These subjects were then divided into the emphysema-predominant group (LAA% −950≥9.9%) and the non-emphysema-predominant group (LAA% −950<9.9%). After treatment for ~1 month, subjects returned for reevaluation of both pulmonary function parameters and dyspnea severity. Correlation analysis between the change in IC (∆IC) and dyspnea (∆mMRC) was performed.
Results: Correlation analysis revealed that ∆IC was negatively correlated with ∆mMRC (correlation coefficient [cc], −0.490, P<0.001) in the total study population, which was stronger than that between ∆FEV1 and ∆mMRC (cc, −0.305, P=0.001). Patients with absolute ∆mMRC >1 were more likely to exhibit a marked increase in IC (≥300 mL) than those with absolute ∆mMRC ≤1 (74.36% versus 35.29%; odds ratio [OR], 5.317; P<0.001). In the emphysema-predominant group, only ∆IC strongly correlated with ∆mMRC (cc, −0.459, P=0.005), while ∆FEV1 did not (P>0.05).
Conclusion: IC could serve as an effective complement to FEV1 in COPD patients undergoing dyspnea evaluation after treatment. For COPD patients with predominant emphysematous lesions, an increase in IC is particularly more suitable for explaining dyspnea relief than FEV1.
Keywords: IC, COPD, mMRC score, quantitative computerized tomography, emphysema index
Introduction
COPD, as a common preventable and treatable disease, is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities caused by a significant exposure to noxious particles or gases.1 For patients with COPD, precise evaluation of symptom severity and treatment efficacy is closely linked to the patient’s confidence in the treatment and physicians’ considerations for further therapy options.2–4
Dyspnea, the hallmark complaint of patients with COPD, correlates with exercise intolerance and declining life quality.5 Persistent activity-related dyspnea often obliges patients to adopt a sedentary lifestyle, which further erodes the perceived quality of life. Frequent exacerbation of dyspnea, on the other hand, which forces patients to seek help from physicians and hospitals, is an independent predictor of a poor prognosis.6 Therefore, dyspnea relief and precise assessment play crucial roles in daily management of stable COPD patients.
A simple measure of dyspnea severity by the modified Medical Research Council (mMRC) scale is considered an adequate and convenient tool for daily assessment of COPD patients, which is well related to patients’ health status7 and future mortality risk.8,9 In addition, the mMRC score has been shown to have good correlation with declining lung function and other evaluation systems, such as the Chronic Respiratory Disease Questionnaire (CRQ) and the St George’s Respiratory Questionnaire (SGRQ) in a previous longitudinal study.10
Historically, forced expiratory volume in 1 second (FEV1) has been the “gold standard” for diagnosis and severity assessment of airflow limitation. However, some issues with its efficacy have remained, namely, that some patients with severe airflow limitation conduct nearly normal daily activities, and FEV1 sometimes shows no obvious improvement despite dyspnea being significantly alleviated. This coincides with the statement from the Global Initiative for Chronic Obstructive Lung Disease (GOLD) that FEV1 shows quite a weak correlation with symptom severity in COPD patients.1 Therefore, in this article, we have focused on other objective parameters that might be well correlated with subjective dyspnea evaluation and then might serve as a complement to FEV1 for more precise assessment of COPD.
In this work, we verified the efficiency of the volume parameter inspiratory capacity (IC) to evaluate dyspnea relief for ~1 month. This composite parameter may indirectly reflect the severity of lung hyperinflation, which represents the fundamental origin of dyspnea development.10,11
As a heterogenic disease, airflow limitation in COPD develops as a co-effect of both airway narrowing and destruction of lung elastic recoil, and the latter may display more severe gas trapping during hard expiration. Quantitative computerized tomography (QCT) provides a new approach for COPD subtyping by calculating the emphysema index (EI), which is the percentage of voxels with low attenuation, ie, <−950 Hounsfield units (Hu).12 Patients with or without marked emphysematous lesions may display distinct clinical characteristics and treatment responses. A study showed that QCT measures of emphysema were more likely to be associated with dyspnea severity, while complaints such as coughing and phlegm might relate to airway disease.13 This proposed a question of whether emphysematous changes may influence the application value of IC during dyspnea relief.
The aims of this study were to investigate the role of IC when evaluating dyspnea relief among total COPD subjects and then to compare the possible, different applications of IC in patients with different emphysematous phenotypes.
Methods
Subject population
Subjects eligible for inclusion in this prospective clinical study were patients aged >40 years who were diagnosed with COPD. All the subjects were in a stable state, with no exacerbation history for the recent 6 weeks prior to their entry into the study. All the subjects were enrolled between January 2015 and May 2017 in Qilu Hospital, Shandong University, People’s Republic of China. Subjects with a definite diagnosis of asthma or interstitial lung disease were excluded from the present study. Other exclusion criteria included thoracic pleural disease, bronchiectasis, or a computerized tomography (CT) mass with a diameter >3 cm.
This research was approved by the Human Research Ethics Committees of Qilu Hospital, Shandong University, People’s Republic of China (No 2015091). The study information was provided to subjects verbally prior to enrollment, and then informed consent was obtained in writing from each subject.
Study design
During baseline registration, individual information and medical history were collected. Dyspnea severity was evaluated through the mMRC scale. Pulmonary function tests were performed and interpreted for all subjects by experienced technicians, according to the requests of the American Thoracic Society/European Respiratory Society (ATS/ERS) statement.14 Subjects with the following conditions were recommended by the respiratory physicians to complete QCT scans: 1) subjects who did not complete any imaging examination, such as chest X-rays or chest CT scans, prior to the enrollment and 2) subjects whose symptom evaluation did not match the pulmonary function impairment under a physician’s consideration, especially for those with a slight activity-related dyspnea but with a severe decline in FEV1. The necessity and benefits of the QCT check were explained to the patients before the check. After QCT scanning, the EI was calculated as the percentage of lung voxels with a CT attenuation value ≤−950 Hu (low attenuation area [LAA]% −950). According to the adopted cutoff value of 9.9%,15 subjects were further divided into an emphysema-predominant group (LAA% −950≥9.9%) and a non-emphysema-predominant group (LAA% −950<9.9%).
We offered no medical intervention with household treatments, which was directed by physicians after baseline enrollment. Conventional treatments included inhaled bronchodilators, such as a long-acting β2 receptor agonist (LABA; eg, formoterol and salmeterol), a long-acting muscarinic antagonist (LAMA; eg, tiotropium bromide), and an inhaled corticosteroid (ICS; eg, budesonide), as well as systemic medicines, including theophylline. No systematic corticosteroids or antibiotics were given to these patients. Regular phonic follow-ups were made to supervise the patients’ compliance to treatment. After ~1 month, patients were called in for reexamination. Pulmonary function tests were conducted, while dyspnea severity was assessed by investigators who coordinated follow-up and were blind to previous assessment results and CT phenotypes.
Patients who experienced exacerbation, missed to follow-up, or changed the initial therapy for personal reasons during the treatment were eliminated from this study.
Assessment of dyspnea severity
Patients in this study were questioned regarding their degree of dyspnea symptoms by utilizing the mMRC dyspnea scale. The baseline and second tests were performed by different investigators, avoiding any implicating words during the investigation. The dyspnea severity was then scored on a scale from 0 to 4. According to the change in the mMRC score after treatment, subjects in this study were divided into a dyspnea obvious-remission group (absolute value of ΔmMRC score >1) and a non-remission group (absolute value of ΔmMRC score ≤1).
Pulmonary function tests
Pulmonary function tests were performed by experienced technicians at the baseline and second visits. Parameters were measured with instruments, including a spirometer and a diffusion device (MasterScreen; Jaeger, Wurzburg, Germany). The observed parameters included IC, FEV1, vital capacity (VC), forced vital capacity (FVC), total lung capacity (TLC), residual volume (RV), diffusing capacity of the lungs for carbon monoxide (DLCO), and diffusing capacity divided by the alveolar volume (DLCO/VA). Changes in parameters were calculated and presented as the Δ parameter.
QCT scan
Subjects who followed the recommendation of the physicians underwent chest CT scans performed at full inspiration stage. The scan was conducted with a 64-multidetector helical CT scanner (Philips Brilliance, Amsterdam, the Netherlands). Tube voltage of the scanner was 120 kV, and tube current was varied by automatic regulation in the range of 20–500 mA. Exposure time was 0.5 seconds, and image reconstruction was built in 1 mm – thick slices using a standard algorithm. LAAs were analyzed using a Airway Inspector CT Slicer software (Surgical Planning Laboratory at Brigham and Women’s Hospital, Boston, MA, USA). EI was calculated as the percentage of lung voxels with a CT attenuation value ≤−950 Hu, presented as LAA% −950. Based on the EI value, these subjects were then divided into an emphysema-predominant group (LAA% −950≥9.9%) and a non-emphysema-predominant group (LAA% −950<9.9%).
Statistical analysis
Data in this study were analyzed with SPSS 19.0 software (IBM Corporation, Armonk, NY, USA). Quantitative variables were presented as mean ± standard deviation (SD), and categorical variables were mainly shown as percentages (%). A paired t-test was utilized for comparison of clinical characteristics of subjects between the baseline and second visits. An independent sample t-test was applied on quantitative variables between the obvious-remission and non-remission groups and between the emphysema-predominant and non-emphysema-predominant groups. Categorical variables were analyzed via a chi-squared test. Correlations were verified by Pearson correlation coefficient (cc) analysis, while odds ratio (OR) and model fitting were calculated using a regression model. A P-value of <0.05 was considered as statistically different.
Results
Subject characteristics at baseline and second visits
A total of 124 stable COPD patients were enrolled in this study. The median interval between the first and second visits was 30.5 days. Mean age of these subjects was 62.08±8.36 years. Mean IC pretreatment was 2.08±0.63 L, which increased by ~300 mL after the treatment period. Apart from this, FEV1 and mMRC scores also changed significantly (P<0.001). Comparison of subjects’ clinical characteristics between the baseline and second visits is shown in Table 1.
Association between the changes in mMRC scores and the changes in IC and FEV1
Correlation analysis between the changes in mMRC scores and the changes in lung function parameters showed that ΔIC was negatively correlated with the ΔmMRC score (cc, −0.490, P<0.001). Although still significant, this association was weaker between ΔFEV1 and ΔmMRC (cc, −0.305, P=0.001). Detailed correlation analysis is shown in Table 2.
Comparison of clinical characteristics between subjects with dyspnea obvious remission and non-remission
According to the changes in mMRC scores after treatment, subjects were divided into a dyspnea obvious-remission group (absolute value of ΔmMRC >1) and a non-remission group (absolute value of ΔmMRC ≤1). Comparison of the clinical characteristics between the two subgroups showed no significant difference between GOLD grades and emphysema subtypes (P>0.05). However, subjects in the obvious-remission group showed a significant increase in IC and FEV1 compared to those in the non-remission group (P<0.001; Table 3). Since both IC and FEV1 increased by ~300 mL after treatment, we further set 300 mL as a cutoff value for grouping. A higher percentage of subjects in the obvious-remission group showed a significant increase in IC (ΔIC ≥300 mL) compared to the non-remission group (74.36% versus 35.29%; OR, 5.317; 95% CI, 2.28–12.38; P<0.001). Moreover, more subjects in the obvious-remission group showed a significant increase in IC (ΔIC ≥300 mL) than an increase in FEV1 (ΔFEV1 ≥300 mL; 74.36% versus 51.28%).
Comparison of characteristics between the emphysema-predominant group and the non-emphysema-predominant group
According to the value of LAA% −950, 70 COPD subjects who performed QCT scans were divided into an emphysema-predominant group (LAA% −950≥9.9%, n=36) and a non-emphysema-predominant group (LAA% −950<9.9%, n=34), as previously described. Subjects in the emphysema-predominant group show a higher mMRC score (2.39±0.77 versus 1.68±0.73, P<0.001) and a higher EI (21.10±10.08 versus 3.99±2.94, P<0.001). Comparisons of clinical characteristics of the two groups are shown in Table 4.
Role of IC and FEV1 applied to dyspnea evaluation in different COPD emphysematous phenotypes
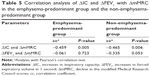
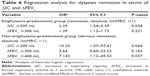
In this study, we investigated the role of IC and FEV1 dyspnea evaluation in different COPD subtypes. As shown in Table 5, ΔIC was negatively correlated with ΔmMRC scores in the non-emphysema-predominant group (cc, −0.465, P=0.006), while cc of ΔFEV1 and ΔmMRC scores was −0.335 (P=0.053). In the emphysema-predominant group, only ΔIC was negatively correlated with ΔmMRC scores (cc, −0.459, P=0.005), while ΔFEV1 was not (P=0.723). Further logistic regression model was utilized to analyze the relationship between dyspnea outcomes and improvements in IC and FEV1 in two groups separately. In the emphysema-predominant group, only ΔIC predicted the degree of dyspnea relief (R=0.459, P=0.005), while FEV1 did not (P>0.05). For the non-emphysema-predominant group, no effective logistic regression model to predict the changes in mMRC scores was built in terms of ΔIC and ΔFEV1 (P>0.05). However, a regression analysis revealed that subjects with a significant increase in IC (ΔIC ≥300 mL) tended to achieve obvious dyspnea relief (absolute ΔmMRC >1; OR, 10.20; 95% CI, 1.07–97.41; P=0.021). Apart from this, the significant increase in FEV1 (ΔFEV1 ≥400 mL) may also predict dyspnea relief to some degree in the non-emphysema-predominant group (OR, 7.14; 95% CI, 1.12–45.52; P=0.025). Results of regression analysis are shown in Table 6.
Discussion
The increase in IC showed a better correlation with the decline in mMRC scores than FEV1 did in the total COPD population. Moreover, patients with obvious dyspnea relief tended to display a significant IC increase compared to patients whose symptoms showed hardly any improvement. As to the different COPD emphysematous phenotypes, increases in both IC and FEV1 might negatively correlate with the decline in mMRC scores in the non-emphysema-predominant group. However, only the increase in IC could be used to specifically assess the relief of dyspnea in patients with predominant emphysematous lesions.
We tried to elucidate two points in this study. The first is that the volume parameter IC may serve as an effective complement to FEV1 in dyspnea evaluation during COPD daily management and assessment. As is known, FEV1 is widely used as a major criterion for judging and grading the severity of the expiratory flow limitation (EFL) in COPD patients.1 Despite the close correlation between the progressive decline in FEV1 and the mortality of patients, a number of studies5,16,17 have demonstrated rather weak correlations between FEV1 and symptom severity, especially for exertional dyspnea and exercise intolerance. In this study, a relatively weaker correlation was shown between an increase in FEV1 and a decline in mMRC score. This may be partially explained by the fact that the subjects selected in this study were distributed from GOLD I to IV, and the higher proportion of subjects with severe airflow limitation (GOLD IV) may have brought about this unexpected cc.
To explore the mechanism, the dyspnea symptom of COPD patients mainly results from the uncoupling between limited tidal volume (VT) expansion and increasing ventilation demand during exercise.18 This uncoupling is one of the intuitive manifestations of the EFL, and the latter represents the principal function disorder of COPD.19 The underlying pathogenesis is that EFL further promotes the development of dynamic hyperinflation (DH). DH forces patients to breathe at a high end-expiratory lung volume level, which is affected by both a faint breathing drive (mainly by recoil destruction) and airway construction (mainly by airway remodeling).16 During exercise, VT expansion is greatly restricted and thus reaches an inflection point or plateau earlier than in healthy subjects. To interpret the uncoupling during dyspnea development, it is key to find a parameter that fully reflects the change in DH. Since DH has more volume expansion than flow disorder, IC showed more advantages over FEV1 in terms of dyspnea evaluation. Compared to volume parameters, such as TLC and RV, obtained by a single-breath diffusion test or body plethysmograph, the measurement of IC can be obtained through a spirometer, which is simpler, is cost-effective, and has a low demand for technical requirements and patient cooperation. This means, for primary hospitals or clinics, simple detection of IC may well explain the obvious improvement in dyspnea symptoms of patients after treatment, despite almost no change in FEV1 in some instances.
Several previous studies have focused on the application of IC during clinical practice. Manriquez et al20 compared the proportion of 50 stable COPD patients whose FEV1 and IC improved by >10% after inhaling 200 mg of salbutamol. In a display of transient efficacy, only 13 patients (26%) showed FEV1 improvement in excess of 10%, while 40 patients (80%) displayed an obvious IC increase. Ramon et al21 investigated the relationship between the ratio of IC to TLC and the decline in exercise capacity among COPD patients and suggested that patients with a lower IC/TLC ratio had a greater decline in 6-minute walk distance (6MWD) decline. In the present study, no significant correlation was found between ΔIC/TLC and declining mMRC scores; one possible reason for this may be that the volume measurements in this study were mainly obtained through diffusion tests of one single breath. This method might sometimes severely underestimate the actual lung volume, thus affecting the correlation analysis results.
The second point we wanted to elucidate is that the increase in IC may be particularly more suitable for interpreting dyspnea relief in COPD patients with an emphysema-predominant CT indication. As a heterogenic disease, patients of different COPD subtypes may display distinct clinical characteristics and therapeutic responses.22–24 COPD heterogeneity depends mostly on different pathological and physiological impairments, such as airway remodeling, emphysematous lung destruction, or some other specific features.
Since QCT is a promising technique for the diagnosis and severity assessment of COPD, different CT phenotypes may exhibit distinct characteristics and bronchodilator responses. Hersh et al25 compared clinical features between emphysema-predominant COPD and non-emphysematous COPD in a multicenter clinical study. It showed that patients in the emphysema-predominant group underwent more severe airflow obstruction, greater exercise limitation, and reduced quality of life, while non-emphysematous patients were more frequent to be diagnosed with diabetes. Moreover, CT quantitative analysis showed a strong correlation with COPD candidate gene in which CTGA diplotype was closely associated with emphysematous phenotype.26 In this study, we divided the subjects according to emphysema severity.27,28 The measure of emphysema, executed by calculating the percentage of voxels with the CT attenuation value ≤−950 Hu, exhibits a good correlation with visual emphysema assessment and pathologic morphology.29–31 Our previous study15 showed that the measure of EI (LAA% −950) among normal subjects was 2.79%±2.37%, and LAA% −950 exceeding 9.9% may suggest evidence of obvious emphysema. Fewer studies have focused on the role of IC in the evaluation of dyspnea relief in different COPD subtypes.
In patients with no obvious change in emphysema, increase in both IC and FEV1 may be possible to explain the relief of dyspnea, and the role of FEV1 is doubted. This may depend on the fact that airway obstruction may be dominant rather than severe recoil destruction among these patients. The decline in FEV1 represents the severity of airflow limitation, and the detection of it may be affected by both emphysema severity and airway obstruction. However, for patients of the emphysema-predominant subtype, airflow limitation develops mainly on the basis of parenchyma destruction. This pathogenic change thus results in severe hyperinflation and air trapping. Therefore, volume changes may be more sensitive and could reliably reflect the relief of dyspnea symptoms. This point is also verified by regression model that a significant increase in IC may predict the remission of activity-related dyspnea. Taken together with factors including age, sex, nutrition status, smoking history, and pulmonary function parameters, an increase in IC alone may serve as a linear predictor for the degree of dyspnea relief.
Limitations
There are several limitations in this study. First, as a single-center pilot study, the limited cohort size may affect the correlation analysis results, despite the association between IC and dyspnea showed in this article The limited cohort size also affected the efficacy of regression model for predicting dyspnea remission in terms of ΔIC and FEV1. Therefore, an enlarged cohort study was necessary to better elucidate the conclusions. Second, mMRC scores were utilized as the only measure of symptom evaluation in this study. Different investigators, who were blinded to the previous evaluating scores, assessed the severity of dyspnea during the baseline and second visits. However, different questioning methods may still affect the accuracy of mMRC scores. For further study, a more comprehensive evaluation system, such as COPD Assessment Test (CAT) or SGRQ, needs to be used. Finally, lung volume measures in this study were mainly obtained via diffusion tests of one single breath; this may somewhat underestimate the actual lung volume values and changes. IC is a composite parameter that is easily interfered by breathing patterns during the check. Despite strict quality control, a larger sample size may be helpful to improve accuracy. Besides, a study focusing on volume changes determined by body plethysmography is also needed.
Conclusion
IC could serve as an effective complement to FEV1 in COPD patients for dyspnea evaluation during a stable period of treatment. For COPD patients with predominant emphysematous lesions, an increase in IC is particularly more suitable for explaining dyspnea relief than that in FEV1.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grant No 81370148). We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Disclosure
The authors report that no potential conflicts of interest exist with any companies or organizations whose products or services are discussed in this article.
References
Global Initiative for Chronic Obstructive Lung Disease (GOLD) [homepage on the Internet]. Global Strategy for the Diagnosis, Management and Prevention of COPD. 2017. Available from: http://www.goldcopd.org/. Accessed January 13, 2017. | ||
van der Molen T, Miravitlles M, Kocks JW. COPD management: role of symptom assessment in routine clinical practice. Int J Chron Obstruct Pulmon Dis. 2013;8:461–471. | ||
Calverley PM, Postma DS, Anzueto AR, et al. Early response to inhaled bronchodilators and corticosteroids as a predictor of 12-month treatment responder status and COPD exacerbations. Int J Chron Obstruct Pulmon Dis. 2016;11:381–390. | ||
Eckerblad J, Tödt K, Jakobsson P, et al. Symptom burden in stable COPD patients with moderate or severe airflow limitation. Heart Lung. 2014;43(4):351–357. | ||
O’Donnell DE, Travers J, Webb KA, et al. Reliability of ventilatory parameters during cycle ergometry in multicentre trials in COPD. Eur Respir J. 2009;34(4):866–874. | ||
Ora J, Jensen D, O’Donnell DE. Exertional dyspnea in chronic obstructive pulmonary disease: mechanisms and treatment approaches. Curr Opin Pulm Med. 2010;16(2):144–149. | ||
Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. | ||
Sundh J, Janson C, Lisspers K, Ställberg B, Montgomery S. The dyspnoea, obstruction, smoking, exacerbation (DOSE) index is predictive of mortality in COPD. Prim Care Respir J. 2012;21(3):295–301. | ||
Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002;121(5):1434–1440. | ||
Oga T, Tsukino M, Hajiro T, Ikeda A, Nishimura K. Analysis of longitudinal changes in dyspnea of patients with chronic obstructive pulmonary disease: an observational study. Respir Res. 2012;13(1):85. | ||
Frisk B, Hardie JA, Espehaug B, et al. Peak oxygen uptake and breathing pattern in COPD patients – a four-year longitudinal study. BMC Pulm Med. 2015;15:93–104. | ||
Madani A, Zanen J, de Maertelaer V, et al. Pulmonary emphysema: objective quantification at multi-detector row CT – comparison with macroscopic and microscopic morphometry. Radiology. 2006;238(3):1036–1043. | ||
Grydeland TB, Dirksen A, Coxson HO, et al. Quantitative computed tomography measures of emphysema and airway wall thickness are related to respiratory symptoms. Am J Respir Crit Care Med. 2010;181(4):353–359. | ||
Pellegrino R, Viegi G, Enright P, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26:948–968. | ||
Xie M, Wang W, Dou S, Cui L, Xiao W. Quantitative computed tomography measurements of emphysema for diagnosing asthma-chronic obstructive pulmonary disease overlap syndrome. Int J Chron Obstruct Pulmon Dis. 2016;11:953–961. | ||
Guenette JA, Webb KA, O’Donnell DE. Does dynamic hyperinflation contribute to dyspnoea during exercise in patients with COPD? Eur Respir J. 2012;40(2):322–329. | ||
O’Donnell DE, Guenette JA, Maltais F, Webb KA. Decline of resting inspiratory capacity in COPD: the impact on breathing pattern, dyspnea, and ventilatory capacity during exercise. Chest. 2012;141(3):753–762. | ||
Chen R, Chen R, Chen X, Chen L. Effect of endurance training on expiratory flow limitation and dynamic hyperinflation in patients with stable chronic obstructive pulmonary disease. Intern Med J. 2014;44(8):791–800. | ||
Tantucci C. Expiratory flow limitation definition, mechanisms, methods, and significance. Pulm Med. 2013;2013:749860. | ||
Manriquez J, Diaz O, Borzone G, et al. Spirometric reversibility to salbutamol in chronic obstructive pulmonary disease (COPD). Differential effects on FEV1 and on lung volumes. Rev Med Chil. 2004;132(7):787–793. | ||
Ramon MA, Ferrer J, Gimeno-Santos E, et al. Inspiratory capacity-to-total lung capacity ratio and dyspnoea predict exercise capacity decline in COPD. Respirology. 2016;21(3):476–482. | ||
Camiciottoli G, Bigazzi F, Bartolucci M, et al. BODE-index, modified BODE-index and ADO-score in chronic obstructive pulmonary disease: relationship with COPD phenotypes and CT lung density changes. COPD. 2012;9(3):297–304. | ||
Fens N, van Rossum AG, Zanen P, et al. Subphenotypes of mild-to-moderate COPD by factor and cluster analysis of pulmonary function, CT imaging and breathomics in a population-based survey. COPD. 2013;10(3):277–285. | ||
Camiciottoli G, Diciotti S, Bigazzi F, et al. Is intrathoracic tracheal collapsibility correlated to clinical phenotypes and sex in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:843–852. | ||
Hersh CP, Make BJ, Lynch DA, et al. Non-emphysematous chronic obstructive pulmonary disease is associated with diabetes mellitus. BMC Pulm Med. 2014;14:164. | ||
Choo JY, Lee KY, Shin C, et al. Quantitative analysis of lungs and airways with CT in subjects with the chronic obstructive pulmonary disease (COPD) candidate FAM13A gene: case control study for CT quantification in COPD risk gene. J Comput Assist Tomogr. 2014;38(4):597–603. | ||
Bafadhel M, Umar I, Gupta S, et al. The role of CT scanning in multidimensional phenotyping of COPD. Chest. 2011;140(3):634–642. | ||
Diaz AA, Bartholmai B, San José Estépar R, et al. Relationship of emphysema and airway disease assessed by CT to exercise capacity in COPD. Respir Med. 2010;104(8):1145–1151. | ||
Van Tho N, Wada H, Ogawa E, Nakano Y. Recent findings in chronic obstructive pulmonary disease by using quantitative computed tomography. Respir Investig. 2012;50(3):78–87. | ||
Gierada DS, Yusen RD, Pilgram TK, et al. Repeatability of quantitative CT indexes of emphysema in patients evaluated for lung volume reduction surgery. Radiology. 2001;220(2):448–454. | ||
Bakker ME, Stolk J, Putter H, et al. Variability in densitometric assessment of pulmonary emphysema with computed tomography. Invest Radiol. 2005;40(12):777–783. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.