Back to Journals » Infection and Drug Resistance » Volume 15
Risk Factors Associated with Methicillin Resistance in Hospitalized Newborn Infants with Staphylococcus aureus Infection
Authors Wei J, Wang Y, Chen C, Lin J
Received 30 March 2022
Accepted for publication 27 May 2022
Published 7 June 2022 Volume 2022:15 Pages 2921—2928
DOI https://doi.org/10.2147/IDR.S367912
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Jia Wei,1 Yin Wang,2 Chao Chen,3 Jing Lin4
1Department of Psychological Medicine, Children’s Hospital of Fudan University, National Children’s Medical Center, Shanghai, People’s Republic of China; 2Clinical trial unit, Children’s Hospital of Fudan University, National Children’s Medical Center, Shanghai, People’s Republic of China; 3Department of Neonatology, Children’s Hospital of Fudan University, National Children’s Medical Center, Shanghai, People’s Republic of China; 4Department of Pediatrics, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Correspondence: Jing Lin, Department of Pediatrics, Icahn School of Medicine at Mount Sinai, One Gustave Levy Place, New York, NY, 10029, USA, Tel +1-212-241-6186, Fax +1-212534-5207, Email [email protected]
Background: An increasing number of infections due to methicillin-resistant Staphylococcus aureus (S. aureus) have been reported worldwide. To explore the risk factors associated with methicillin-resistance among the neonates with confirmed S. aureus infections and thereby to help selection of appropriate empirical antibiotics.
Methods: We compared a group of hospitalized neonates with culture confirmed methicillin-resistant S. aureus (MRSA) infections to a group with methicillin-sensitive S. aureus (MSSA) based on antimicrobial susceptibility reports. We used multivariable regression analysis to determine the risk factors for neonatal MRSA infections.
Results: There was no difference in the ratio of local to systemic infections or mortality between the two groups. However, the total hospitalization days and the medical care expenses in the MRSA group were significantly increased when compared to that of the MSSA group. Prior use of antibiotics for more than 48 hours was an independent risk factor for neonatal acquisition of MRSA infections, while exclusive breast milk feeding was a protective factor against MRSA infections.
Conclusion: Restrictions on antibiotic abuse and promotion of breast milk feeding may protect newborns from MRSA infections. Prior history of antibiotic use and exclusive breast milk feeding may be important factors to consider in the selection of appropriate empirical antibiotics for use in neonates prior to the availability of the results of antimicrobial susceptibility testing.
Keywords: neonates, methicillin-resistant Staphylococcus aureus, protective factor, empirical antibiotics
Introduction
Staphylococcus aureus (S. aureus) is one of the most common gram-positive pathogens causing neonatal infections.1 In the last decades, an increasing number of infections due to methicillin-resistant S. aureus (MRSA) have been reported worldwide, especially in developing countries. In Asia, more than half of the S. aureus infections in neonates were found to be resistant to methicillin.2 We have shown previously that MRSA accounted for 59.8% of all S. aureus bloodstream isolates in Chinese NICUs.3 Neonatal infections due to S. aureus, especially MRSA, continue to be a major cause of neonatal fatality and increased medical expenditure.4,5
Neonates are at high-risk for S. aureus infection because of their immature skin and mucosal defense functions, and the high frequency of invasive procedures during hospitalization. To reduce neonatal mortality caused by bacterial infection, when infection is suspected, it is vital to select appropriate empirical antibiotics prior to the availability of culture and antimicrobial susceptibility results, generally avoiding the unnecessary use of broad-spectrum antibiotics. Furthermore, once preliminary culture results are available, it may take up to one or two additional days before the final antimicrobial susceptibility is determined. Therefore, the first-line empirical antibiotic regimen should be selected based on the most common local pathogens and their historical antimicrobial sensitivity patterns. In the current study, we compared the clinical characteristics of a group of hospitalized neonates with culture confirmed MRSA infection with a group infected with methicillin-sensitive S. aureus (MSSA) in order to determine the potential risk factors for MRSA infection among the neonates with confirmed S. aureus infections. These results may inform the selection of appropriate empirical antibiotics before the antimicrobial susceptibility results in the future.
Materials and Methods
Data Collection
This was an observational retrospective cohort study which included newborn infants who were admitted into The Children’s Hospital of Fudan University, a National Children’s Medical Center in Shanghai, China, from 2012 to 2018. The Department of Neonatology, Children’s Hospital of Fudan University, is one of the largest neonatology departments in China, responsible for receiving critically ill neonates in the Yangtze River Delta region of China and even the whole country. Neonates requiring mechanical ventilation, surgery, or more complex interventions are frequently transferred to our neonatal unit. All cultures which grew S. aureus were identified through our hospital database, and those from blood, cerebrospinal fluid or infected tissue drainage (eg pustules, abscesses, purulent discharge from the umbilical cord) were included for analysis. Detailed clinical data were retrieved from medical records. If the patient had multiple culture positive for S. aureus during the hospitalization, only the first result was included to avoid over-representation. Cases with culture specimen sources from sputum, rectal swabs, and other specimen sources (eg Urine, nasal swab, skin, throat swab) which were most likely due to colonization were considered as colonization and excluded for analysis. Cases with incomplete data were also excluded. Cases with culture confirmed S. aureus infection were divided into an MRSA group and an MSSA group. Community-acquired S. aureus infection was defined as an isolate from either an outpatient, or an inpatient within 48 hours of hospitalization. Those were the babies who had been discharged home and admitted for a variety of reasons.
Hospital-acquired S. aureus infection was defined as culture taken >48 hours after admission. Prior use of antibiotics was defined as having been treated with intravenous antibiotics for more than 48 hours prior to the culture was taken. Transferred from OSH was defined as neonates who were transferred from another hospital to our hospital for further treatment. A waiver for parental consent to review medical records was granted by the Institutional Ethics Committee. Confidential handling of patient data followed the institutional rules strictly and were in compliance with the Declaration of Helsinki.
Bacterial Identification and Drug Susceptibility Testing
S. aureus strain identification was conducted using a MALDI-TOF/MS mass spectrometer (Bruck, Germany) or a VITEK-2 Compact automatic bacterial identification instrument (Mérieux, France). The screen for MRSA and MSSA was either by cefoxitin paper method (30ug, British OXOID) or oxacillin MIC method (AST GP67 Gram-positive bacteria drug sensitivity test card, Mérieux, France). The results were interpreted following the recommendations and definitions of the Clinical and Laboratory Standards Institute (CLSI, 2019). And the quality control strains adopt ATCC29213 and ATCC25923, which were obtained from the Clinical Laboratory Center of Shanghai.
Statistical Analysis
SPSS version 22 (SPSS, Inc., Chicago, Illinois) was used to perform the statistical analysis. Continuous variables were tested for normality using the Kolmogorov–Smirnov test. Non-normally distributed data were expressed by median (25–75 percentile), and the differences between groups were compared by the rank sum test. Categorical data were expressed as numbers or percentages and were analyzed by using the Chi-square test or Fisher’s exact test. Multivariable logistic regression was conducted to determine the risk factors associated with infection by a methicillin resistant strain in neonates with confirmed S. aureus infection. Factors with P < 0.1 in univariate analysis were included in multivariable logistic regression analysis. Before we put these variables into the multivariable logistic regression model, we made a variance inflation factor (VIF), and then all of its VIF are less than 10, indicating that all variables did not have collinearity. Odds ratio (OR) with 95% confidence interval (95% CI) was presented. P < 0.05 was considered statistically significant. The goodness-of-fit test of risk factors adopts the Hosmer and Lemeshow test. When P > 0.05, it is believed that the risk factors can fit the sample data.
Results
During the study period, a total of 1468 S. aureus isolates were identified from specimens sent from our Neonatal Units. Specimens were predominantly from sputum, blood, pus, urine, mucous, and skin swabs. The proportion of MRSA in all S. aureus isolates from 2012 to 2018, presented in Figure 1, increased until 2016 when it peaked at 36.8%. After that, the proportion of MRSA decreased gradually and was down to 29.6% in 2018.
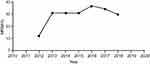 |
Figure 1 The proportion of MRSA in all S. aureus isolates from 2012 to 2018. |
After a careful review of the 1468 isolates of S. aureus from specimens from newborns, we identified 170 which represented clinical significant infection rather than colonization. Six cases were excluded due to incomplete data, leaving 164 cases that were included for analysis. Among those, 49 were infected with MRSA and 115 were infected with MSSA as the diagram shown in Figure 2. The proportion of MRSA in all S. aureus infection was 29.9%, which is similar to the overall proportion of MRSA in all S. aureus isolates shown in the Figure 1.
 |
Figure 2 Screening flowchart of research objects. |
Comparisons of the basic clinical characteristics between the two groups are presented in Table 1. As shown in the table, there were no statistically significant differences in gender, birth weight, gestational age, mode of delivery, multiple birth, maternal preeclampsia, maternal chorioamnionitis, infant of diabetic mother (IDM), and history of surgeries between the MRSA group and the MSSA group. However, when compared to the MSSA group, the MRSA group had fewer on exclusive breast milk feeding, more with a history of prior antibiotics use for more than 48 hours, and with an older age and longer hospitalization days prior to infection (P < 0.01). Furthermore, the proportion of babies transferred from outside hospitals (OSH) and those with central lines were significantly higher in MRSA group (P < 0.05). Community acquired infections appeared to be more often seen in the MSSA group, and the rate of mechanical ventilations including CPAP was higher in the MRSA group, but neither has reached a statistical significance with univariate analysis (P > 0.05).
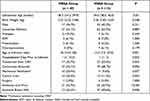 |
Table 1 The Basic Clinical Characteristics Between the Two Groups |
Since the infection site or infection type is closely related to the prognosis of patients, the types of S. aureus infection and outcomes were compared between the two groups. As shown in Table 2, there was no difference in the ratio of local to systemic infection between the two groups (p > 0.05). Looking into the specific types of infection, other than that the MSSA group had higher percentage of skin infections, there were no percentage differences in other types of infection between the MRSA group and the MSSA group. There was no statistically significant difference in mortality between the two groups (P = 0.887). However, the total hospitalization days and the medical care expenses in the MRSA group were significantly higher than those of the MSSA group (P < 0.01).
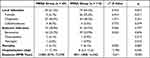 |
Table 2 Comparison of Infection Sites and Clinical Outcomes Between the Two Groups |
To determine the risk factors associated with methicillin-resistant strain in newborns with S. aureus infection, a multivariable logistic regression analysis was performed. All associated variables with P < 0.1 in the univariate analysis were included into the model. As shown in Table 3, the prior use of antibiotics for more than 48 hours was an independent risk factor for methicillin resistance in hospitalized newborn infants with S. aureus infection (OR = 3.939, 95% CI:1.460–10.625, P = 0.007), while exclusive breast milk feeding was a protective factor against MRSA infection (OR = 0.365, 95% CI:0.164–0.814, P = 0.014). None of the other variables were statistically significant in the multivariable regression model.
 |
Table 3 Multivariate Regression Analysis of Risk Factors for MRSA Infection |
Discussion
Although numerous antibiotics have been developed to overcome the challenge presented by pathogenic bacteria, infection with S. aureus, especially MRSA, in newborns remains an important problem faced by clinicians.6 In hospitalized newborn infants, whenever S. aureus infections are suspected, appropriate selection of empirical antibiotics is very important to improve the prognosis. Previous studies have shown that the incidence of MRSA correlates with the neonates’ history of having received medical therapy.7,8 In the current study, we collected data of hospitalized neonates with S. aureus infection, and analyzed the risk factors associated with MRSA infection among the neonates with confirmed S. aureus infection. We demonstrate that prior antibiotic usage is a strong and independent risk factor for methicillin resistance of S. aureus isolated from a neonate, while exclusive breast milk feeding is a protective factor against methicillin resistance.
An increasing number of MRSA are being isolated as the pathogens in neonatal infections in China.3 The current study from one of the largest children’s medical centers in China suggests that the proportions of MRSA in either S. aureus colonization or serious infection are about 30%. When the clinical differences between the MRSA and MSSA infections were compared, we found that neonates in the MRSA group had longer length of hospitalization days prior to the onset of infection, higher chance of being transferred from OSH, more with central lines, higher percentage of CPAP or mechanical ventilation, and more with prior antibiotic use. As the results, the treatment of MRSA group was associated with higher total expenses for hospitalization, although no significant differences were found in overall infection types as well as mortality between the two groups.
Several factors that were significantly different between the MRSA and MSSA groups by using univariate analysis were confounding factors. Using a multivariable regression analysis, we found that prior use of antibiotics for more than 48 hours was the only independent risk factor for methicillin resistance in hospitalized newborn infants with S. aureus infection. S. aureus is an opportunistic pathogen,9 which is a conditional pathogen that causes infection when human immune function is low or disturbed. The use of antibiotics may act as a selective factor, increasing the risk of infection of resistant strains. The abuse of antibiotics in China has been relatively serious in the past decades, resulting in an increasing rate of MRSA colonization and infection.10,11 In recent years, the country began to pay attention to the abuse of antibiotics, and antibiotic stewardship is being implemented in our hospital. Possibly as a result, the MRSA proportion of S. aureus isolates has peaked as demonstrated in our data. However, the incidence of community-related MRSA infections worldwide continues to gradually increase, so restrictions on the unnecessary use of antibiotics require more effort.12–14
Our data demonstrate that exclusive breast milk feeding is a protective factor against MRSA infection. Our results are consistent with the recent findings by others that breastfeeding is an independent preventive factor for MRSA colonization and that MRSA colonization is an independent risk factor for neonatal MRSA infection.15,16 In addition to essential nutrients, breast milk also contains a wide range of immune cells and bioactive ingredients with anti-inflammatory, anti-infection and probiotic effects.17,18 Breast milk can promote the development of a healthy infant microbiota and immune system through various mechanisms, prevent various infections and reduce the symptoms.19 Indeed, recent trials from both Finland20 and France21 have proven that breastfeeding is closely related to the reduction of antibiotic use, and there is an inverse relationship between the duration of breastfeeding and the frequency of antibiotic use in infants. Decreased colonization by MRSA may be the reason that exclusive breastfeeding is a protective factor against MRSA infection in newborn infants.
Several molecular mechanisms have been elucidated for methicillin resistance of S. aureus.22,23 We did not perform molecular analysis on any of the isolated MRSA strains. Apart from the commonly known synthesis of modified PBP2a, S. aureus resistance to methicillin may also be determined by other mechanisms.24,25 One example is the staphylococcal strains referred to as borderline oxacillin-resistant S. aureus (BORSA), which do not carry modified PBP2a encoded by the mecA or mecC gene.26 In our study, BORSA strains, with oxacillin MIC of ≥4 µg/mL, can fall into the MRSA group. There are other limitations of our study. Due to the nature of an observational retrospective cohort study, the risk factors selected for analysis were not comprehensive enough to include all possible factors. Furthermore, this study is a single-center study with a limited sample size, which may cause bias. It is hoped that a related multi-center study can be conducted in the future.
Conclusions
Our research shows that a prior use of antibiotics for more than 48 hours is an independent risk factor for methicillin resistance in neonates with S. aureus infection, while, on the other hand, exclusive breast milk feeding is associated with a lower risk for MRSA infection. The prior history of antibiotic use and exclusive breast milk feeding may be important factors to be considered for appropriate antibiotic selection prior to availability of the antimicrobial susceptibility results. To reduce the risk of MRSA infections in neonatal intensive care units, we need to restrict the abuse of antibiotics in neonates. Furthermore, we should promote breastfeeding for all infants to protect newborns from MRSA infections.
Abbreviations
MRSA, methicillin-resistant Staphylococcus aureus; MSSA, methicillin-sensitive Staphylococcus aureus; NICU, neonatal intensive care unit; CLSI, clinical and Laboratory Standards Institute; VIF, variance inflation factor; OR, odds ratio; CI, confidence interval; IDM, infant of diabetic mother; OSH, outside hospitals.
Data Sharing Statement
The datasets generated during and analysed during the current study are not publicly available due to patient privacy protection but are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was approved by the ethical committee of Children’s Hospital of Fudan University, Shanghai, China. This study was conducted in accordance with the Declaration of Helsinki. The data are anonymous, and the requirement for informed consent was therefore waived.
Consent for Publication
Written informed consent for publication was obtained from all authors.
Acknowledgments
We would like to thank Dr. Robert Green for advice and critical review of the manuscript.
Author Contributions
All authors made significant contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically important intellectual content; gave final approval for the version to be published; agreed to submit to the current journal; and agreed to be accountable for all aspects of the work.
Funding
We have no financial support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zelellw DA, Dessie G, Worku Mengesha E, Balew Shiferaw M, Mela Merhaba M, Emishaw S. A systematic review and meta-analysis of the leading pathogens causing neonatal sepsis in developing countries. Biomed Res Int. 2021;2021:6626983. doi:10.1155/2021/6626983
2. Al-Taiar A, Hammoud MS, Cuiqing L, et al. Neonatal infections in China, Malaysia, Hong Kong and Thailand. Arch Dis Child Fetal Neonatal Ed. 2013;98(3):F249–F255. doi:10.1136/archdischild-2012-301767
3. Li JY, Chen SQ, Yan YY, et al. Identification and antimicrobial resistance of pathogens in neonatal septicemia in China-A meta-analysis. Int J Infect Dis. 2018;71:89–93. doi:10.1016/j.ijid.2018.04.794
4. Tumuhamye J, Sommerfelt H, Bwanga F, et al. Neonatal sepsis at Mulago national referral hospital in Uganda: etiology, antimicrobial resistance, associated factors and case fatality risk. PLoS One. 2020;15(8):e0237085. doi:10.1371/journal.pone.0237085
5. Giuffrè M, Bonura C, Cipolla D, Mammina C. MRSA infection in the neonatal intensive care unit. Expert Rev Anti Infect Ther. 2013;11(5):499–509. doi:10.1586/eri.13.28
6. Turner NA, Sharma-Kuinkel BK, Maskarinec SA, et al. Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research. Nat Rev Microbiol. 2019;17(4):203–218. doi:10.1038/s41579-018-0147-4
7. Geraci DM, Giuffrè M, Bonura C, et al. Methicillin-resistant Staphylococcus aureus colonization: a three-year prospective study in a neonatal intensive care unit in Italy. PLoS One. 2014;9(2):e87760. doi:10.1371/journal.pone.0087760
8. Giuffrè M, Amodio E, Bonura C, et al. Methicillin-resistant Staphylococcus aureus nasal colonization in a level III neonatal intensive care unit: incidence and risk factors. Am J Infect Control. 2015;43(5):476–481. doi:10.1016/j.ajic.2014.12.027
9. Jenul C, Horswill AR. Regulation of Staphylococcus aureus virulence. Microbiol Spectr. 2019;7(2):10.
10. Shang W, Hu Q, Yuan W, et al. Comparative fitness and determinants for the characteristic drug resistance of ST239-MRSA-III-t030 and ST239-MRSA-III-t037 strains isolated in China. Microb Drug Resist. 2016;22(3):185–192. doi:10.1089/mdr.2015.0226
11. Hu F, Zhu D, Wang F, Wang M. Current status and trends of antibacterial resistance in China. Clin Infect Dis. 2018;67(suppl_2):S128–S134. doi:10.1093/cid/ciy657
12. Fritz SA, Hogan PG, Hayek G, et al. Staphylococcus aureus colonization in children with community-associated Staphylococcus aureus skin infections and their household contacts. Arch Pediatr Adolesc Med. 2012;166(6):551–557. doi:10.1001/archpediatrics.2011.900
13. Reich PJ, Boyle MG, Hogan PG, et al. Emergence of community-associated methicillin-resistant Staphylococcus aureus strains in the neonatal intensive care unit: an infection prevention and patient safety challenge. Clin Microbiol Infect. 2016;22(7):
14. Fasciana T, Gargano ML, Serra N, et al. Potential activity of albino Grifola frondosa mushroom extract against biofilm of methicillin-resistant. Staphylococcus aureus J Fungi. 2021;7(7):551.
15. Inoue M, Uchida K, Nagano Y, et al. Risk factors and intraoral breast milk application for methicillin-resistant Staphylococcus aureus colonization in surgical neonates. Pediatr Int. 2020;62(8):957–961. doi:10.1111/ped.14228
16. Huang YC, Chou YH, Su LH, Lien RI, Lin TY. Methicillin-resistant Staphylococcus aureus colonization and its association with infection among infants hospitalized in neonatal intensive care units. Pediatrics. 2006;118(2):469–474. doi:10.1542/peds.2006-0254
17. Zimmermann P, Curtis N. Breast milk microbiota: a review of the factors that influence composition. J Infect. 2020;81(1):17–47. doi:10.1016/j.jinf.2020.01.023
18. Reis NA, Saraiva MA, Duarte EA, de Carvalho EA, Vieira BB, Evangelista-Barreto NS. Probiotic properties of lactic acid bacteria isolated from human milk. J Appl Microbiol. 2016;121(3):811–820. doi:10.1111/jam.13173
19. Wiciński M, Sawicka E, Gębalski J, Kubiak K, Malinowski B. Human milk oligosaccharides: health benefits, potential applications in infant formulas, and pharmacology. Nutrients. 2020;12(1):266. doi:10.3390/nu12010266
20. Korpela K, Salonen A, Virta LJ, Kekkonen RA, de Vos WM. Association of early-life antibiotic use and protective effects of breastfeeding: role of the intestinal microbiota. JAMA Pediatr. 2016;170(8):750–757. doi:10.1001/jamapediatrics.2016.0585
21. Davisse-Paturet C, Adel-Patient K, Divaret-Chauveau A, et al. Breastfeeding status and duration and infections, hospitalizations for infections, and antibiotic use in the first two years of life in the ELFE cohort. Nutrients. 2019;11(7):1607. doi:10.3390/nu11071607
22. Peacock SJ, Paterson GK. Mechanisms of methicillin resistance in Staphylococcus aureus.. Annu Rev Biochem. 2015;84:577–601. doi:10.1146/annurev-biochem-060614-034516
23. Mammina C, Calà C, Bonura C, et al. Polyclonal non multiresistant methicillin resistant Staphylococcus aureus isolates from clinical cases of infection occurring in Palermo, Italy, during a one-year surveillance period. Ann Clin Microbiol Antimicrob. 2012;11:17. doi:10.1186/1476-0711-11-17
24. Montanari MP, Massidda O, Mingoia M, Varaldo PE. Borderline susceptibility to methicillin in Staphylococcus aureus: a new mechanism of resistance? Microb Drug Resist. 1996;2(2):257–260. doi:10.1089/mdr.1996.2.257
25. Djoudi F, Bonura C, Benallaoua S, et al. Panton-Valentine leukocidin positive sequence type 80 methicillin-resistant Staphylococcus aureus carrying a staphylococcal cassette chromosome mec type IVc is dominant in neonates and children in an Algiers hospital. New Microbiol. 2013;36(1):49–55.
26. Hryniewicz MM, Garbacz K. Borderline oxacillin-resistant Staphylococcus aureus (BORSA) - a more common problem than expected? J Med Microbiol. 2017;66(10):1367–1373. doi:10.1099/jmm.0.000585
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
