Back to Journals » Therapeutics and Clinical Risk Management » Volume 16
Robot-Assisted Total Hip Arthroplasty for Arthrodesed Hips
Authors Chai W, Kong X, Yang M , Puah KL , Tang P, Chen J
Received 18 January 2020
Accepted for publication 15 April 2020
Published 4 May 2020 Volume 2020:16 Pages 357—368
DOI https://doi.org/10.2147/TCRM.S246565
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Wei Chai, 1 Xiangpeng Kong, 1 Minzhi Yang, 1, 2 Ken Lee Puah, 3 Peifu Tang, 1 Jiying Chen 1
1Department of Orthopedics, Chinese PLA General Hospital, Beijing, People’s Republic of China; 2Medical College, Nankai University, Tianjin, People’s Republic of China; 3Department of Orthopedic Surgery, Singapore General Hospital, Singapore
Correspondence: Jiying Chen; Peifu Tang Tel +8610-66938404
; +8610-66938304
Email [email protected]; [email protected]
Background: Conversion of arthrodesed hips to total hip arthroplasty (THA) remains technically demanding. This study aims to evaluate the safety and efficacy of robot-assisted THA in arthrodesed hips.
Methods: We retrospectively analyzed 45 ankylosing spondylitis patients with hip arthrodesis in the Chinese PLA General Hospital between August 2018 and August 2019. All surgeries were carried out by one single surgeon. The patients were followed at 3 months after surgery. Gender, body mass index, angle of hip arthrodesis, operating time, intraoperative fluoroscopic times, postoperative length of hospitalization, cup positioning, postoperative leg length discrepancy, offset discrepancy, intraoperative and postoperative complications, and postoperative Harris Hip Score were collected for all patients.
Results: Twenty-two patients (35 hips) who underwent robot-assisted THA and 23 patients (37 hips) who underwent manual THA were enrolled in this study. There were no significant differences in demographics and arthrodesed angles between the two groups. The fluoroscopic times during manual THA were significantly higher than those during robot-assisted THA (2.16± 1.61 vs 0.47± 0.61, respectively, p=0.000). In the robotic group, the percentage of acetabular cups within the safe zone was significantly greater than in the manual group (94.29% vs 67.56%, respectively, p=0.042). For manual THA, the anteversions were significantly different between the left and right sides (21.14± 7.86 vs 16.00± 6.32, respectively, p=0.042); however, no such significant difference was found in robot-assisted THA.
Conclusion: Compared with manual THA for arthrodesed hips, robot-assisted THA had significant advantages in improving the frequency of achieving cup positioning within the target zone with diminished radiation dose and no increase in operating time.
Keywords: total hip arthroplasty, robot-assisted surgery, cup positioning, hip arthrodesis
Corrigendum for this paper has been published
Introduction
Ankylosing spondylitis (AS) is the prototype of immune-mediated inflammatory rheumatic diseases grouped under the term spondyloarthritis (SpA).1,2 The prevalence of AS is between 0.1% and 1.4% worldwide.3 As a chronic and painful degenerative arthritis, it primarily affects the spine, sacroiliac joints and peripheral joints.3,4
Hips are the most susceptible peripheral joints. Up to 8% of AS patients ultimately require total hip arthroplasty (THA).1 Although many studies have shown the clinical outcome of hip replacement in AS patients to be satisfactory, conversion of the arthrodesed hip to THA is very technically demanding. This is due to altered anatomy during the exposure and difficulty in correctly identifying the true acetabulum.5–11 A lack of defined anatomical landmarks and deceptive intraoperative positioning of the patient tend to cause cup malpositioning, which would increase the risk of dislocation and accelerating polyethylene wear after THA.12–15 In recent years, the use of robot-assisted technology in executing THA for many complex cases has increased, and many studies have reported that robots can improve the accuracy of prosthetic positioning in THA.14,16-18 Therefore, we conducted a retrospective cohort study to evaluate the safety and efficacy of robot-assisted THA for arthrodesed hips.
Patients and Methods
We retrospectively analyzed the AS patients who had arthrodesed hips and underwent hip replacement in our prospectively constructed joint registry system between August 2018 and August 2019. The diagnostic criterion of hip arthrodesis was an absence of joint space with trabeculae traversing the joint on computed tomography (CT). Inclusion criteria were: 1) the hip was arthrodesed in the extended position (the angle between the shaft of the femur and the anterior pelvic plane was within 20°); 2) the spinal deformity did not need surgical correction after the consultation with a spinal surgeon; 3) all surgeries used the cementless acetabular cup (Trident; Stryker, Mahwah, USA), tapered cementless stem (AccoladeII; Stryker, Mahwah, USA) and ceramic on highly cross-linked polyethylene (CoP); and 4) all surgeries were performed by one senior surgeon (CJY) with or without the assistance of a robot. Exclusion criteria were: 1) patients who had unilateral hip arthrodesis undergoing bilateral THA; and 2) patients who had incomplete clinical data or non-standard radiographs. The study protocol was approved by the Medical Ethics Committee of Chinese PLA General Hospital. Written informed consent was obtained from all patients. Robot-assisted THA was suggested for all patients. Since it usually took 2 weeks to draw up the surgical plan for robot-assisted THA, the patients who underwent robot-assisted THA had to go home and wait for 2 weeks after the CT scan. This was time consuming for patients who lived far from the hospital. The surgeon had no preference for any given technique with any particular patient group. In practice, the surgeon would take each patient’s opinion into full consideration and decide on the surgical method.
Fifty-four patients met the inclusion criteria. Two patients were excluded because of the first exclusion criterion and three patients were excluded because of the second exclusion criterion. Four patients were lost to follow-up, and finally 45 patients (72 hips) were enrolled in this study. Among these cases, 22 patients (35 hips; 19 left hips and 16 right hips) underwent robot-assisted THA and 23 patients (37 hips; 22 left hips and 15 right hips) manual THA.
Surgical Procedure: Robot-Assisted THA
In our institute, the Mako THA system (Stryker, Mahwah, USA) was used to enable robot-assisted THA. For the patients who underwent robot-assisted THA, the preoperative surgical plans of the three-dimensional template were created in the robotic system.
- Construction and segmentation (Figure 1). Preoperative CT DICOM images of bilateral hip and knee were imported into the robotic system for the template. The segmentation of arthrodesed hips was different from the technique utilized in standard robot-assisted THA. When segmenting the pelvis with the standard technique, the pelvis is separated from the femur and they are registered as two independent bones. In arthrodesed hips, the pelvis and femur are regarded as an integrated bone with no attempt to separate the bones during segmentation. The new method of construction and segmentation requires registration of the pelvis prior to femoral neck osteotomy, which has not been described in previous studies.
- Preoperative surgical plan (Figure 2). Several anatomical landmarks could be found easily in the CT scans. The fossa acetabuli, which was filled by the fatty ligamentum capitis femoris, could be used to identify the acetabular floor. The transverse acetabular ligament and calcified joint space could be used to identify the acetabular wall. Based on these landmarks, we were able to make a template of the size and depth of the acetabular cup. All acetabular cups were set at 40° (inclination) and 20° (anteversion) in the initial preoperative plan.

Figure 2 Preoperative surgical plan of positioning of components in the robotic system.
- Preparation and approach. The pelvic tacking array was placed in the iliac crest prior to skin incision. All surgeries were performed through a posterolateral approach. Checkpoints were placed during the exposure to enable leg length and offset measurement.
- Registration and in-situ osteotomy. The surgeon began the virtual registration after removing the soft tissue surrounding the acetabular posterior wall and greater trochanter. The first three landmarks should, in theory, be located in the posterior acetabulum, anterior acetabulum and superior acetabulum. In this study, the landmarks were changed to the posterior acetabulum, greater trochanter and neck–pelvis junction, respectively (Figure 3). Then, pelvic registration was completed according to system prompts and instructions. The registration points should be located as far apart from each other as possible in the operating area, because these initial landmarks will determine the distribution range of the next 32 registration points. Incorrect initial landmarks would yield some unattainable points and thus compromise the registration accuracy. Two methods were used to verify the accuracy of registration. The first was to check the color of registration points. Green is the most accurate (<0.5 mm), followed by yellow (0.5–1.5 mm), and red is not accurate (>1.5 mm) (Figure 4). The second was to use the location of verification points (blue changed to white) and distance to bone (<1 mm) (Figure 5). Pelvic registration was considered accurate only if there were fewer than three red dots and all verification points were passed. After pelvic registration, the in-situ osteotomy was performed perpendicular to the femoral neck to enable mobilization of the femur while minimizing the risk of damage to the acetabular anterior wall. Then femur was pulled forward to expose the acetabulum.

Figure 3 Preoperative

Figure 4 Accuracy of intraoperative pelvic registration (green points: <0.5 mm; yellow points: 0.5–1.5 mm; red points: >1.5 mm).

Figure 5 Verification of intraoperative pelvic registration (blue points changed to white and distance to bone was <1 mm).
- Reaming and cup implantation. The surgeon moved the reamer into the acetabulum. With the help of the haptic arm, the planned volume bone was removed with a reamer (Figure 6). Then, the surgeon impacted the acetabular cup into the planned position. Finally, acetabular screws were placed and the acetabular liner was impacted in place. The femoral stem was implanted manually (Figure 7). Joint stability was tested through a range-of-motion assessment to determine the direction of the elevated rim of the polyethylene liner. The final orientations of the acetabular cup, LLD and offset were recorded. Intraoperative fluoroscopy was used when the stem alignment could not be determined.
Figure 6 Intraoperative image of acetabulum reaming (the white acetabulum is the planned volume of bone being removed).

Figure 7 Comparison of preoperative surgical plan and postoperative X-rays of the arthrodesed hip. (A) Robotic surgical plan. (B) Actual postoperative X-rays.
Surgical Procedure: Manual THA
For the patients who underwent manual THA, the preoperative surgical plans of the two-dimensional template were made in Orthoview software (version 6.6.1; Materialise, Leuven, Belgium). The procedures of exposure and osteotomy were as described in the previous subsection. The surgeon used the smallest reamer to search for the fatty ligamentum capitis femoris to determine the acetabular floor, then used larger reamers, in turn, to remove the femoral head and prepare the acetabulum. The acetabular cup and femoral stem were implanted manually. Intraoperative fluoroscopy was used when the acetabular floor, acetabular wall or stem alignment could not be determined.
When femoral fracture occurred during the operation, it was managed according to its location and severity. Robots cannot help with the management of femoral fracture.
Follow-Up and Radiographic Measurements
The patients were reviewed at 3 months after surgery and X-rays were taken of the anteroposterior pelvis in the supine position. When taking postoperative X-rays, the hips were in 10–15° of internal rotation and the X-ray beam was centered over the pubic symphysis. The longitudinal axis of the body and legs was parallel to the imaging table. The acetabular cups were used to calibrate the radiographs to eliminate magnification errors.
The patients’ age, gender, body mass index (BMI) and angle of hip arthrodesis were collected in our joint registry system.
The operating time, fluoroscopic times during the operation, postoperative length of hospitalization (LOH), position of the acetabular cup, postoperative leg length discrepancy (LLD), offset, intraoperative and postoperative complications, and postoperative Harris Hip Score (HHS) were collected for each patient at 3 months after surgery.
The angle between the long axis of the femoral shaft and bilateral teardrops’ connecting line was used to evaluate whether X-rays were standard. If the angle was greater than 10°, the related data of LLD and offset were excluded.
The operating time was defined as the time from initial incision to final wound closure.
The orientation of the acetabular cup was measured on X-rays with Orthoview software. The anteversion of the cup was the angle between the short and long axes of the ellipse projected by the cup. Anteversion = arcsin (short axis/long axis). The inclination of the cup was the angle between the cup’s long axis and bilateral teardrops’ connecting line. The accuracy of this software for measuring inclination and anteversion has been validated.19 Then, we calculated every cup’s anteversion and inclination that were within Lewinnek’s safe zones.16,20
The LLD was the difference in distance between the lesser trochanters and bilateral teardrops’ connecting line. If teardrops or lesser trochanters were poorly visible, the ischial tuberosity or greater trochanters were used as their substitutions, respectively.
Offset was the distance between the center of the femoral head and the long axis of the femoral shaft. Offset discrepancy (offset-D) was the difference between bilateral offsets.
Intraoperative complications were defined as neurovascular injury (significant disturbance of movement or sensation of the operated leg; intervention by a vascular surgeon required) and femoral fracture. Postoperative complications were defined as cup malposition, dislocation, aseptic loosening, periprosthetic joint infection and reoperation for any reason.
Cup malposition was defined as: 1) the acetabular cup was superiorly placed (the inferior border of the acetabular cup above the bilateral teardrops’ connecting line was more than 1 cm); 2) the acetabular cup was excessively medialized (the cup broke through the acetabular medial wall by more than 0.5 cm); or 3) the acetabular cup was excessively lateralized (the cup was located in the femoral head or its medial border was more than 0.5 cm away from the acetabular medial wall). If any of the above conditions were met, the acetabular cups were regarded as malpositioned.
To assess intraobserver and interobserver variations, these measurements (position of the acetabular cup, LLD and offset) were initially performed in a random order independently by two trained joint surgery residents (KXP and YMZ), who then took the measurements again after 2 weeks without knowing the first values. The final result was the average of four values. When the two residents disagreed on cup malposition, the decision was made by the senior surgeon (CW).
Statistical Analysis
All statistical analyses were performed utilizing SPSS version 22 (IBM Corp., Armonk, NY, USA). Measurement data are shown as the mean, standard deviation and extreme values (range). Measurement data were analyzed by the Student’s t-test or rank-sum test. Categorical data were analyzed by Fisher’s exact test and the chi-squared test. The intraobserver and interobserver agreements were calculated by the interclass correlation coefficient (ICC). A value of α=0.05 was applied to all tests.
Results
There were no significant differences in demographics between the two groups (Table 1).
 |
Table 1 Comparison of the Preoperative Clinical Data Between the Two Groups |
The intraobserver and interobserver agreements were found to have nearly perfect reliability for all of the measurements (ICC>0.81). The results are shown in Table 2.
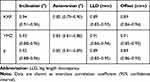 |
Table 2 Intraobserver and Interobserver Variations of Measurements |
There were no significant differences in the operating time, anteversion, inclination, LLD, offset-D, LOH and HHS between the two groups (Table 3).
 |
Table 3 Comparison of the Intraoperative and Postoperative Clinical Data Between the Two Groups |
The robotic procedures of registration, reaming and cup implantation did not prolong the operation. Instead, the fluoroscopic times in the robot group was significantly shorter than that in the control group (0.47±0.61 vs 2.16±1.61, respectively, p=0.000), which meant that intraoperative fluoroscopy was needed more in manual THA than in robot-assisted THA for arthrodesed hips. Therefore, when robot-assisted THA was applied in arthrodesed hips for AS patients, the operating time was comparable to manual THA, and the duration of intraoperative fluoroscopy was significantly reduced.
Two acetabular cups in the robot group and 12 acetabular cups in the control group were outside the safe zone. Although the anteversion and inclination did not differ significantly between the two groups, the percentage of acetabular cups in the safe zone was significantly higher in the robot group than in the control group (94.29% vs 67.57%, respectively, p=0.004). In addition, the anteversion in the robot-assisted THA had a smaller range than in the manual THA, although the difference was not significant (Figure 8).
 |
Figure 8 Box-plot of inclination and anteversion in robot-assisted THA and manual THA (○ means abnormal value and * means outlier). |
The total incidence of perioperative complications in the robot group was significantly lower than in the control group (5.71% vs 56.76%, respectively, p=0.000). There were six hips with cup malposition in the control group, which was more than in the robot group, although the difference was not significant (16.22% vs 0%, respectively, p=0.086) (Table 4). The robot showed a trend toward finding the real acetabulum and improving the cup positioning. In the control group, all three fractures were a mild split of the femoral calcar during stem implantation and were treated with wire binding.
 |
Table 4 Comparison of the Incidence of Perioperative Complications Between the Two Groups |
The anteversion of left cups was significantly larger than that of the right side in the control group (21.14±7.86 vs 16.00±6.32, respectively, p=0.042). In the robot group, there were no significant differences in anteversion or inclination between the two sides (Table 5).
 |
Table 5 Comparison of the Orientation of the Acetabular Cup on Different Sides Between the Two Groups |
Discussion
Hip arthrodesis in the extended position can cause great inconvenience to the affected patients. These patients cannot sit or bend, which makes their quality of life extremely poor. THA is the most successful treatment to restore the mobility of the hip joint and improve patients’ social life. However, the conversion of arthrodesed hips to replacement hips poses huge challenges for surgeons.12,21-24
In 1975, Brewster first reported that the challenges included patient positioning, exposure and identification of anatomical landmarks, component placement, restoration of limb length and stability.25 The surgical difficulties can be divided into several aspects. First, the rigid spine and pelvis, which was an unreliable reference, would cause cup malposition and dislocation.3 Secondly, the blind in-situ osteotomy of the femoral neck might result in injuring the acetabular wall and neurovascular structure. Thirdly, the boundary between the acetabulum and femoral head was difficult to discern. It was easy to implant the cup within the femoral head. Fourthly, severe osteoporosis would increase the risk of periprosthetic fracture.
The adoption of robots in THA has been reported previously to improve component positioning.26–29 Considering the clinical benefits of robot-assisted surgery, some surgeons recommended applying robots in complex hip replacement.9,14
This study is the first report on robot-assisted THA in arthrodesed hips. In our cohort, robot-assisted THA demonstrated significant advantages in reducing perioperative complications and improving cup positioning. Although the anteversion or inclination between the two groups showed no significant difference, the robot could increase the proportion of acetabular cups within the safe zone. The robot could also follow the surgical plan accurately and reduce the incidence of cup malposition in vertical and horizontal orientations. The incidences of dislocation between robot-assisted THA and manual THA were not significantly different, which may have been influenced by the small sample size and short follow-up.
One previous study in our institute reported that even for experienced surgeons, individual handedness was likely to be a contributory factor to cup orientation.30 In this study, we found similar results. For the manual THA, which was undertaken by a right-handed surgeon, cup positioning by the dominant hand was more accurate than that by the non-dominant side. Furthermore, there was less variability in acetabular cups on the dominant side, regardless of the anteversion or inclination. For the robot-assisted THA, no significant differences in the orientation of cups between the two sides were found. Thus, the robot could eliminate the effect of the surgeon’s handedness on cup positioning in THA.
Compared to common cases of hip replacement, the advantages of using a robot may be more significant in arthrodesed hips. The advantages are embodied in two aspects: the accurate preoperative surgical plan and the high implementation rate of the surgical plan. First, the three-dimensional template can more precisely determine the size and position of acetabular cups. Secondly, the preoperative plan can be more accurately replicated during the operation by the robotic system. These two functions contributed significantly to the clinical superiority of robot-assisted THA in this study.
Of course, the realization of these advantages depended on the surgeons’ experience. The robot could only copy, not create, the surgical plan. The surgeons had the main effect on the surgical effectiveness and safety of the semi-automatic robot. Exposure, osteotomy and management of complications remained manual work in THA for arthrodesed hips.
This study had several limitations. First, the study design was retrospective and the sample size was small. The prospectively constructed joint registry system and the automatic saving robotic software could ensure the authenticity of the data to some extent. This study enrolled the rare cases with arthrodesed hips, and its sample size was the largest among similar studies.9,15 Secondly, the follow-up time was relatively short and longer observation was needed to evaluate the long-term clinical outcomes. Thirdly, the measurements of the acetabular cup were based on X-rays. However, measurements based on radiography have been proved to have excellent correlation with CT scans.31–33 Fourthly, this study did not take the spine–pelvic parameters into consideration in the surgical plans.
Conclusion
Compared with manual THA for arthrodesed hips, robot-assisted THA had significant advantages in improving the frequency of achieving cup positioning within the target zone, with diminished radiation dose and no increase in operating time.
Data Sharing Statement
The data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The medical ethics committee of Chinese PLA General Hospital has approved the study. All procedures were conducted in compliance with the guidelines of the Declaration of Helsinki. Written informed consent was obtained from patients prior to their participation in the study. We have obtained consent for publication. Wei Chai and Xiangpeng Kong are co-first authors for this study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was funded by the Beijing Municipal Natural Science Foundation (L182063).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Taurog JD, Chhabra A, Colbert RA, Longo DL. Ankylosing spondylitis and axial spondyloarthritis. N Engl J Med. 2016;374:2563–2574. doi:10.1056/NEJMra1406182
2. Raychaudhuri SP, Deodhar A. The classification and diagnostic criteria of ankylosing spondylitis. J Autoimmun. 2014;48–49:128–133. doi:10.1016/j.jaut.2014.01.015
3. Blizzard DJ, Penrose CT, Sheets CZ, et al. Ankylosing spondylitis increases perioperative and postoperative complications after total hip arthroplasty. J Arthroplasty. 2017;32:2474–2479. doi:10.1016/j.arth.2017.03.041
4. Tang WM, Chiu KY. Primary total hip arthroplasty in patients with ankylosing spondylitis. J Arthroplasty. 2000;15:52–58. doi:10.1016/S0883-5403(00)91155-0
5. Ward MM. Complications of total hip arthroplasty in patients with ankylosing spondylitis. Arthritis Care Res (Hoboken). 2019;71:1101–1108. doi:10.1002/acr.23582
6. Khan MA. Total hip arthroplasty in ankylosing spondylitis. J Rheumatol. 2002;29:
7. Joshi AB, Markovic L, Hardinge K, et al. Total hip arthroplasty in ankylosing spondylitis: an analysis of 181 hips. J Arthroplasty. 2002;17:427–433. doi:10.1054/arth.2002.32170
8. Sochart DH, Porter ML. Long-term results of total hip replacement in young patients who had ankylosing spondylitis. Eighteen to thirty-year results with survivorship analysis. J Bone Joint Surg Am. 1997;79(8):1181–1189. doi:10.2106/00004623-199708000-00010
9. Kim YL, Shin SI, Nam KW, et al. Total hip arthroplasty for bilaterally ankylosed hips. J Arthroplast. 2007;22:1037–1041. doi:10.1016/j.arth.2007.03.027
10. Idulhaq M, Park KS, Diwanji SR, et al. Total hip arthroplasty for treatment of arthrodesed hip with 90 degrees flexion deformity. J Arthroplasty. 2010;25:
11. Morsi E. Total hip arthroplasty for arthrodesed hips; planning and techniques. J Arthroplast. 2007;22:871–875. doi:10.1016/j.arth.2006.09.003
12. Milone MT, Schwarzkopf R, Meere PA, et al. Rigid patient positioning is unreliable in total hip arthroplasty. J Arthroplasty. 2017;32:1890–1893. doi:10.1016/j.arth.2016.12.038
13. Della Valle AG, Shanaghan K, Benson JR, et al. Pelvic pitch and roll during total hip arthroplasty performed through a posterolateral approach. A potential source of error in free-hand cup positioning. Int Orthop. 2019;43:1823–1829. doi:10.1007/s00264-018-4141-2
14. Padgett DE. Simplifying the hip-spine relationship for total hip arthroplasty: what do i need to do differently intraoperatively? J Arthroplasty. 2019;34:S71–S73. doi:10.1016/j.arth.2019.01.003
15. Dabir S, Ramanath S, Shah H, et al. Surgical technique and outcome of uncemented THR using HA coated stems in arthrodesed and deformed hips due to ankylosing spondylitis. Hip Int. 2015;25:142–145. doi:10.5301/hipint.5000197
16. Domb BG, El Bitar YF, Sadik AY, et al. Comparison of robotic-assisted and conventional acetabular cup placement in THA: a matched-pair controlled study. Clin Orthop Relat Res. 2014;472:329–336. doi:10.1007/s11999-013-3253-7
17. Elson L, Dounchis J, Illgen R, et al. Precision of acetabular cup placement in robotic integrated total hip arthroplasty. Hip Int. 2015;25:531–536. doi:10.5301/hipint.5000289
18. Gupta A, Redmond JM, Hammarstedt JE, et al. Does robotic-assisted computer navigation affect acetabular cup positioning in total hip arthroplasty in the obese patient? A comparison study. J Arthroplasty. 2015;30:2204–2207. doi:10.1016/j.arth.2015.06.062
19. Restrepo C, Parvizi J, Kurtz SM, et al. The noisy ceramic hip: is component malpositioning the cause? J Arthroplasty. 2008;23:643–649. doi:10.1016/j.arth.2008.04.001
20. Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. doi:10.2106/00004623-197860020-00014
21. Bhan S, Eachempati KK, Malhotra R. Primary cementless total hip arthroplasty for bony ankylosis in patients with ankylosing spondylitis. J Arthroplasty. 2008;23:859–866. doi:10.1016/j.arth.2007.07.014
22. Wang W, Huang G, Huang T, et al. Bilaterally primary cementless total hip arthroplasty in patients with ankylosing spondylitis. BMC Musculoskelet Disord. 2014;15:344. doi:10.1186/1471-2474-15-344
23. Feng D-X, Zhang K, Zhang Y-M, et al. Bilaterally primary cementless total hip arthroplasty for severe hip ankylosis with ankylosing spondylitis. Orthop Surg. 2016;8:352–359. doi:10.1111/os.12254
24. Beverland DE, O’Neill CKJ, Rutherford M, et al. Placement of the acetabular component. Bone Joint J. 2016;null:37–43. doi:10.1302/0301-620X.98B1.36343
25. Brewster RC, Coventry MB, Johnson EW. Conversion of the arthrodesed hip to a total hip arthroplasty. J Bone Joint Surg Am. 1975;57:27–30. doi:10.2106/00004623-197557010-00005
26. Kanawade V, Dorr LD, Banks SA, et al. Precision of robotic guided instrumentation for acetabular component positioning. J Arthroplasty. 2015;30:392–397. doi:10.1016/j.arth.2014.10.021
27. Werner SD, Stonestreet M, Jacofsky DJ. Makoplasty and the accuracy and efficacy of robotic-assisted arthroplasty. Surg Technol Int. 2014;24:302–306.
28. Jacofsky DJ, Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016;31:2353–2363. doi:10.1016/j.arth.2016.05.026
29. Tarwala R, Dorr LD. Robotic assisted total hip arthroplasty using the MAKO platform. Curr Rev Musculoskelet Med. 2011;4:151–156. doi:10.1007/s12178-011-9086-7
30. Song X, Ni M, Li H, et al. Is the cup orientation different in bilateral total hip arthroplasty with right-handed surgeons using posterolateral approach? J Orthop Surg Res. 2018;13:123. doi:10.1186/s13018-018-0789-y
31. Lu M, Zhou Y-X, Du H, et al. Reliability and validity of measuring acetabular component orientation by plain anteroposterior radiographs. Clin Orthop Relat Res. 2013;471:2987–2994. doi:10.1007/s11999-013-3021-8
32. Nho J-H, Lee Y-K, Kim HJ, et al. Reliability and validity of measuring version of the acetabular component. J Bone Joint Surg Br. 2012;94:32–36. doi:10.1302/0301-620X.94B1.27621
33. Shin WC, Lee SM, Lee KW, et al. The reliability and accuracy of measuring anteversion of the acetabular component on plain anteroposterior and lateral radiographs after total hip arthroplasty. Bone Joint J. 2015;null:611–616. doi:10.1302/0301-620X.97B5.34735
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

