Back to Journals » Research and Reports in Urology » Volume 14
Role and Training of the Bedside Surgeon in Robotic Surgery: A Survey Among French Urologists-in-Training
Authors Lagrange F, Fiard G, Larose C, Eschwege P, Hubert J
Received 15 November 2021
Accepted for publication 11 January 2022
Published 18 January 2022 Volume 2022:14 Pages 17—22
DOI https://doi.org/10.2147/RRU.S344369
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Panagiotis J Vlachostergios
Francois Lagrange,1 Gaelle Fiard,2,3 Clement Larose,1 Pascal Eschwege,1 Jacques Hubert1,4
1Department of Urology, University Hospital Nancy-Brabois, Vandœuvre-lès-Nancy, Nancy, 54511, France; 2Department of Urology, Grenoble Alpes University Hospital, Grenoble, 38043, France; 3University Grenoble Alpes, CNRS, Grenoble INP, TIMC-IMAG, Grenoble, 38043, France; 4IADI-UL-INSERM (U1254), University Hospital Nancy-Brabois, Vandœuvre-lès-Nancy, Nancy, 54511, France
Correspondence: Francois Lagrange, Tel +33 83 15 31 52, Email [email protected]
Introduction: Due to the development of robotic surgery, surgeons operating at the console are physically separated from the patient. They must rely on help from an assistant, also called bedside surgeon. This study aimed to investigate the habits and practices of French urologic residents when performing this role and to determine whether they expected specific training to qualify as bedside surgeons.
Materials and Methods: A web-based survey was sent to French urology residents and fellows using the mailing-list of the French Association of Urologists in Training (AFUF).
Results: Over a 3-month period, 86 residents and fellows responded to the survey. Seventy-five (87.2%) thought that an experience as bedside surgeon was useful to acquire console surgeon status and, more specifically, 48.2% of them indicated that this former experience was vital. Nearly 64% considered that learning robotic surgery was essential during residency and fellowship. Overall, 91.9% believed that bedside surgeons should receive a formal training. They were 69.7% to need 5 to 10 procedures to feel confident as bedside surgeon. Almost 75% underwent laparoscopic training on simulators. Having access to a surgery school significantly increased the probability of receiving laparoscopic training on simulators (p = 0.0033).
Conclusion: French urology residents and fellows expect a specific training program for bedside surgeons to increase their level of confidence and to get familiar with the device during their first robotic procedures. For them, a bedside surgeon program on a regional/national level would be required.
Keywords: education, residency, surgical training, robotic training, robot
Introduction
The past 20 years have witnessed an exponential development of robotic surgery in urology, general surgery and gynaecology, among others.1 In 2020, over 5800 Da Vinci™ robotic systems were being used around the world.
Most studies are looking at the feasibility and evaluate the results of procedures from the point of view of the console surgeon. There are different training programs for the console surgeon. Academic programs were described such as the EAU Robotic Urology Section (ERUS).2 Training programs include theoretical knowledge, simulation, console management and non-technical skills to learn.
However, the console surgeon belongs to a surgical team and a training of the whole team is needed,2,3 especially the assistant or bedside surgeon, the latter being the sole scrubbed surgeon during the console time. Its skills allow performing critical tasks (quick instruments exchange, lavage, aspiration, clip application, etc.).4,5
The aim of this study was two folds: describe the practices of the French urologic residents and fellows when they assisted robotic surgery as bedside surgeon and if they expected a specific training before performing this role.
Materials and Methods
A questionnaire was designed after informal discussions between robotic experts, residents and fellows due to a lack of validated questionnaire on this subject. Then, it was sent to the French residents and fellows in Urology as a web-based survey using the mailing-list of the French Association of Urologists in Training (AFUF). The answers to the survey were anonymous and voluntary. Respondents had to answer all questions (except free text fields) before submitting their answer. Most questions were multiple choice questions and some free text boxes where applicable. The different parts captured the demographics of the surveyed urologists-in-training (localization of the university, number of residency/fellowship semesters passed, etc.), the characteristics of the surgical departments they were attached to (robot system, dual console availability, robotic theatre time dedicated to urology, etc.), and finally, their learning and robotic experience (exposure, number of interventions, access to a school of surgery, simulations, bedside surgeon training, common problems experienced as bedside assistants as free text, etc.). The questionnaire is provided in Appendix.
The study was approved by the Institutional review board of the AFUF before being sent to members. Before answering the questionnaire, participants had to provide their consent. The survey participants were informed about the purpose of the study. The guidelines outlined in the Declaration of Helsinki were followed.
Data were collated using Google Form™ and used for descriptive analysis. Results are presented as means. Statistical analysis was performed using SAS v9.4 for analysis of variance (ANOVA), correlation tests and chi-square tests. p values ‹0.05 were considered statistically significant.
Results
We received 86 voluntary responses among the 379 urologists-in-training members of the AFUF (response rate 22.7%), collected over a three-month period. Among these, 66 were residents and 20 fellows. They had spent on average 3.6 semesters (21.6 months) in urologic departments and 2.4 semesters (14.4 months) in departments where robotic surgery was performed.
Laparoscopy and Robotic Surgery Training
Among the respondents, 66 (73.3%) received laparoscopic training using simulators. Simulators used included a Pelvitrainer™ for 37 (58.7%), Pelvitrainer™ and Simbionix™ laparoscopic simulator for 5 (7.9%), Pelvitrainer™ and another device for 17 (27.0%).
For robotic surgery training, 20 (31.7%) reported having received training on robotic simulators or wet labs (porcine model). Access to a school of surgery attached to their university was available in their region for 47 (54.7%) of the participants. In one case, for 7 (8.1%), the school was not open to residents. Having access to a surgery school significantly increased the probability of receiving laparoscopic training on simulators (p=0.0033).
Robotic Surgery Exposure
For 31 (36.0%) of the responding residents and fellows, robotic surgery was only performed in the University Hospital they were attached to. Among them, 55 (64.7%) played the role of bedside surgeons solely in this University Hospital and 29 (33.8%) were equipped with a dual console robot. The average robotic theatre time dedicated to urology departments was 5.5 half-days per week. In the respondents’ departments, the robot was shared with the gynaecology department in 80.2% (69), with general surgery in 68.6% (59), with Head & Neck surgery in 31.4% (27) and with paediatric surgery in 31.4% (21).
Regarding their training and their robotic experience, 64% thought that robotic surgery training and learning was essential during residency or fellowship (Table 1).
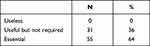 |
Table 1 Robotic Surgery Training and Learning During Residency and Fellowship |
Bedside Surgeon Training
For 79 (91.9%) of the respondents, a specific training for bedside surgeons should be mandatory. (Table 2). The average ideal duration for this kind of training program should be, in their view, 6.4 days SD. The promoter should be a university for 58% (Table 3). It should be conducted, according to them during the first year of residency for 36.0%, the second year for 22.1% and the third year for 26.7%.
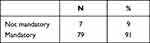 |
Table 2 Specific Training for Bedside Surgeon |
 |
Table 3 Promoter of the Bedside Surgeon Specific Training |
Among the respondents, 69.8% noted they would be ready to follow this training in their university or even a national expert centre (not currently available in France) for 54.7%.
Most participants responded that they had begun as bedside surgeons before the 4th semester (2nd year of residency). In 30.2% (26) of the cases, they were not accompanied for their first procedure as bedside assistant. Overall, residents were the sole member of the surgical team at patient side during robotic cases (94.2%). In 55.8% (48) of the cases, the numbers of residents in the department did not allow them to work in pairs in the operating room.
Regarding conventional laparoscopy, according to 19.8% (17), the principal surgeon required residents to have previous assistant experience, whereas 36% (31) in robotic surgery.
Among the participants, 95.0% (82) had already assisted over 10 robotic cases and 61.6% (53) over 30 prior to the survey. For 73.2% (60) of the respondents, a minimal number of 5 to 10 procedures seemed necessary to feel comfortable as bedside surgeon (mean = 8.2 cases). Overall, 87.2% (75) thought that prior bedside surgeon experience was useful to become console surgeon in robotic surgery and 48.8% (42) considered this prior experience as useful and vital (Table 4). Regarding the advantages of bedside surgeon experience before being console surgeons, 27.9% (24) thought that it was useful to know what is expected from the assistant, 23.3% (20) noted it could help to prevent instrument clashes and to manage them. According to 12.8% (11), this experience allowed to improve trocar placement and another 12.8% (11) for docking while 8.1% (7) reported that it enhanced their surgical knowledge.
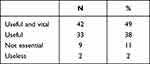 |
Table 4 Having Been Bedside Surgeon to Become Console Surgeon |
According to 72.1% (62) of the urologists-in-training surveyed, no specific training requirement was expected from console surgeons performing their first robotic cases at their institutions.
Problems Encountered as Bedside Surgeons
Difficulties encountered during robotic procedures comprised instrument clashes (29.1%), inadequate trocar placement with difficult instrument insertion and manipulation (13.9%) difficult communication due to the distance between the lead surgeon and his assistant (16.3%). 9.1% (8) reported being regularly hit by the robot’s arms. 16.3% (14) mentioned difficulties when applying hemostatic clips or vascular clamps.
Discussion
Robotic surgery requires a dedicated training for all team-members.3,6 For the French National Agency of Medicine and Health Products Safety, ANSM, as well as for the National Academy of Surgery,7 the bedside surgeon and its training remain of particular interest. This motivated our study which aimed both at assessing current training and robotic surgery exposure, but also the expectations of French urologists-in-training via the AFUF, to formalize this training. Among the respondents, 91.6% felt that such a training would be useful. Indeed, the emergence and the development of robotic surgery resulted in a new era for surgery and surgical education. Because robotic surgery implies remote handling, the surgeon cannot be in permanent contact by the side of the patient throughout the operation. Besides trocar placement, robot docking and skin closure, the surgeon stays at the console, looking at the patient through binoculars focused on a limited area of the operating site. In particular, the surgeon does not have a permanent view of the global operating field anymore as usually experienced with conventional approaches (open, laparoscopic, or even endoscopic surgery). It is even more accentuated as sight is one of the main sources of information for the surgeon in the absence of haptic feedback. Also, since the console is isolated from the surgical table, the surgeon is distanced from the rest of the team who remains at the patient side, surgically scrubbed. This distancing requires further mutual trust and experience among the different team members, and good communication between members of the team.
The number of incidents involving robotic surgery seems to be under-reported.8–10 Incidents were also observed in France, including cases of misuse of the robot due to a lack of training, even though the Intuitive Surgical Inc. company, which commercializes the robot, could provide initial training for the whole surgical team, as specified on its website. Alerted on the risks of insufficient training, The National Academy of Surgery (Académie Nationale de Chirurgie) issued new guidelines in November 2015 for surgeons starting as robotic surgeons.7 They highlighted the absence of visual communication between the surgeon and the rest of the team and consequently advocated for dedicated training of the entire team, especially for the bedside surgeon whose importance proved to be non-negligible.11
The importance of the bedside surgeon has been debated in the literature. For Kumar et al, the role of bedside surgeon in robotic surgery required more qualification than conventional surgery. Well trained, the bedside surgeon became as important as the surgeon operating from the console himself, having to master skills in open, laparoscopic and robotic surgery.4 Also, it was shown that an insufficiently trained assistant resulted in longer operating time5 and that the estimated blood loss could be reduced with a qualified bedside surgeon.
Other studies contradicted these findings. Potretzke et al studied 414 robot-assisted partial nephrectomies and found no significant difference in operative time, blood loss, oncological margins status and post-operative complications according to the academic level of the operating assistant.12 In another study looking at 129 robot-assisted prostatectomies performed by a single expert console surgeon, Albo et al showed that the experience of the bedside surgeon did not significantly impact perioperative results.13 Furthermore, Abu-Ghanem showed that the seniority level of the bedside surgeon had no influence on short-term outcomes collected after 106 robot-assisted prostatectomies.14 Of note, all these operations were conducted by a single expert console surgeon for whom the assistance of the bedside surgeon could be less critical than for surgeons with less expertise. In particular, the adjustment of the console surgeon to his assistants and his level of stress were not assessed, both of which could be confounder effects for favourable outcomes.15 Moreover, in our study, the principal surgeon expected their assistants to have more previous experience when performing robotic surgery than conventional laparoscopy. In our study, 75 (87%) respondents estimated that prior bedside surgeon experience in robotic surgery was helpful when becoming console operator; 42 (48.8%) added that it was essential. The importance of experience as bedside surgeon before becoming console surgeon has also been emphasized.16 According to Cimen, prior practice as bedside surgeon let the console surgeon reach better surgical outcomes for radical prostatectomy.17
To go into more details, Sheridan et al estimated that a surgeon should only operate from the console after 20 procedures as bedside surgeon,11 whereas Winder et al suggested 10 procedures as threshold in their training program.16 This is in keeping with our results, 73% of the respondents reporting that they would feel confident after 5 to 10 interventions. Many training programs are currently available or being developed around the world. Guzzo et al described 3 major phases in the training of a robotic surgeon.18 The first phase consisted in general knowledge about the robot, the second phase included training as bedside surgeon and the last phase was about operating from the console. In the second phase, teaching focused on trocar placement, robot docking, instrumentation, troubleshooting and specific knowledge of the different steps of a procedure. Such a training is offered by The EAU Robotic Urology Section (ERUS).2 This type of bedside surgeon training corresponds to the expectations of French urologists-in-training as collected in this study. A 3 phases training program could be suggested and would last 4 days in a national centre in the first year of residency.
Other authors aimed at standardizing bedside surgeon training in order to define and offer the most efficient and safest teaching program.19–21 Simulation-based training appears to play an essential role in bedside surgeon training. The interest of robotic simulation has been raised in multiple papers.22 Training on simulators is expected to flatten the learning curve and help novice surgeons to acquire essential skills and provide maximum safety for the patients.21,23 In our study, having access to a surgery school significantly increased the probability of receiving laparoscopic training on simulators. However, when looking at the role of simulators in bedside surgeon training, it must be noted that most simulators offer training for the console surgeon. Currently, the XperienceTM Team Trainer (XTT) simulator is the only simulator allowing to train both console and bedside surgeons together at the same time.24
In this study, training for robotic surgery was deemed essential or at least useful by 64% and 36% of participants, respectively. No respondent considered it to be useless. These numbers can be put into perspective with the study by Broholm et al, where 95% of American residents estimated that simulation training improved their skills and 92% of that they could transfer these skills to in-vivo interventions.25 Asked about more practical aspects of training, these residents suggested that training became compulsory, to make sure dedicated time was allocated and to guarantee access to the training tools - some schools being deprived of simulators.25,26 A 2013 study from the AFUF reported the under-utilization of simulation in urology training because of a lack of accessibility (lack of time and a lack of incentives) and unavailability of equipment.27 In the present study, 27.9% of the residents were eager to travel to a European center to be provided with such training. Though, training funding is currently problematic for residents.
To our knowledge, this study is the first national study assessing the need for a specific bedside surgeon training designed for urologists in training. The main limitation of this study lies in the relatively low response rate.28 Although it could be considered as good compared to other studies with a similar design, it can clearly lead to a selection bias, the population being the most interested in robotic surgery or feeling more deprived of specific training being more interested in responding to our study. Another limitation is due to the use of a non-validated questionnaire.
Conclusion
French residents experienced discomfort, technical and non-technical issues as they started their new role as bedside surgeon. Similarly, to console surgeon, a specific training program for bedside surgeon is expected by French urologic residents and fellows to increase their level of confidence and to get familiar with the device during their first robotic procedures.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Leal Ghezzi T, Campos Corleta O. 30 years of robotic surgery. World J Surg. 2016;40(10):2550–2557. doi:10.1007/s00268-016-3543-9
2. Professionals SO. ERUS robotic curriculum. Uroweb. Available from: https://uroweb.org/section/erus/education/.
3. Raison N, Wood T, Brunckhorst O, et al. Development and validation of a tool for non-technical skills evaluation in robotic surgery—the ICARS system. Surg Endosc. 2017;31(12):5403–5410. doi:10.1007/s00464-017-5622-x
4. Kumar R, Hemal AK. The “scrubbed surgeon” in robotic surgery. World J Urol. 2006;24(2):144–147. doi:10.1007/s00345-006-0068-0
5. Sgarbura O, Vasilescu C. The decisive role of the patient-side surgeon in robotic surgery. Surg Endosc. 2010;24(12):3149–3155. doi:10.1007/s00464-010-1108-9
6. Collins JW, Dell’Oglio P, Hung AJ, Brook NR. The importance of technical and non-technical skills in robotic surgery training. Eur Urol Focus. 2018;4(5):674–676. doi:10.1016/j.euf.2018.08.018
7. Les préconisations | académie Nationale de Chirurgie. Available from: https://www.academie-chirurgie.fr/publications/les-preconisations.
8. Cooper MA, Ibrahim A, Lyu H, Makary MA. Underreporting of robotic surgery complications. J Healthc Qual. 2015;37(2):133–138. doi:10.1111/jhq.12036
9. Alemzadeh H, Raman J, Leveson N, Kalbarczyk Z, Iyer RK. Adverse events in robotic surgery: a retrospective study of 14 years of FDA data. Lee HS, ed. PLoS One. 2016;11(4):e0151470. doi:10.1371/journal.pone.0151470
10. Gupta P, Schomburg J, Krishna S, et al. Development of a classification scheme for examining adverse events associated with medical devices, specifically the DaVinci surgical system as reported in the FDA MAUDE database. J Endourol. 2017;31(1):27–31. doi:10.1089/end.2016.0396
11. Sheridan C, Bach C, Koupparis A. How to train your surgeon! Experience of a patient side assistant. Arab J Urol. 2014;12(1):62–63. doi:10.1016/j.aju.2013.08.015
12. Potretzke AM, Knight BA, Brockman JA, et al. The role of the assistant during robot-assisted partial nephrectomy: does experience matter? J Robot Surg. 2016;10(2):129–134. doi:10.1007/s11701-016-0582-z
13. Albo G, De Lorenzis E, Gallioli A, et al. Role of bed assistant during robot-assisted radical prostatectomy: the effect of learning curve on perioperative variables. Eur Urol Focus. 2020;6(2):397–403. doi:10.1016/j.euf.2018.10.005
14. Abu-Ghanem Y, Erlich T, Ramon J, Dotan Z, Zilberman DE. Robot assisted laparoscopic radical prostatectomy: assistant’s seniority has no influence on perioperative course. J Robot Surg. 2017;11(3):305–309. doi:10.1007/s11701-016-0655-z
15. Sorokin I, Nelson J, Canvasser NE. Re: robot-assisted laparoscopic radical prostatectomy: assistant’s seniority has no influence on perioperative course. J Robot Surg. 2018;12(3):389–390. doi:10.1007/s11701-018-0836-z
16. Winder JS, Juza RM, Sasaki J, et al. Implementing a robotics curriculum at an academic general surgery training program: our initial experience. J Robot Surg. 2016;10(3):209–213. doi:10.1007/s11701-016-0569-9
17. Cimen HI, Atik YT, Gul D, Uysal B, Balbay MD. Serving as a bedside surgeon before performing robotic radical prostatectomy improves surgical outcomes. Int Braz J Urol. 2019;45(6):1122–1128. doi:10.1590/s1677-5538.ibju.2019.0330
18. Guzzo TJ, Gonzalgo ML. Robotic surgical training of the urologic oncologist. Urol Oncol. 2009;27(2):214–217. doi:10.1016/j.urolonc.2008.09.019
19. Ahmed K, Khan R, Mottrie A, et al. Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int. 2015;116(1):93–101. doi:10.1111/bju.12974
20. Tom CM, Maciel JD, Korn A, et al. A survey of robotic surgery training curricula in general surgery residency programs: how close are we to a standardized curriculum? Am J Surg. 2019;217(2):256–260. doi:10.1016/j.amjsurg.2018.11.006
21. Zhao B, Lam J, Hollandsworth HM, et al. General surgery training in the era of robotic surgery: a qualitative analysis of perceptions from resident and attending surgeons. Surg Endosc. 2019. doi:10.1007/s00464-019-06954-0
22. Fiard G, Descotes JL, Troccaz J. [Simulation-based training in urology: a systematic literature review]. Prog Urol. 2019;29(6):295–311. French. doi:10.1016/j.purol.2019.03.003
23. Thiel DD, Lannen A, Richie E, Dove J, Gajarawala NM, Igel TC. Simulation-based training for bedside assistants can benefit experienced robotic prostatectomy teams. J Endourol. 2013;27(2):230–237. doi:10.1089/end.2012.0382
24. Xu S, Perez M, Perrenot C, Hubert N, Hubert J. Face, content, construct, and concurrent validity of a novel robotic surgery patient-side simulator: the XperienceTM Team Trainer. Surg Endosc. 2016;30(8):3334–3344. doi:10.1007/s00464-015-4607-x
25. Broholm M, Rosenberg J. Surgical residents are excluded from robot-assisted surgery. Surg Laparosc Endosc Percutan Tech. 2015;25(5):449–450. doi:10.1097/SLE.0000000000000190
26. Shetty S, Zevin B, Grantcharov TP, Roberts KE, Duffy AJ. Perceptions, training experiences, and preferences of surgical residents toward laparoscopic simulation training: a resident survey. J Surg Educ. 2014;71(5):727–733. doi:10.1016/j.jsurg.2014.01.006
27. Fiard G, Capon G, Rizk J, et al. The role of simulation in the curriculum of French urologists-in-training: a study by the French Association of Urologists-in-Training (AFUF). Prog Urol. 2014;24(6):390–396. doi:10.1016/j.purol.2013.10.013
28. Cunningham CT, Quan H, Hemmelgarn B, et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol. 2015;15:1. doi:10.1186/s12874-015-0016-z
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
