Back to Journals » Nature and Science of Sleep » Volume 13
Risk Factors for Sleepiness at the Wheel and Sleep-Related Car Accidents Among Patients with Obstructive Sleep Apnea: Data from the French Pays de la Loire Sleep Cohort
Authors Sabil A, Bignard R, Gervès-Pinquié C, Philip P, Le Vaillant M, Trzepizur W, Meslier N , Gagnadoux F
Received 10 July 2021
Accepted for publication 24 September 2021
Published 5 October 2021 Volume 2021:13 Pages 1737—1746
DOI https://doi.org/10.2147/NSS.S328774
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
AbdelKebir Sabil,1 Remi Bignard,2 Chloé Gervès-Pinquié,3 Pierre Philip,4 Marc Le Vaillant,3 Wojciech Trzepizur,2 Nicole Meslier,2 Frédéric Gagnadoux2
1Clinical Research Department, Cloud Sleep Lab, Paris, France; 2Department of Respiratory and Sleep Medicine, University Hospital of Angers, Angers, France; 3Biostatistics Department, Pays de la Loire Respiratory Health Research Institute, Beaucouzé, France; 4Sleep, Attention and Neuropsychiatry Unit, University of Bordeaux, CNRS, SANPSY USR 3413, and CHU Pellegrin, Bordeaux, France
Correspondence: AbdelKebir Sabil
Clinical Research Department, Cloud Sleep Lab, 29 rue Louis Braille, Paris, France
Tel +33 648 01 00 21
Email [email protected]
Purpose: We aimed to determine the risk factors of sleepiness at the wheel among patients with obstructive sleep apnea (OSA) and to determine factors that were independently associated with reported sleep-related near-miss accidents or car accidents.
Patients and Methods: This retrospective study was conducted on 843 OSA patients from the French Pays de la Loire sleep cohort database. Each patient completed surveys including anthropometric data, medical history, professional status, and data on alcohol and tobacco use. Epworth sleepiness scale (ESS) and sleep quality questionnaires were administered. Regarding driving, data were collected on occurrence of sleepiness-related near-misses or car accidents, and on distance driven per year. The primary dependent variable of interest was reported sleepiness at the wheel.
Results: On multivariable regression analysis, reported sleepiness at the wheel (n=298) was independently associated with younger age (p=0.02), male gender (p=0.009), marked nocturnal hypoxemia (p=0.006), lower BMI (p=0.03), absence of cardiovascular disease (p=0.022), executives or high degree jobs (p=0.003) and reported difficulty-maintaining sleep (p=0.03). Only past experience of sleepiness at the wheel (OR 12.18, [6.38– 23.25]) and an ESS ≥ 11 (OR 4.75 [2.73– 8.27]) were independently associated with reported car accidents (n=30) or near-miss accidents (n=137).
Conclusion: In patients newly diagnosed with OSA, the risk of car accident seems multifactorial, and its evaluation should include multiple parameters such as patient self-reported sleepiness at the wheel, occurrence of sleepiness-related accidents, anthropometry, professional status, and insomnia complaints. Thus, it is possible to evaluate this risk and advise patients as early as the first visit at the sleep medicine clinic without waiting for the results of the sleep study.
Keywords: sleepiness, accidents, near-miss accidents, French drivers, OSA, early risk prediction
Introduction
Sleepiness at the wheel is the second most common risk factor for car accidents after alcohol consumption, causing many deaths and injuries as well as high social and economic costs.1 In 2018, the World Health Organization reported that 1.35 million people die every year due to road accidents.2 Roughly 16% to 20% of all traffic accidents and 29% to 50% of deaths and serious injuries related to motor vehicles are thought to be associated with sleepiness at the wheel.3 The proportion of crashes caused by sleepiness at the wheel have been reported to vary substantially between countries, possibly due to geographical differences imposing greater exposure to long and monotonous driving. A 2017 meta-analysis showed that drowsy driving increases the risk of having a traffic accident by 2.5 times.4 In the USA, the Centers for Disease Control and Prevention found that an estimated 4% of adult drivers (>18 years old) reported having fallen asleep while driving in the previous 30 days.5 A survey in New Zealand found that sleep problems were more prevalent among accident-involved drivers.6 In the UK, it was reported that 29% of drivers admitted having felt close to falling asleep at the wheel in the previous twelve-month period.7
Defined as an intermediate state between wakefulness and sleep, sleepiness at the wheel has been compared to the effects caused by alcohol. Driving after a sleepless night is equivalent to driving with a 0.9 g/L of blood alcohol content,8 a level that is illegal in all European Union countries.9 Sleepiness at the wheel is caused by sleep deprivation, poor sleep quality, circadian rhythm sleep-wake disorders such as shift work disorder or by sedative substance intake.10–12
Obstructive sleep apnea is highly prevalent, with recent general population studies indicating that 20% to 30% in men and 10% to 15% in women have moderate or severe sleep-disordered breathing.13,14 Excessive daytime sleepiness (EDS), a major symptom of OSA, is reported in approximately 25% to 50% of OSA patients15 and studies have shown that EDS while driving is an important factor in road accidents or work-related accidents.13,16 While OSA has been recognized by the European Respiratory Society (ERS) as a risk factor for road accidents,13 there is still uncertainty about the relative importance of OSA severity indices of OSA, and the degree of sleepiness as a risk factor for accidents. Given the high heterogeneity of OSA in terms of clinical presentation, treatment response and outcomes,17–19 assessing the risk of accident during the initial diagnosis, constitutes a major management issue for the clinician.
Thus, the main objective of our study was to determine the risk factors of sleepiness at the wheel among OSA patients in a French sleep cohort.20 Secondary objectives of our study were to determine in this French cohort population: 1) the association of sleepiness at the wheel with reported sleep-related car accidents or near-miss accidents, and 2) the factors that were independently associated with reported car accidents or near-miss accidents.
Materials and Methods
Study Design
This retrospective study was conducted on the Pays de la Loire sleep cohort database. As previously described,20 this multicenter clinic-based French cohort has been recruiting patients ≥ 18 years investigated for suspected OSA. Patients with mild-to-severe OSA (apnea-hypopnea index [AHI] ≥5 events/h), diagnosed between 2007 and 2017 at the Sleep Medicine Center of the University Hospital of Angers, were included in this study. Patients with learning difficulties, who were unable to fill in the questionnaires, or read and/or speak French, patients with neuromuscular diseases or chronic respiratory failure, and those without a driver license were excluded from the cohort. Approval was obtained from the University of Angers Ethics Committee and the “Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le domaine de la Santé (C.C.T.I.R.S.)” (07.207bis). All patients had given their written informed consent at the time of their enrollment. The database complies with the restrictive requirements of the “Commission Nationale Informatique et Liberté (C.N.I.L.)” and the French information technology and personal data protection authority.
Sleep Studies
Patients were investigated by polysomnography (PSG) or home sleep apnea testing (HSAT) according to pretest clinical probability of OSA,21 using CID102L8DTM and CID102LTM devices (CIDELEC, Sainte-Gemmes-sur-Loire, France), respectively, for PSG and HSAT. Recorded data included oronasal airflow, tracheal sounds and suprasternal pressure, chest and abdominal wall motion using respiratory inductance plethysmography belts, arterial oxygen saturation (pulse oximetry), body position and electrophysiological signals for sleep evaluation (for PSG only). However, only data, from the PSG and HSAT recordings, relevant to OSA severity, was explored for this study. Sleep stages and other sleep-related data were not analyzed as it was not available in patients investigated by HSAT. Respiratory events were scored manually using the AASM recommended criteria22 and the apnea hypopnea index (AHI) was included in the analysis. Indices of nocturnal hypoxemia included the 3% oxygen desaturation index (ODI), the percentage of sleep time (or recoding time for HSAT) with oxygen saturation (SaO2) < 90% (T90) and the hypoxic burden (HB) defined as the total area under the respiratory event-related desaturation curve, expressed in %min23 were included in our analysis as well.
Baseline Evaluation and Questionnaires
Each patient completed surveys including anthropometric data, medical history, and professional status according to a specifically designed and validated self-administered questionnaires from the “Institut National de la Statistique et des Etudes Economiques” (INSEE).20 Patients were asked to specify whether they were shift workers, and if so, to state their shift schedule. Data on clinical diagnosis of depression requiring drug treatment and data on alcohol and tobacco use were documented. The validated French version of the Epworth sleepiness scale24 (ESS) was used to assess EDS. In addition, subjects were asked about symptoms of insomnia (difficulty falling asleep, difficulty maintaining sleep and early morning awakening), and about sleep habits (sleep duration on workdays and sleep duration on non-workdays). The presence of sleepiness while driving was investigated by the following question: “Have you ever nodded off or fallen asleep while driving? “. For patients responding positively, they were asked to rate the frequency of this sleepiness, thus classifying sleepiness while driving into 5 categories: “almost every day,” “3 to 4 times/week,” “1 to 2 times/week,” “1 to 2 times/month,” “< 1 time/month”, and “never or almost never.” To align with published data available in the literature, we grouped the frequencies into 3 categories: “≥ 1 time/week”, “= 1 to 2 times/month”, and “< 1 time/month”.25 However, for our statistical analysis, the subjects were divided into 2 groups: patients with reported sleepiness at the wheel including the first 2 categories (≥1 time/month), and the third category (<1 time/month) as patients without reported sleepiness at the wheel. Regarding driving, the patients were asked two questions concerning the occurrence of sleep-related near misses or car accidents in the last year. A near-miss accident was defined as an event of limited impact, perceived by the subject as being at risk of an accident (eg, deviation from the lane, crossing a white line) but having caused no damage. An accident was defined as an event that caused injury and/or material damage. Finally, data on distance driven per year came from patients’ self-reported information through questionnaires.
Statistical Analyses
The primary dependent variable of interest was reported sleepiness at the wheel.
Patients with and without reported sleepiness at the wheel were compared using Chi-square test for categorical variables and 2-sample t-test for continuous variables. Variables were included in the multivariable regression analysis based upon a univariate analysis p value<0.25 and/or previous literature26 to determine variables independently associated with reported sleepiness at the wheel (model 1) and with reported car accidents or near-miss accidents (model 2). Results were expressed as mean (standard deviation, SD) and adjusted odds ratio (OR) (95% confidence intervals [CI]). A 2-tailed probability value < 0.05 was considered significant. A ROC curve analysis was also performed to determine the ESS threshold above which patients were at risk of road accidents or near-miss accidents. Statistical analyses were performed with SAS 9.4 software (SAS institute, Cary, NC).
Results
Study Population
Among 1014 eligible OSA patients from the Pays de la Loire sleep cohort, recruited at the Angers University Hospital, 171 were excluded due to missing data (n=96) or absence of driving license (n=75). The final sample size comprised 843 patients including 87 professional drivers. The studied patients were majority men (63%) with typical mild-to-severe OSA (mean (SD) apnea-hypopnea index [AHI] and ESS: 25.3 (23.3) events/h and 10.1 (5.2) respectively), with frequent obesity (mean (SD) body mass index [BMI]: 29.6 (6.6)), systemic hypertension (32.6%), diabetes (12.9%), cardiovascular diseases (16.2%) and diagnosed depression (25.6%).
Of the 843 subjects in our sample, 298 (35.3%) reported having fallen asleep or felt sleepy at the wheel in the past year. Frequency of sleepiness occurrence was homogeneously distributed with approximately 31.0% reporting sleepiness occurring at least once a week, 34.1% reporting sleepiness 1 to 2 times a month and 34.9% reporting sleepiness less than once a month. Finally, according to the patients’ self-reported information in this French cohort, the prevalence of sleep-related accidents was 3.6% and that of near-miss accidents was 16.2%.
Comparison of Patients with and without Reported Sleepiness at the Wheel
Table 1 presents the characteristics of the entire population, patients without and with incident reported sleepiness at the wheel. Patients reporting sleepiness at the wheel were more frequently younger (p=0.0005), men (p=0.0004), with lower BMI (p=0.0014), and less systemic hypertension (p=0.0346) and cardiovascular diseases (p=0.0135). Concerning professional activity, subjects who reported sleepiness at the wheel were more often active with a full-time job ≥ 35 hours/week (p<0.0002), the distribution of professional categories was different (p=0.0032) with an over-representation of company directors/executives and/or higher degree jobs (university professors, medical doctors, engineers, etc.), and a lower representation of employees and blue-collar workers. Shift workers were twice as many in the sleepy subjects (15.4%) compared to the non-sleepy subjects (8.5%) at the wheel (p=0.0026). There was no significant difference between patients with and without reported sleepiness at the wheel regarding the use of alcohol, hypnotics, antidepressants, and anxiolytics. Nocturnal sleep complaints (ie, Difficulty maintaining sleep) was more frequently reported (p=0.0054) in sleepy drivers compared to non-sleepy drivers. As expected, sleepy drivers had a significantly higher ESS score compared to non-sleepy subjects (12.9 (4.7) vs 8.5 (4.7)). However, there was no significant difference between sleepy and non-sleepy drivers regarding indices of OSA severity (AHI, ODI, T90 and hypoxic burden). Finally, drivers with sleepiness at the wheel drove longer distance compared to non-sleepy drivers (p<0.0001) with a significant difference in reported history of car accidents and near-miss accidents (<0.0001 for both).
 |
Table 1 Characteristics of the Entire Population, Patients without and with Incident Reported Sleepiness at the Wheel |
Multivariate Analysis of Variables Associated with Sleepiness at the Wheel
The Forest plot in Figure 1 illustrates logistic regression analysis of variables associated with reported sleepiness at the wheel. In model 1, the multivariate analysis was adjusted for confounding risk factors with p< 0.2526 as well as for depression (p< 0.26) because it is borderline in our study, and it is a well-known risk factor according to the literature.27–30 Our results show that sleepiness at the wheel is significantly associated with younger (OR [95% CI]: 0.72 [0.54–0.95]), male gender (OR 1.80 [1.16–2.79]), lower BMI (OR 0.77, [0.61–0.97]), driving longer distance per year (OR 1.73 [1.38–2.18]), reporting difficulty maintaining sleep (OR 1.57 [1.04–2.37]), and having a managerial or higher degree jobs (OR 2.04 [1.27–3.29]). Depression (OR 1.54, [0.99–2.39]) was borderline with p = 0.05. Conversely, patients with prevalent cardiovascular diseases were at lower risk of sleepiness at the wheel (OR 0.49 [0.27–0.88]). As the study population consisted of OSA patients, indices of OSA severity were independently entered in the multivariable analysis. Among all indices, only T90 was significantly associated with reported sleepiness at the wheel (OR 1.36 [1.09–1.70]). Because of its redundancy with sleepiness, the ESS variable was removed from our multivariate analysis in model 1. However, we investigated its impact on the analysis and when ESS was used, the insomnia factor, difficulty maintaining sleep, was no longer significant (data not shown).
Factors Associated with Reported Car Accidents or Near-Miss Accidents
As illustrated in Figure 2, the percentage of subjects with history of sleep-related near misses or car accidents was markedly higher in patients with reported sleepiness at the wheel compared to non-drowsy drivers (8.0 vs 1.0% for car accidents and 37.8 vs 3.8% for near-miss accidents; p<0.0001 for both). The threshold above which the risk of accidents and near-miss accidents becomes critical is ESS= 10.94. This threshold was determined with an AUC = 0.77, a 71% sensitivity and a 70% specificity (Figure 3).
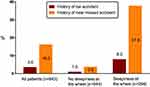 |
Figure 2 Percentage of subjects with history of car accidents or near-miss accidents in the entire population and in patients without and with reported sleepiness at the wheel. |
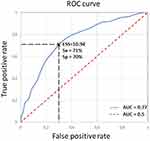 |
Figure 3 ROC analyses to determine the Epworth sleepiness scale threshold above which patients were at risk of car accidents or near-miss accidents. |
We further conducted a logistic regression analysis of factors associated with reported sleep-related accidents or near-miss accidents (model 2). Using variables from model 1 + ESS and reported sleepiness at the wheel, only ESS (OR 4.75 [2.73–8.27] for ESS≥11) and the presence of sleepiness at the wheel (OR 12.18, [6.38–23.25]) were associated with reported accidents or near-miss accidents (Table 2).
 |
Table 2 Logistic Regression Analysis to Determine Variables Independently Associated with Reported Car Accidents or Near-Miss Accidents (Model 2) |
Discussion
Within a large sample of typical OSA patients from a French sleep cohort investigated between 2007 and 2017, we found that 35% of subjects reported sleepiness at the wheel and almost 20% reported history of car accidents or near-miss accidents in the past year. Taking into consideration driving distance, we found that younger male patients with lower BMI, with no history of cardiovascular disease, with a managerial or higher degree jobs and reporting difficulty maintaining sleep were at higher risk of sleepiness while driving. Overall, nocturnal hypoxemia assessed by T90 was the only OSA severity index associated with reported sleepiness at the wheel. These findings, except for T90, could help identify OSA patients at risk for sleepiness at the wheel and car accidents as early as the first visit at the sleep medicine clinic and before sleep study results.
Our data show that one-third of OSA patients, from this French cohort, reports sleepiness while driving. This prevalence is in agreement with a recent French study of more than 50,000 subjects referred to the sleep clinic.31 In the general population, the prevalence of sleepiness at the wheel is usually lower, with 17% of Europeans reporting an episode of sleepiness at the wheel over the last two years32 and 28% of French drivers reporting a severe episode of sleepiness requiring a driving break over the last year.25 This difference may be explained by the nature of the sample and the way in which sleepiness at the wheel is assessed. A recent meta-analysis by Bioulac et al of 17 studies confirms a large variability between studies with prevalence ranging from 1.1% to 58%.4
Consistent with previous studies,32–34 our data show that males are more at risk to experience sleepiness while driving. Even when age, distance travelled and sleep disturbances are accounted for, the risk of falling asleep at the wheel remains higher for men comparing to women.34 The reasons for this difference are poorly documented, with few studies pointing to more aggressive and over confident driving among men, especially in younger subjects.35,36 Possibly, a higher prevalence of OSA among men could explain this higher risk.
Sleepiness at the wheel was also associated with younger age. This is consistent with other studies that have shown a clear increase in the risk of sleepy driving in young people.33,37 Philip et al provided an answer by studying reaction times. In the absence of sleep deprivation, reaction times were slower in older subjects. However, after sleep deprivation, reaction times in younger subjects increased while those in older subjects remained virtually unchanged.38 This implies a greater sensitivity to sleep debt in younger subjects. Furthermore, a significant proportion of young subjects continues to drive despite their increasing perception of sleepiness.39 Age was not independently associated with the risk of car accidents or near-miss accidents in our study, which included typical OSA patients with a relatively high mean age (60 years). However, this finding should be interpreted with caution due to the nature of our sample.
Our findings suggest that active professionals, and particularly executives and those with higher degree jobs, are more prone to sleepy driving than those who were retired or with blue-collar jobs. This category of workers is highly exposed to extended hours of work, anxiety, and stress symptoms which are all very real factors that can contribute to sleep deprivation and thus to sleepiness. The non-significance of the shift work in the multivariate analysis is probably due to the small number of shift workers in our studied cohort (n=89).
Our data also shows that difficulty maintaining sleep, a type of insomnia, was significantly associated with sleepiness at the wheel. By interviewing over five thousand insomniacs, Léger et al showed that 4% had had an accident related to sleepiness and that 9% had fallen asleep at the wheel in the last year.40 Moreover, according to a study on French highways, Quera-Salva et al showed that in 15 years, French drivers have reduced their sleep time, are more sleepy at the wheel and have seven times more near-miss accidents related to sleepiness.41
Our study revealed an association of sleepiness at the wheel with higher T90 which is in accordance with a recent study showing that obstruction duration, desaturation duration, and T90 had the strongest correlations with mean daytime sleep latency.42 Fanfulla et al also demonstrated that the severity of nocturnal hypoxia combined with reduced habitual sleep time and excessive daytime sleepiness, contributed to near-miss car accidents.27 Mendelson et al showed a positive association between nocturnal hypoxemia and daytime sleepiness.43
The Epworth score quantifies behavioral sleepiness in relatively passive situations requiring a low level of alertness (sitting and reading or watching television), whereas sleepiness at the wheel refers to a state requiring a high level of alertness. However, Powell et al44 and Sagaspe et al25 have shown an association between abnormal Epworth score (ESS ≥ 11) and near-miss accidents. Using a ROC curve analysis, we demonstrated that an Epworth score ≥ 11 is associated with an almost five-fold risk of car accidents and near-miss accidents. Our results also show that the risk is even higher (11.34 times) in OSA patients having experienced sleepiness at the wheel in the past. Thus, according to our results regarding OSA patients from this French cohort, an ESS ≥ 11 and chronic sleepiness at the wheel are the best predictors of car accidents and near-miss accidents in OSA patients. Consequently, a question about sleepiness while driving should be systematically associated with the assessment of daytime sleepiness to determine the ability to drive in OSA patients who are usually sleepy.
Finally, our study shows that reported sleepiness at the wheel is strongly associated with longer distance driving. This is probably because longer distance driving increases potential exposure to sleepiness at the wheel in these patients. However, when adjusted for confounders, the multivariate analysis regarding the risk of car accidents and near-miss accidents, driving distance was not a significant factor anymore. In fact, studies have shown that drowsy driving accidents occurred more often in the city (53.8%) and in short trips (84.6%).
Limitations and Biases
Our study has several limitations. Our sample concerns only OSA patients living in France and having consulted at a specific university hospital sleep center, introducing a selection bias, and making the extrapolation to the general population difficult. In addition, our data were collected retrospectively, which may introduce a bias in data collection. A large part of the data is declarative and is therefore exposed to recall bias. Furthermore, our investigation did not include any questions about countermeasures against sleepy driving. Nevertheless, these different biases are counterbalanced by an adjustment of confounding factors through multivariate analysis and inclusion of a relatively large number of subjects. These measures make the strengths of our study. Concerning sleepiness while driving, our study is one of the few to include clinical data as well as data from questionnaires and sleep study recordings, giving us a complete profile of OSA patients who are vulnerable to sleepiness while driving and are at risk of road accidents.
Conclusion
The studied population consisted of typical OSA patients that had been diagnosed with mild to severe sleep apnea syndrome. Given the high prevalence of excessive daytime somnolence in this population, the evaluation of sleepiness at the wheel and risk of road accidents is crucial as early as the first visit at the sleep medicine clinic. Our study has shown that the risk is not necessarily revealed through sleep study parameters but could mainly be recognized in other signs and factors that could easily be identified in OSA patients before the results of their sleep study that could be done many months after the initial visit in the sleep clinic.
Acknowledgments
The authors thank the IRSR, promoter of the cohorts from which the data for this study were obtained. We thank Julien Godey, Laetitia Moreno and Marion Vincent, sleep technicians in the Department of Respiratory and Sleep Medicine of Angers University Hospital.
Disclosure
Professor Pierre Philip reports personal fees, non-financial support from Jazz, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Dawson D, Reynolds AC, Van Dongen HPA, Thomas MJW. Determining the likelihood that fatigue was present in a road accident: a theoretical review and suggested accident taxonomy. Sleep Med Rev. 2018;42:202–210. doi:10.1016/j.smrv.2018.08.006
2. World Health Organization. Global status report on road safety 2018. World Health Organization; 2018.
3. Johnson KD, Patel SR, Baur DM, et al. Association of sleep habits with accidents and near misses in United States transportation operators. J Occup Environ Med. 2014;56:510–515. doi:10.1097/JOM.0000000000000132
4. Bioulac S, Micoulaud-Franchi J-A, Arnaud M, et al. Risk of motor vehicle accidents related to sleepiness at the wheel: a systematic review and meta-analysis. Sleep. 2017;40. doi:10.1093/sleep/zsx134
5. Wheaton AG, et al. Drowsy driving and risk behaviors - 10 states and Puerto Rico, 2011–2012. MMWR Morb Mortal Wkly Rep. 2014;63:557–562.
6. Gander PH, Marshall NS, Harris RB, Reid P. Sleep, sleepiness and motor vehicle accidents: a national survey. Aust N Z J Public Health. 2005;29:16–21. doi:10.1111/j.1467-842X.2005.tb00742.x
7. Maycock G. Sleepiness and driving: the experience of UK car drivers. J Sleep Res. 1996;5:229–237. doi:10.1111/j.1365-2869.1996.00229.x
8. Fairclough SH, Graham R. Impairment of driving performance caused by sleep deprivation or alcohol: a comparative study. Hum Factors. 1999;41:118–128. doi:10.1518/001872099779577336
9. Allsop R. Drink driving as the commonest drug driving-a perspective from Europe. Int J Environ Res Public Health. 2020;17:E9521. doi:10.3390/ijerph17249521
10. Garbarino S, Durando P, Guglielmi O, et al. Sleep apnea, sleep debt and daytime sleepiness are independently associated with road accidents. a Cross-Sectional Study on truck drivers. PLoS One. 2016;11:e0166262. doi:10.1371/journal.pone.0166262
11. Garbarino S, Nobili L, Beelke M, De Carli F, Ferrillo F. The contributing role of sleepiness in highway vehicle accidents. Sleep. 2001;24:203–206. doi:10.1093/sleep/24.2.1a
12. Moradi A, Nazari SSH, Rahmani K. Sleepiness and the risk of road traffic accidents: a systematic review and meta-analysis of previous studies. Transp Res Part F Traffic Psychol Behav. 2019;65:620–629. doi:10.1016/j.trf.2018.09.013
13. Bonsignore MR, Randerath W, Schiza S, et al. European respiratory society statement on sleep apnoea, sleepiness and driving risk. Eur Respir J. 2021;57:2001272. doi:10.1183/13993003.01272-2020
14. Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015;3:310–318. doi:10.1016/S2213-2600(15)00043-0
15. Bonsignore MR, Pepin JL, Cibella F, et al. Excessive daytime sleepiness in obstructive sleep apnea patients treated with continuous positive airway pressure: data from the European sleep apnea database. Front Neurol. 2021;12:690008. doi:10.3389/fneur.2021.690008
16. Garbarino S, Guglielmi O, Sanna A, Mancardi GL, Magnavita N. Risk of occupational accidents in workers with obstructive sleep apnea: systematic review and meta-analysis. Sleep. 2016;39:1211–1218. doi:10.5665/sleep.5834
17. Gagnadoux F, Le Vaillant M, Paris A, et al. Relationship between OSA clinical phenotypes and CPAP treatment outcomes. Chest. 2016;149:288–290. doi:10.1016/j.chest.2015.09.032
18. Mazzotti DR, Keenan BT, Lim DC, et al. Symptom subtypes of obstructive sleep apnea predict incidence of cardiovascular outcomes. Am J Respir Crit Care Med. 2019;200:493–506. doi:10.1164/rccm.201808-1509OC
19. Zinchuk A, Yaggi HK. Phenotypic subtypes of OSA. Chest. 2020;157:403–420. doi:10.1016/j.chest.2019.09.002
20. Gagnadoux F, Le Vaillant M, Goupil F, et al. Influence of marital status and employment status on long-term adherence with continuous positive airway pressure in sleep apnea patients. PLoS One. 2011;6:e22503. doi:10.1371/journal.pone.0022503
21. Meurice J-C, Gagnadoux F. [Recommendations for clinical practice in the management of obstructive sleep apnea syndrome in adults. Preface]. Rev Mal Respir. 2010;27 Suppl 3:S113–114. Catalan. doi:10.1016/S0761-8425(10)70016-4
22. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. deliberations of the sleep apnea definitions task force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8:597–619. doi:10.5664/jcsm.2172
23. Blanchard M, Gervès-Pinquié C, Feuilloy M, et al. Association of nocturnal hypoxemia and pulse rate variability with incident atrial fibrillation in patients investigated for obstructive sleep apnea. Ann Am Thorac Soc. 2021;18:1043–1051. doi:10.1513/AnnalsATS.202009-1202OC
24. Kaminska M, Jobin V, Mayer P, et al. The Epworth sleepiness scale: self-administration versus administration by the physician, and validation of a French version. Can Respir J. 2010;17:e27–34. doi:10.1155/2010/438676
25. Sagaspe P, Taillard J, Bayon V, et al. Sleepiness, near-misses and driving accidents among a representative population of French drivers. J Sleep Res. 2010;19:578–584. doi:10.1111/j.1365-2869.2009.00818.x
26. Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. Wiley; 2013; doi:10.1002/9781118548387
27. Fanfulla F, Pinna GD, Marrone O, et al. Determinants of sleepiness at wheel and missing accidents in patients with obstructive sleep apnea. Front Neurosci. 2021;15:656203. doi:10.3389/fnins.2021.656203
28. Philip P, Chaufton C, Orriols L, et al. Complaints of poor sleep and risk of traffic accidents: a Population-Based Case-Control Study. PLoS One. 2014;9:e114102. doi:10.1371/journal.pone.0114102
29. Jacobsen JH, Shi L, Mokhlesi B. Factors associated with excessive daytime sleepiness in patients with severe obstructive sleep apnea. Sleep Breath. 2013;17:629–635. doi:10.1007/s11325-012-0733-z
30. Koutsourelakis I, Perraki E, Bonakis A, et al. Determinants of subjective sleepiness in suspected obstructive sleep apnoea. J Sleep Res. 2008;17:437–443. doi:10.1111/j.1365-2869.2008.00663.x
31. Philip P, Bailly S, Benmerad M, et al. Self-reported sleepiness and not the apnoea hypopnoea index is the best predictor of sleepiness-related accidents in obstructive sleep apnoea. Sci Rep. 2020;10:16267. doi:10.1038/s41598-020-72430-8
32. Gonçalves M, Amici R, Lucas R, et al. Sleepiness at the wheel across Europe: a survey of 19 countries. J Sleep Res. 2015;24:242–253. doi:10.1111/jsr.12267
33. Akerstedt T, Kecklund G. Age, gender and early morning highway accidents. J Sleep Res. 2001;10:105–110. doi:10.1046/j.1365-2869.2001.00248.x
34. Phillips RO, Sagberg F. Road accidents caused by sleepy drivers: update of a Norwegian survey. Accid Anal Prev. 2013;50:138–146. doi:10.1016/j.aap.2012.04.003
35. Gregersen NP, Bjurulf P. Young novice drivers: towards a model of their accident involvement. Accid Anal Prev. 1996;28:229–241. doi:10.1016/0001-4575(95)00063-1
36. Massie DL, Campbell KL, Williams AF. Traffic accident involvement rates by driver age and gender. Accid Anal Prev. 1995;27:73–87. doi:10.1016/0001-4575(94)00050-V
37. Pack AI, Pack AM, Rodgman E, et al. Characteristics of crashes attributed to the driver having fallen asleep. Accid Anal Prev. 1995;27:769–775. doi:10.1016/0001-4575(95)00034-8
38. Philip P, Taillard J, Sagaspe P, et al. Age, performance and sleep deprivation. J Sleep Res. 2004;13:105–110. doi:10.1111/j.1365-2869.2004.00399.x
39. Nordbakke S, Sagberg F. Sleepy at the wheel: knowledge, symptoms and behaviour among car drivers. Transp Res Part F Traffic Psychol Behav. 2007;10:1–10. doi:10.1016/j.trf.2006.03.003
40. Léger D, Bayon V, Ohayon MM, et al. Insomnia and accidents: cross-sectional study (EQUINOX) on sleep-related home, work and car accidents in 5293 subjects with insomnia from 10 countries. J Sleep Res. 2014;23:143–152. doi:10.1111/jsr.12104
41. Quera-Salva MA, Hartley S, Sauvagnac-Quera R, et al. Association between reported sleep need and sleepiness at the wheel: comparative study on French highways between 1996 and 2011. BMJ Open. 2016;6:e012382. doi:10.1136/bmjopen-2016-012382
42. Kainulainen S, Töyräs J, Oksenberg A, et al. Severity of desaturations reflects OSA-related daytime sleepiness better than AHI. J Clin Sleep Med. 2019;15:1135–1142. doi:10.5664/jcsm.7806
43. Mendelson WB. The relationship of sleepiness and blood pressure to respiratory variables in obstructive sleep apnea. Chest. 1995;108:966–972. doi:10.1378/chest.108.4.966
44. Powell NB, Schechtman KB, Riley RW, et al. Sleepy driver near-misses may predict accident risks. Sleep. 2007;30:331–342. doi:10.1093/sleep/30.3.331
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

