Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 12
Role of 11β HSD 1, rs12086634, and rs846910 single-nucleotide polymorphisms in metabolic-related skin diseases: a clinical, biochemical, and genetic study
Authors Farag AGA , Badr EAE , Eltorgoman AMA, Assar MFA, Elshafey EN, Tayel NR, Aboutaleb HEA
Received 1 November 2018
Accepted for publication 18 December 2018
Published 23 January 2019 Volume 2019:12 Pages 91—102
DOI https://doi.org/10.2147/CCID.S193156
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Azza Gaber Antar Farag,1 Eman AE Badr,2 Abdel Monem A Eltorgoman,3 Mohamed FA Assar,4 Eman N Elshafey,1,4 Nermin Reda Tayel,5 Hossam EA Aboutaleb4
1Department of Dermatology, Andrology and STDs, Faculty of Medicine, Menoufia University, Shibin El Kom, Egypt; 2Department of Medical Biochemistry and Molecular Biology, Faculty of Medicine, Menoufia University, Shibin El Kom, Egypt; 3Department of Organic Chemistry, Faculty of Science, Menoufia University, Shibin El Kom, Egypt; 4Department of Chemistry, Biochemistry Division, Faculty of Science, Menoufia University, Shibin El Kom, Egypt; 5Department of Molecular Diagnostics and Therapeutics, Genetic Engineering Biotechnology Research Institute, Sadat City, Egypt
Background: 11β HSD1 generates cortisol from cortisone. 11β HSD1 single-nucleotide polymorphism (SNP) was associated with metabolic syndrome (MeTS). Although the relation of acne vulgaris (AV) and skin tags (STs) with MeTS has been reported, the relationship between 11β HSD 1 SNP and cortisol activity in those patients has not studied till now.
Aims: To investigate, two 11β-HSD1 SNPs (rs846910 and rs12086634), serum lipid profile and cortisol levels in patients with AV and STs in an Egyptian population.
Patients and methods: This case–control study was performed on 50 patients having STs and 50 complaining of AV and 50 sex- and age-matched controls. We searched for serum lipid profile, cortisol levels, and 11β-HSD1 rs846910 and rs12086634 SNPs using real time-PCR.
Results: Compared to controls,11β-HSD1 rs846910 GA genotype carriers had significantly higher risks for developing AV and STs by 3.4- and 4.9-fold, respectively, and its A allele increases these risks by 3.1 and 4.4 times, respectively. Also, 11β-HSD1 rs12086634 TG genotype increases the risk of AV by 3.2-fold, as well as STs by 3.5-fold, and its G allele increases the risk of AV by 3.2-fold and STs by 7-fold. In AV and ST patients, rs846910 GA genotype demonstrated significant associations with elevated body mass index (BMI), and cholesterol, low density lipoprotein (LDL), cortisol, and decreased high density lipoprotein serum levels, respectively. However, rs12086634 GG genotype was significantly associated with increased BMI, cholesterol, and LDL serum levels in patients with AV and STs, in addition to the number of STs and serum cortisol levels in ST patients.
Conclusion: 11β-HSD1 rs846910 and rs12086634 gene polymorphisms may contribute to AV and STs pathogenesis, that may be mediated through enhancing the enzymatic activity (increasing cortisol levels). AV and STs are associated with obesity and atherogenic lipid profile. Diagnosis of AV and STs may play a role in early detection of the MeTS.
Keywords: skin tags, acne vulgaris, metabolic syndrome, 11 beta hydroxysteroid dehydrogenase, single-nucleotide polymorphism
Introduction
Skin diseases are the most widespread human morbidities, affecting all populations. They were the 18th major reason of universal disability-adjusted life year in Global Burden of Disease 2013.1
Metabolic syndrome (MeTS) is diagnosed by the presence of three or more of the following criteria; increased waist circumference, high triglycerides, low high density lipoprotein (HDL) level, increased blood fasting glucose, and increased blood pressure. The most accepted theory for MeTS pathophysiology is insulin resistance. The increased body fat decreases the expression of insulin receptor substrate-1, leading to decreased insulin sensitivity. Consequently, the pancreas compensates by secreting larger quantities of insulin (hyper insulinemia). Individuals having MeTS seem to have increased prevalence of cardiovascular disease and type 2 diabetes mellitus.2
There is ongoing scientific interest regarding association of skin comorbidities with the MeTS, that ranges from severe diseases such as psoriasis to simple cosmetic problems like skin tags (STs) and includes the commonest ones such as acne vulgaris (AV).3
AV is one of the most common dermatological disorders. The prevalence of AV in adolescents ranges from 35 to over 90%.4 Acne develops within the pilosebaceous unit of the villous hair due to co-interaction between many factors including abnormal keratinization, excessive sebum secretion, and endocrinal factors.5
STs or acrochordons are common benign connective tissue neoplasms of the dermis that are mainly composed of loose fibrous tissue.6 They occur mainly on the neck and major flexures as small, soft protrusions.7 Histologically, STs formed of a polypoid show an acanthotic epidermis and a fibrous vascular kernel dermis.6
11β HSD 1 is a well-known cortisone reductase. It is highly expressed in major metabolic tissues including adipose tissue and liver. For local glucocorticoid action, 11β HSD 1 diminishes cortisone to its active form (cortisol) that stimulates glucocorticoid receptors.8 Cortisol is the major steroid hormone of the glucocorticoids. It is one of the most important hormones in regulation of different immunologic and metabolic processes.9 Cortisol has been linked to several morbidities including MeTS.10
The 11β HSD 1 gene is located on chromosome 1q32-q41.11 Many studies have demonstrated a pathogenic role for 11β HSD 1 gene in metabolic diseases and detected the positive associations of 11β HSD 1 polymorphisms with type 2 diabetes mellitus, insulin resistance, and MeTS.11–16
Although the relation of AV and STs to MeTS has been reported,3 the relationship between 11β HSD 1 single-nucleotide polymorphism (SNP) and cortisol activity in those patients has not yet been studied.
Therefore, we aimed in this study to investigate, for the first time, two 11β-HSD1 gene polymorphisms (rs846910 and rs12086634), serum lipid profile, and cortisol levels in patients with AV and STs and their characteristics in the Egyptian population.
Patients and methods
In this case–control study, we investigated 150 subjects divided into three equal groups: group I included patients with AV; group II included patients with STs; and group III included sex- and age-matched apparently healthy volunteers (control group). They were selected from Dermatology Outpatient Clinic – Menoufia University Hospital during the period from January 2018 to May 2018. The study protocol was approved by the ethical committee of Faculty of Medicine, Menoufia University that was in accordance with the Helsinki Declaration in 1975 (revised in 2000). A written informed consent was obtained from all participants prior to study initiation.
We included patients from both sexes. They were in stable living conditions and maintained a general diet for 2 weeks before joining the study, and were asked to avoid vigorous exercise before blood sampling. Subjects with diabetes mellitus, hepatic diseases, thyroid disorders, Cushing’s syndrome, and those who are either on treatment or had history of treatment with drugs that can influence serum cortisol level or lipid profile (glucocorticoids, insulin, oral hypoglycemic agents, systemic retinoids, and oral contraceptive pills) within the last 3 months were excluded. Additionally, we excluded pregnant and lactating women, and those having polycystic ovarian syndrome (PCOS).
Methods
Every subject was submitted to full history taking and clinical examinations. Weight and height measuring were assessed to calculate body mass index (BMI).17 Dermatological examination for STs and AV was done. Regarding STs; their site, size, and the total number (mild disease [STs number <10], moderate [10–30 STs], and severe [STs number >30]) were evaluated.18 Also, acne severity was addressed.19 The investigations were carried out in the Biochemistry Department, Faculty of Science and Medical Biochemistry & Molecular Biology Department, Faculty of Medicine, Menoufia University. Serum lipid profile and cortisol levels, and 11β HSD 1 rs12086634 and rs846910 SNP by real time-PCR were performed.
Blood sampling
Under complete aseptic conditions and after overnight fasting, 6 mL blood samples were withdrawn from each participant and separated into two parts, one for DNA extraction that was kept in an EDTA tube. The other part was put in a plain tube, left to clot for 30 minutes at room temperature, then underwent centrifugation for 10 minutes at 4,000 × g per minute and the serum obtained was divided into aliquots, stored at –80°C until the time for lipid profile and cortisol level analysis.
Assay methods
- Lipid profile: Quantitative estimation of total cholesterol (TC), HDL-cholesterol and triglycerides (TG) using the colorimetric enzymatic method, using standard enzymatic colorimetric kits (Spinreact diagnostics kit, Spain) and low density lipoprotein (LDL)-cholesterol was elaborated by modified Friedewald equation.20
- Cortisol level estimation: Serum cortisol was determined by ELISA, using a DetectX® Cortisol ELISA kit, USA.21
- SNP assay. After DNA extraction by Pure link genomic DNA extraction kits (USA), the DNA extract was used for SNP assay in a total reaction volume 20 μL with 10 μL of TaqMan Genotyping Master Mix, 1.25 μL of 20× TaqMan genotyping assay kits containing both primers and probes and nuclease-free water. By using the 7,500 Real-time PCR system (Applied Biosystems, Foster City, CA, USA), the Reaction steps were as follows: 50°C for 2 minutes Pre-PCR read, then 95°C for 10 minutes and 40 cycles of 95°C for 15 seconds, 60°C for 1 minute (cycling), and 60°C for 1 minute (Post-PCR).
The probe sequence for of the 11′- HSD1 rs12086634 was 5′CCCAGAGGATTTCT VIC/FAMCAGATGATTTCT-3′. The sequence of forward primer was 5′-GGAGGAGAATGGGAAAGGTATCAAC-3′, and the reverse primer was 5′-TCCTCCTGCAAGAGATGGCTATATT-3′. While, The probe sequence for of the 11′- HSD1 rs846910 was 5′-CTGGTGGGAATVIC/FAMTCAAATCAGAGAGA-3′. the sequence of forward primer was 5′-CTCTGTTGCTTGTGCTTGATTC-3′, and the reverse primer was 5′-AGAGCAGGCTTTCAGCAGATA C-3′ (Biosearch Technologies, Novato, CA, USA). Figure 1A and B shows the allelic discrimination plots of the SNP.
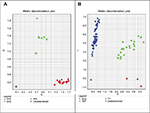  | Figure 1 Allelic discrimination plot of 11β-HSD1 rs846910 (A/G) (A) and rs12086634 (G/T) (B). |
Statistical analysis
Results were collected, tabulated and statistically analyzed by IBM personal computer and statistical package SPSS version 20 (IBM Corporation, Armonk, NY, USA). Hardy–Weinberg equilibrium was computed to exclude any bias of results. Qualitative data were expressed using number and percent, while quantitative data were described in mean ± SD. Student’s t-test was used for comparison between two groups having quantitative variables. Mann–Whitney and Kruskal–Wallis tests were used for comparison of two and three groups of non-parametric variables respectively. ORs were calculated using logistic regression with CI 95%. A P-value ≤0.05 was considered statistically significant.
Results
Personal, clinical and serological data of studied subjects
The personal and clinical data as well as the laboratory characteristics of the investigated subjects are shown in Table 1. Patient and control groups were matched as regards personal data except for BMI (P<0.001), where AV patients had a significantly higher percentage of overweight subjects, and ST patients demonstrated a significantly higher percentage of obese patients (Table 1).
There was a considerable variance among all the studied groups regarding serum level of TC, HDL, LDL, and cortisol, but a non-significant difference regarding TG. Compared to controls, AV and STs patients exhibited significantly higher mean values of TC, LDL, and cortisol, and lower HDL serum levels (P<0.001 for all) (Table 1).
11β HSD1 rs846910 and rs12086634 gene polymorphisms of studied groups
Our study of 11β HSD1 rs846910 (Figure 1A) and rs12086634 (Figure 1B) SNPs showed considerable significant differences among all studied groups, regarding rs846910 (GG, GA) and rs12086634 (TT, TG, GG) genotypes (P=0.044 and P=0.023, respectively) and rs12086634 allele distribution (P=0.001) (Figure 2).
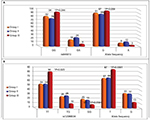  | Figure 2 Comparison between the three studied groups regarding 11β-HSD1 rs846910 (A) and rs12086634 (B) genotypes and allele distribution. |
By calculating ORs and CIs: we found that rs846910 GA genotype increases the risk of AV and STs by 3.4- and 4.9-fold, and its A allele increases the risk by 3.1 and 4.4, times respectively. While, rs12086634 TG genotype increases the risk of AV by 3.2-fold, as well as STs by 3.5-fold, and its G allele increases the risk of AV by 3.2-fold and STs by 7-fold (Table 2).
The relationship between 11β HSD1 rs846910 genotypes and assessed parameters in patients with AV and STs
There was a significant association between rs846910 GA genotype and BMI in groups I (P=0.023) and II (P<0.001), and was predominant among obese AV and STs patients (P=0.014; P=0.005, respectively) (Table 3).
  | Table 3 Relation between 11β-HSD1 rs846910 genotypes and BMI, lipid profile, and cortisol level in groups I and II Note: aData presented as mean ± SD; *Significant. Abbreviations: AV, acne vulgaris; STs, skin tags; HDL, high density lipoproteins; LDL, low density lipoproteins; t, Student’s t-test; n, number; χ2, chi-squared test; U, Mann–Whitney test. |
Regarding serum lipid profile and cortisol levels in AV and STs patients, rs846910 GA genotype was significantly associated with higher TC (P=0.008; P<0.001), LDL (P=0.023; P<0.001), and cortisol (P<0.001), and lower HDL (P=0.05; P=0.045), respectively, in addition to lower TG (P=0.006) in AV patients only (Table 3).
The relationship between 11β HSD1 rs12086634 genotypes and assessed parameters in patients with AV and STs
In AV patients, rs12086634 GG genotype carriers have significantly elevated BMI (P=0.006) and all of them were overweight and obese subjects (P=0.023). Also, these rs12086634 GG carriers recorded significantly increased TC (P=0.001) and LDL (P=0.002) serum levels. However, in the STs patient group, all rs12086634 GG genotype carriers were obese ones (P<0.001) and recorded a significantly higher number of ST lesions (0.008), and had significantly increased TC (P<0.001), LDL (P<0.001), and cortisol (P=0.005) serum levels (Table 4).
  | Table 4 Relation between HSD11B1rs12086634 genotypes and BMI, lipid profile, and cortisol level in groups I and II Note: aData presented as mean±SD; *Significant. Abbreviations: AV, acne vulgaris; STs, skin tags; HDL, high density lipoproteins; LDL, low density lipoproteins; t, Students t-test; χ2, chi-squared test; U, Mann–Whitney test; n, number. |
The relationship between rs12086634 and rs846910 genotypes and BMI, serum lipid profile, and cortisol levels in the control group
No significant relations were detected among different rs12086634 and rs846910 genotypes regarding BMI, serum lipid profile, and cortisol levels in the control subjects except rs846910 GA genotype that was significantly associated with high BMI (P=0.02) and elevated cortisol serum levels (P=0.025) (Table 5).
Correlation between cortisol serum level and different parameters in patients with AV and STs
In AV and STs patients, there were significant positive correlations between cortisol levels with disease severity (r=0.48, P<0.001 and r=0.294, P=0.038), BMI (r=0.671, P<0.001 and r=0.324, P=0.022), and serum levels of LDL (r=0.384, P=0.006 and r=0.415, P=0.003) and TC (r=0.388, P=0.005 and r=0.304, P=0.004, respectively), in addition to TG (r=0.549, P<0.001) and negative correlation regarding HDL (r= –0467, P<0.001) in AV patients only (Figure 3).
Discussion
The present work was designed to spot a beam of light on the possible role of 11β-HSD1 gene polymorphism in the pathogenesis of AV and STs, two of the most common metabolic-related skin diseases. Owing to the location of 11β-HSD1 rs12086634 and rs846910 in the transcription initiation place12 and considering the effect of 11β-HSD1 on cortisone activation and metabolic control,8,10 we investigated these two variants (rs12086634 and rs846910) of 11β-HSD1 gene and their end product (cortisol level), with lipid profile in a sample of Egyptian patients having AV and STs.
Our participants in both patient groups (AV and STs) had a significantly higher BMI than that of controls. This demonstrated high BMI represents a major risk factor of MeTS,22 that was previously reported in Norwegian acne female patients.23 Additionally, a low BMI was associated with low acne prevalence in Taiwanese girls and boys,24 as well as, Italian adolescents and young adults.25 Also in STs, Jusuf et al26 demonstrated a significantly high BMI.
Plausible mechanisms that explain the pathogenesis of STs in obesity could be hyperinsulinemia that increases IGF-1 which stimulates the proliferation of both keratinocytes27 and dermal fibroblasts,28 and/or increased leptin levels that has the ability to induce proliferation of keratinocytes.27,29 However, in AV, hyperinsulinemia influences follicular epithelial growth and stimulates sebocyte proliferation and androgen-mediated sebum secretion.30 Additionally, excess adipose tissue could induce lipid peroxidation affecting the inflammatory process and acne pathogenesis.31
AV is a multifactorial skin disease, in which hormones including glucocorticoids were implicated.32 Confirming this speculation, our AV patients demonstrated a significant increase in their cortisol serum levels than their matched peers. Steroids are supposed to increase acne eruptions (steroid acne) through increasing toll-like receptor 2 gene expressions with further release of the pro-inflammatory mediators.33
Altered lipid profile was reported in AV patients in different populations,34,35 with some differences in the evaluated results, that could be influenced by different nutritional state, diet, and lifestyle.35 Herein, we revealed significantly higher TC, LDL, and lower HDL in AV patients than controls. Therefore, we suggested that dyslipidemia may play an active role in AV pathogenesis, and may be a new target in AV management programs. Administration of a high niacin dose (≥200 mg/day), that regulates plasma lipids, is advised in the treatment of AV.36
Also, our STs’ patients demonstrated elevated cortisol serum levels and atherogenic lipid profile in the form of significantly high TC, LDL, and lower HDL serum levels. In line with these findings, are that of Erdogˇan et al37 and Shah et al.38
As the central nervous system (CNS) innervates adipose tissue via efferent pathways of a sympathetic nervous system, it was proposed that CNS is involved in the regulation of fat storage and lipolysis.39 It was demonstrated that high levels of stress hormones including cortisol are associated with an alteration in plasma lipid profile.40
In this study, analysis of 11β-HSD1 rs12086634 and rs846910 SNPs showed a positive association of 11β-HSD1 rs12086634 and rs846910 gene polymorphisms with both AV and STs. The frequency of 11β-HSD1 rs12086634 TG and rs846910 GA polymorphic genotypes, as well as their T and A alleles, respectively, were significantly higher in patients with AV and STs than their matched peers.
Parallel to our findings, a significant positive association was reported between 11β-HSD1 rs12086634 gene polymorphism and PCOS, the common insulin-resistant disorder.12,41 Based on these results, we can conclude the direct relation between 11β-HSD1 rs12086634 TG and rs846910 GA polymorphic genotypes, and development of AV as well as STs. However, due to the novelty of our work on these specific polymorphisms, more studies on a larger number of patients are prerequisite to clarify this issue.
Regarding quantitative variables, the current study showed that, in AV and ST patients, rs846910 GA genotype demonstrated significant associations with elevated BMI, TC, LDL, and cortisol, and decreased HDL levels, however, rs12086634 GG genotype was significantly associated with increased BMI, TC, and LDL serum levels, and the number of STs and cortisol levels in ST cases only.
11β-HSD1 is responsible for the conversion of cortisone to its metabolically active form cortisol that activates glucocorticoid receptors.8 An imbalance in the cortisol level is associated with hyperlipidemia, increased visceral fat and insulin resistance, all of which are related to MeTS, a state resembling Cushing’s syndrome.11 There is a significant body of data suggesting an important functional role of 11β-HSD1 in the metabolic processes. In 11β-HSD1 transgenic mouse (a model of MeTS) showed dyslipidemia, but in 11β-HSD1 knockout animals, normal lipid profiles were found.15 Moreover, 11β-HSD1gene polymorphisms influence lipid levels to develop MeTS.42
Our reported positive associations of 11β-HSD1 rs846910 GA and rs12086634 gene polymorphisms with the reported high BMI and atherogenic lipid profile in investigated AV and ST patients were more impressive, and support the role of increased activity of 11β-HSD1 (cortisone to cortisol conversion), in the form of increased cortisol serum levels which were demonstrated in the current work, and showed significant positive association with STs and AV disease severity.
Therefore, we could suggest that 11β-HSD1 rs846910 and rs12086634 gene polymorphisms participate in AV and ST pathogenesis through increasing its transcriptional activity as shown by a high cortisol level which has a role in the phenotypic appearance of both diseases denoted by its association with disease severity.
Although some authors suggested that11β-HSD1 polymorphic variants are not associated with MetS and obesity,43,44 that could be attributed to the ethnic difference in the population studied,12 as many researchers support our findings. They have reported a significant positive relationship between rs12086634 gene polymorphisms and MeTS in different populations.11,13–16 Moreover, rs12086634 (an intronic variant) acts as an intronic enhancer,42 that enhances conversion of inactive cortisone to its active form (cortisol) as our study showed. Furthermore, 11β-HSD1 inhibitors were shown to be effective in the treatment of different features of MetS, promoting weight loss and reducing hyperglycemia plus improving insulin resistance.45
Conclusion
11β-HSD1 rs846910 and rs12086634 gene polymorphisms may contribute in AV and ST pathogenesis in the Egyptian population, and may be mediated through enhancing its enzymatic activity and increased cortisol levels. We confirmed that AV and STs are associated with obesity and atherogenic lipid profile. Diagnosis of AV and STs may play a role in early detection of MeTS, and patients having these diseases need suitable interventions such as weight reduction and dietary habits.
Acknowledgment
We acknowledge the Central Laboratory Unit, Faculty of Medicine, Menoufia University for providing us with the necessary instruments for completion of the study.
Disclosure
The authors report no conflicts of interest in this work.
References
Karimkhani C, Dellavalle RP, Coffeng LE, et al. Global skin disease morbidity and mortality: an update from the global burden of disease study 2013. JAMA Dermatol. 2017;153(5):406–412. | ||
Labazi H, Trask AJ. Coronary microvascular disease as an early culprit in the pathophysiology of diabetes and metabolic syndrome. Pharmacol Res. 2017;123:114–121. | ||
Stefanadi EC, Dimitrakakis G, Antoniou C-K, et al. Metabolic syndrome and the skin: a more than superficial association. Reviewing the association between skin diseases and metabolic syndrome and a clinical decision algorithm for high risk patients. Diabetol Metab Syndr. 2018;10(1):9. | ||
Wolkenstein P, Machovcová A, Szepietowski JC, Tennstedt D, Veraldi S, Delarue A. Acne prevalence and associations with lifestyle: a cross-sectional online survey of adolescents/young adults in 7 European countries. J Eur Acad Dermatol Venereol. 2018;32(2):298–306. | ||
Zouboulis CC, Jourdan E, Picardo M. Acne is an inflammatory disease and alterations of sebum composition initiate acne lesions. J Eur Acad Dermatol Venereol. 2014;28(5):527–532. | ||
Abdou AG, Maraee AH, Antar AG, Fareed S. Role of mast cells in skin tag development: an immunohistochemical study. Anal Quant Cytopathol Histpathol. 2014;36(4):222–230. | ||
Allegue F, Fachal C, Pérez-Pérez L. Friction induced skin tags. Dermatol Online J. 2008;14(3):18. | ||
Tomlinson JW, Moore JS, Clark PM, Holder G, Shakespeare L, Stewart PM. Weight loss increases 11beta-hydroxysteroid dehydrogenase type 1 expression in human adipose tissue. J Clin Endocrinol Metab. 2004;89(6):2711–2716. | ||
Terao M, Katayama I. Local cortisol/corticosterone activation in skin physiology and pathology. J Dermatol Sci. 2016;84(1):11–16. | ||
Baudrand R, Vaidya A. Cortisol dysregulation in obesity-related metabolic disorders. Curr Opin Endocrinol Diabetes Obes. 2015;22(3):143–149. | ||
Devang N, Nandini M, Rao S, Adhikari P. HSD11B1 gene polymorphisms in type 2 diabetes and metabolic syndrome—do we have evidence for the association? Int J Diabetes Dev Ctries. 2016;36(1):95–102. | ||
Devang N, Satyamoorthy K, Rai PS, Nandini M, Basu A, Adhikari P. Association of HSD11B1 rs12086634 and HSD11B1 rs846910 gene polymorphisms with polycystic ovary syndrome in South Indian women. Int J Diabetes Dev Ctries. 2018;38(4):381–386. | ||
Gambineri A, Tomassoni F, Munarini A, et al. A combination of polymorphisms in HSD11B1 associates with in vivo 11b-HSD1 activity and metabolic syndrome in women with and without polycystic ovary syndrome. Eur J Endocrinol. 2011;165(2):283–292. | ||
Moon SS, Lee YS, Kim JG, et al. Relationship of 11β-hydroxysteroid dehydrogenase type 1 and hexose-6-phosphate dehydrogenase gene polymorphisms with metabolic syndrome and type 2 diabetes. Endocr J. 2011;58(11):949–959. | ||
Walker BR, Andrew R. Tissue production of cortisol by 11beta-hydroxysteroid dehydrogenase type 1 and metabolic disease. Ann N Y Acad Sci. 2006;1083(1):165–184. | ||
Gandhi K, Adhikari P, Basu A, Achappa B. Association between a 11β-hydroxysteroid dehydrogenase type 1 gene polymorphism and metabolic syndrome in a South Indian population. Metab Syndr Relat Disord. 2013;11(6):397–402. | ||
Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA. 2002;288(14):1728–1732. | ||
Rasi A, Faghihi A, Rahmanzadeh Y, Hassannejad H. A comparison study of lipid profile levels between skin tags affected people and normal population in Tehran, Iran. Adv Biomed Res. 2014;3:109. | ||
Hayashi N, Akamatsu H, Kawashima M; Acne Study Group. Establishment of grading criteria for acne severity. J Dermatol. 2008;35(5):255–260. | ||
Ghasemi A, Asgari S, Hadaegh F, et al. New modified Friedewald formulae for estimating low-density lipoprotein cholesterol according to triglyceride levels: extraction and validation. Endocrine. 2018;62(2):404–411. | ||
Friess E, Schiffelholz T, Steckler T, Steiger A. Dehydroepiandrosterone – a neurosteroid. Eur J Clin Invest. 2000;30 Suppl 3(S3):46–50. | ||
Melnik BC1, John SM, Plewig G. Acne: risk indicator for increased body mass index and insulin resistance. Acta Derm Venereol. 2013;93(6):644–649. | ||
Halvorsen JA, Vleugels RA, Bjertness E, Lien L. A population-based study of acne and body mass index in adolescents. Arch Dermatol. 2012;148(1):131–132. | ||
Tsai MC, Chen W, Cheng YW, Wang CY, Chen GY, Hsu TJ. Higher body mass index is a significant risk factor for acne formation in schoolchildren. Eur J Dermatol. 2006;16(3):251–253. | ||
di Landro A, Cazzaniga S, Parazzini F, et al. Family history, body mass index, selected dietary factors, menstrual history, and risk of moderate to severe acne in adolescents and young adults. J Am Acad Dermatol. 2012;67(6):1129–1135. | ||
Jusuf NK, Putra IB, Kartayana J. The correlation between body mass index with the occurrence of skin tag. Open Access Maced J Med Sci. 2017;5(3):271–274. | ||
Agamia N, Gomaa S. Assessment of serum leptin, atherogenic lipids, glucose level, insulin resistance and metabolic syndrome in patients with skin tags. Egypt J Dermatol Venerol. 2014;34(1):58–64. | ||
Bosseila M, Shaker O. The tissue expression of insulin-like growth factor (IGF-1) in acrochordons. J Egypt Wom Dermatol Soc. 2007;4(2):57–62. | ||
Gorpelioglu C, Erdal E, Ardicoglu Y, Adam B, Sarifakioglu E. Serum leptin, atherogenic lipids and glucose levels in patients with skin tags. Indian J Dermatol. 2009;54(1):20–22. | ||
Cordain L, Lindeberg S, Hurtado M, Hill K, Eaton SB, Brand-Miller J. Acne vulgaris: a disease of Western civilization. Arch Dermatol. 2002;138(12):1584–1590. | ||
Rohr UD. The impact of testosterone imbalance on depression and women’s health. Maturitas. 2002;41(1):25–46. | ||
Elsaie ML. Hormonal treatment of acne vulgaris: an update. Clin Cosmet Investig Dermatol. 2016;9:241–248. | ||
Shibata M, Katsuyama M, Onodera T, Ehama R, Hosoi J, Tagami H. Glucocorticoids enhance toll-like receptor 2 expression in human keratinocytes stimulated with Propionibacterium acnes or proinflammatory cytokines. J Invest Dermatol. 2009;129(2):375–382. | ||
Shrestha S. Correlation of hormonal profile and lipid levels with female adult acne in a tertiary care center of Nepal. J Nepal Health Res Counc. 2018;16(2):222–227. | ||
Jiang H, Li CY, Zhou L, et al. Acne patients frequently associated with abnormal plasma lipid profile. J Dermatol. 2015;42(3):296–299. | ||
Duffy D, Rader DJ. Update on strategies to increase HDL quantity and function. Nat Rev Cardiol. 2009;6(7):455–463. | ||
Erdogˇan BS, Aktan S, Rota S, Ergin S, Evliyaogˇlu D. Skin tags and atherosclerotic risk factors. J Dermatol. 2005;32(5):371–375. | ||
Shah R, Jindal A, Patel N. Acrochordons as a cutaneous sign of metabolic syndrome: a case-control study. Ann Med Health Sci Res. 2014;4(2):202–205. | ||
Qureshi GM, Seehar GM, Zardari MK, Pirzado ZA, Abbasi SA. Study of blood lipids, cortisol and haemodynamic variations under stress in male adults. J Ayub Med Coll Abbottabad. 2009;21(1):158–161. | ||
Maduka IC, Neboh EE, Ufelle SA. The relationship between serum cortisol, adrenaline, blood glucose and lipid profile of undergraduate students under examination stress. Afr Health Sci. 2015;15(1):131–136. | ||
Gambineri A, Vicennati V, Genghini S, et al. Genetic variation in 11beta-hydroxysteroid dehydrogenase type 1 predicts adrenal hyperandrogenism among lean women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2006;91(6):2295–2302. | ||
Nair S, Lee YH, Lindsay RS, et al. 11beta-Hydroxysteroid dehydrogenase type 1: genetic polymorphisms are associated with type 2 diabetes in Pima Indians independently of obesity and expression in adipocyte and muscle. Diabetologia. 2004;47(6):1088–1095. | ||
Miyamoto Y, Morisaki H, Yamanaka I, et al. Association study of 11beta-hydroxysteroid dehydrogenase type 1 gene polymorphisms and metabolic syndrome in urban Japanese cohort. Diabetes Res Clin Pract. 2009;85(2):132–138. | ||
Turek LV, Leite N, Rodrigues Souza RL, et al. Gender-dependent association of HSD11B1 single nucleotide polymorphisms with glucose and HDL-C levels. Genet Mol Biol. 2014;37(3):490–495. | ||
do Nascimento FV, Piccoli V, Beer MA, von Frankenberg AD, Crispim D, Gerchman F. Association of HSD11B1 polymorphic variants and adipose tissue gene expression with metabolic syndrome, obesity and type 2 diabetes mellitus: a systematic review. Diabetol Metab Syndr. 2015;7(1):38. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




