Back to Journals » OncoTargets and Therapy » Volume 11
Role of chemotherapy with epidermal growth factor receptor-tyrosine kinase inhibitor (EGFR-TKI ) rechallenge in small cell transformation after EGFR-TKI failure: a case report
Authors Lee S , Joo JH , Kwak MA, Sohn K, Chon SH
Received 6 February 2018
Accepted for publication 15 May 2018
Published 9 July 2018 Volume 2018:11 Pages 3943—3947
DOI https://doi.org/10.2147/OTT.S164764
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Takuya Aoki
Sanghun Lee,1 Jeonghyun Joo,2 Minah Kwak,3 Kicheul Sohn,4 Songha Chon5
1Department of Medical Consilience, Graduate School, Dankook University, Yongin, Republic of Korea; 2Department of Korean Internal Medicine, Comprehensive and Integrative Medicine Hospital, Daegu, Republic of Korea; 3Department of Internal Medicine, College of Korean Medicine, Daegu Haany University, Daegu, Republic of Korea; 4Department of Preventive Medicine, Daegu Catholic University Medical Center, Daegu, Republic of Korea; 5Department of Hemato-Oncology, Comprehensive and Integrative Medicine Hospital, Daegu, Republic of Korea
Background: Small cell lung cancer (SCLC) transformation is one of the resistance mechanisms associated with epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs). Rechallenge with the first-line TKI after the second-line chemotherapy is suggested as a salvage treatment despite modest efficacy.
Case presentation: Here, we report the case of a 72-year-old, never-smoker female diagnosed with multiple metastatic lung adenocarcinoma (cT2aN2M1) harboring EGFR mutations in exon 21 (L858R) of the primary lesion. Despite subsequent treatment with gefitinib for more than a year, the patient developed resistance to the drug. Histological analysis based on rebiopsy at subphrenic mass revealed small cell transformation. After a partial response to irinotecan and carboplatin, the metastatic subphrenic and liver masses presented dramatic progression despite another round of cytotoxic chemotherapy. Rechallenge with erlotinib based on the original EGFR mutation (L858R) without small cell transformation confirmed by re-biopsy of hepatic mass lesions elicited only mixed response. Therefore, cytotoxic chemotherapy comprising irinotecan and carboplatin combined with erlotinib was effective against all the metastatic lesions.
Conclusion: To the best of our knowledge, this is the first case of concurrent retreatments with TKIs and chemotherapy previously effective in SCLC transformation.
Keywords: small cell transformation, epidermal growth factor receptor, tyrosine kinase inhibitors, chemotherapy, salvage treatment
Introduction
Lung cancer is the leading cause of cancer death worldwide. Approximately two-thirds of non-small cell lung cancer (NSCLC) patients, constituting 75%–80% of all lung cancers, present with locally advanced or metastatic disease, with a 5-year survival rate of <5%.1 In the past decade, various tyrosine kinase inhibitor (TKI) therapies showed dramatic and durable clinical benefit against distinct somatic molecular aberrations in tumor genes associated with epidermal growth factor receptor (EGFR), prevalent in up to 60% of the Asian population.2 Nevertheless, clinically apparent acquired resistance to TKIs develop within 1 year from the start of treatment in the vast majority of initial responders.3 Although a second-site EGFR mutation substituting threonine for methionine at position 790 in exon 20 (T790M) is prevalent in more than 50% of cases,4 the mechanisms responsible for resistance are complex and heterogeneous, such as HER2 amplification/mutations and cMET amplification.5,6 Histological changes including small cell lung cancer (SCLC) transformation and epithelial-to-mesenchymal transition have also been detected.7
The subsequent rechallenge with the first-line TKI after the second-line chemotherapy provided clinical benefit because recrudescence of sparing TKI-sensitive clones leads to progressive disease.8,9 However, the clinical outcome falls short of expectations. The present study highlights the advantages of combination of rechallenge with chemotherapy as well as first-line TKIs in cases of tumor heterogeneity of acquired resistance following first-line EGFR-TKI treatment failure. To the best of our knowledge, this is the first case of concurrent rechallenge of TKIs and conventional chemotherapy previously effective in SCLC transformation.
Case report
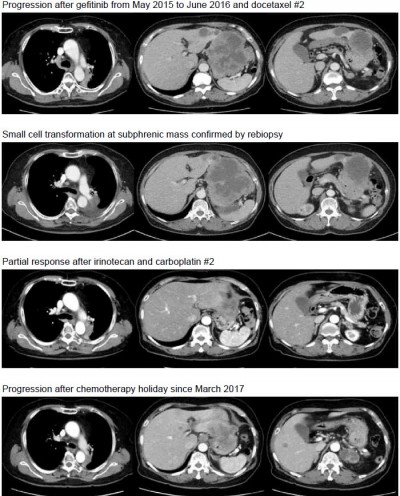
In January 2015, a 72-year-old female with no history of smoking received a medical examination due to persistent cough. Multiple metastatic lung cancer (cT2aN2M1) was diagnosed by computed tomography and positron emission tomography. Histological examination of the bronchoscopic biopsy revealed a moderately differentiated adenocarcinoma, which was confirmed immunohistochemically (IHC) based on strong nuclear expression of thyroid transcription factor 1 (TTF-1). Both IHC-based and sequencing assays indicated an EGFR mutation in exon 21 (L858R) and negative results for EML4-ALK and ROS1. The patient subsequently underwent gamma knife radiosurgery for brain metastases and radiation to the primary lung lesions. In March 2015, the patient started treatment with the TKI inhibitor gefitinib (250 mg/day orally for 15 months). However, by June 2016, disease progression was observed. Histological analysis based on re-biopsy from progressive subphrenic mass revealed small cell transformation and tested positive with TTF-1 (+), CD56 (+), and synaptophysin (+) (Figure 1). The tumor was refractory to two cycles of cytotoxic chemotherapy and docetaxel (Figure 2). However, a partial response was observed during the seven cycles of irinotecan and carboplatin regimen in March 2017. After cessation of chemotherapy, her disease progressed in July 2017 (Figure 2). The metastatic subphrenic and liver masses presented dramatic progression despite subsequent cytotoxic chemotherapy with pemetrexed or etoposide/carboplatin from July to September 2017 (Figure 3). Re-biopsy of hepatic mass lesions revealed the original EGFR mutations in exon 21 (L858R) without small cell transformation and programmed death-ligand 1 (PD-L1) expression. Therefore, rechallenge with the first-line TKI, erlotinib (150 mg/day), was decided rather than second-generation TKI, afatinib, due to the high costs. Erlotinib treatment for 4 weeks showed mixed response including a partial response by the liver masses and progression of subphrenic and adrenal gland metastases, which suggested coexistence of small cell transformation. Therefore, erlotinib combined with the cytotoxic chemotherapy of irinotecan and carboplatin previously effective yielded a favorable response in all the metastatic lesions in November 2017 (Figure 3). No significant adverse effects were observed with the combination chemotherapy.
  | Figure 2 Computed tomography (CT) images showing treatment-related changes. |
  | Figure 3 Computed tomography (CT) images showing differential response to single and combined therapies. |
Discussion
Lung cancer is classified into two histological subtypes: SCLC and NSCLC, including adenocarcinoma, squamous-cell carcinoma, and large-cell carcinoma, commonly believed to be different diseases with distinct biology and genomic abnormalities. The chemotherapy regimen varies according to the tumor type.10,11 Therefore, cisplatin or carboplatin combined with etoposide is most commonly used in SCLC, while various targeted TKIs are available for NSCLC. After the administration of EGFR TKIs in practice, SCLC transformation has been reported as one of the resistance mechanisms associated with first-generation EGFR TKIs in 10% of the cases.7 The prevalence and possible overlap of these mechanisms have yet to be elucidated. However, alveolar type II cells undergo transformation to both adenocarcinoma and SCLC depending on the mutational status of tumor suppressors and key oncogenes underlying the loss of RB1 and EGFR expression, respectively.12
After SCLC transformation, the overall survival rate was 7.1 months despite a high response rate observed with standard chemotherapy for SCLC.13 Subsequent rechallenge with the first-line TKIs in subjects who initially responded to the same TKIs was suggested as salvage treatment after progression of chemotherapy. However, it was reported to offer only modest activity with a median progression-free survival of 2.8 or 6.5 months following gefitinib or erlotinib treatment, respectively.8,9 The clinical efficacy of retreatment with only TKIs is limited, due to acquired resistance such as SCLC.14 Therefore, our case demonstrates the need for a treatment strategy targeting small cells and existing adenocarcinoma via readministration of first-line TKIs.
Conclusion
Our case for the first time indicates that rechallenge with the first-line TKIs combined with standard chemotherapy for SCLC is effective as a salvage treatment in selected patients with SCLC transformation in TKI-responsive adenocarcinoma.
Acknowledgments
We wish to thank the patient and family involved in this study for providing written informed consent for publication of this detailed case report and the accompanying images. This work was supported by a grant from the Comprehensive and Integrative Medicine R&D project through Comprehensive and Integrative Medicine Institute, funded by the Ministry of Health & Welfare, Republic of Korea (Grant Number: 090-091-3000-3038-301-320-01).
Disclosure
The authors report no conflicts of interest in this work.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. | ||
Li CG, Fang R, Sun YH, et al. Spectrum of oncogenic driver mutations in lung adenocarcinomas from East Asian never smokers. PLoS One. 2011;6(11):e28204. | ||
Jackman D, Pao W, Riely GJ, et al. Clinical definition of acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small-cell lung cancer. J Clin Oncol. 2010;28(2):357–360. | ||
Kobayashi S, Boggon TJ, Dayaram T, et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med. 2005;352(8):786–792. | ||
Bean J, Brennan C, Shih JY, et al. MET amplification occurs with or without T790M mutations in EGFR mutant lung tumors with acquired resistance to gefitinib or erlotinib. Proc Natl Acad Sci U S A. 2007;104(52):20932–20937. | ||
Takezawa K, Pirazzoli V, Arcila ME, et al. HER2 amplification: a potential mechanism of acquired resistance to EGFR inhibition in EGFR-mutant lung cancers that lack the second-site EGFRT790M mutation. Cancer Discov. 2012;2(10):922–933. | ||
Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3(75):75ra26. | ||
Becker A, Crombag L, Heideman DA, et al. Retreatment with erlotinib: regain of TKI sensitivity following a drug holiday for patients with NSCLC who initially responded to EGFR-TKI treatment. Eur J Cancer. 2011;47(17):2603–2606. | ||
Cappuzzo F, Morabito A, Normanno N, et al. Efficacy and safety of rechallenge treatment with gefitinib in patients with advanced non-small cell lung cancer. Lung Cancer. 2016;99:31–37. | ||
NSCLC Meta-Analyses Collaborative Group. Chemotherapy in addition to supportive care improves survival in advanced non-small-cell lung cancer: a systematic review and meta-analysis of individual patient data from 16 randomized controlled trials. J Clin Oncol. 2008;26(28):4617–4625. | ||
Murray N, Turrisi AT. A review of first-line treatment for small-cell lung cancer. J Thorac Oncol. 2006;1(3):270–278. | ||
Oser MG, Niederst MJ, Sequist LV, Engelman JA. Transformation from non-small-cell lung cancer to small-cell lung cancer: molecular drivers and cells of origin. Lancet Oncol. 2015;16(4):e165–e172. | ||
Jiang SY, Zhao J, Wang MZ, et al. Small-cell lung cancer transformation in patients with pulmonary adenocarcinoma: a case report and review of literature. Medicine. 2016;95(6):e2752. | ||
Nishimura J, Miyamoto Y, Fujimoto N, et al. Adenocarcinoma of the lung acquiring resistance to afatinib by transformation to small cell carcinoma: a case report. Case Rep Oncol. 2017;10(2):666–670. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

