Back to Journals » International Journal of General Medicine » Volume 16
Risk Factors and Prognostic Implications of New-Onset Paroxysmal Atrial Fibrillation in Patients Hospitalized with Intracerebral Hemorrhage
Authors Huang B , Li J, Li P, Chen C, Cao S, Jiang Z, Zeng J
Received 21 March 2023
Accepted for publication 12 May 2023
Published 23 May 2023 Volume 2023:16 Pages 1973—1981
DOI https://doi.org/10.2147/IJGM.S411722
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Baozi Huang,1,2 Jianle Li,1 Pingping Li,1,2 Chunyong Chen,1,2 Suhan Cao,1 Zimu Jiang,1 Jinsheng Zeng1
1Department of Neurology and Stroke Center, Guangdong Provincial Key Laboratory of Diagnosis and Treatment of Major Neurological Diseases, The First Affiliated Hospital, Sun Yat-sen University, National Key Clinical Department and Key Discipline of Neurology, Guangzhou, People’s Republic of China; 2Department of Neurology of the First Affiliated Hospital of Guangxi Medical University, Nanning, People’s Republic of China
Correspondence: Jinsheng Zeng, Department of Neurology and Stroke Center, Guangdong Provincial Key Laboratory of Diagnosis and Treatment of Major Neurological Diseases, The First Affiliated Hospital, Sun Yat-sen University, National Key Clinical Department and Key Discipline of Neurology, No. 58 Zhongshan Road 2, Guangzhou, 510080, People’s Republic of China, Tel +86-20-87755766-8253, Fax +86-20-87335935, Email [email protected]
Objective: We aimed to assess the prevalence and risk factors of new-onset paroxysmal atrial fibrillation (PAF) in patients hospitalized with ICH and determine whether the new-onset PAF had influenced functional outcomes.
Methods: We analyzed a database of all consecutive patients with ICH from October 2013 to May 2022. Univariate and multivariable regression analyses were performed to identify risk factors for new-onset PAF in patients with ICH. Multivariate models were also constructed to assess whether the new-onset PAF was an independent predictor of poor functional outcome, as measured using the modified Rankin scale.
Results: This study included 650 patients with ICH, among whom 24 patients had new-onset PAF. In the multivariable model, older age (OR per 10-y increase, 2.26 [95% CI, 1.52– 3.35]; P< 0.001), hematoma volume (OR per 10-mL increase, 1.80 [95% CI, 1.26– 2.57]; P=0.001), and heart failure (OR, 21.77 [95% CI, 5.52– 85.91]; P< 0.001) were independent risk factors for new-onset PAF. In a sensitivity analysis restricted to 428 patients with N-terminal pro-B-type natriuretic peptide (NT-proBNP), older age, larger hematoma volume, heart failure, and increased NT-proBNP were associated with new-onset PAF. After adjusting for baseline variables, new-onset PAF was an independent predictor of poor functional outcome (OR, 10.35 [95% CI, 1.08– 98.80]; P=0.042).
Conclusion: Older age, larger hematoma volume, and heart failure were independent risk factors for new-onset PAF after ICH. Increased NT-proBNP is correlated with higher risks for new-onset PAF when their information is available at admission. Furthermore, new-onset PAF is a significant predictor of poor functional outcome.
Keywords: intracerebral hemorrhage, paroxysmal atrial fibrillation, prognostic implication, risk factors
Introduction
Atrial fibrillation (AF) is a significant risk factor for cardioembolic stroke.1 Among patients with embolic stroke of undetermined source (ESUS), paroxysmal AF (PAF) is considered to be the main underlying cause and is detected in 10–30% of these patients.2,3 Timely detection of PAF after acute ischemic stroke (AIS) has meaningful therapeutic implications; therefore, predictors of PAF in patients with AIS have been widely investigated.4–7 However, limited data are available regarding the prevalence and risk factors of new-onset PAF after intracerebral hemorrhage (ICH), rather than patients with an ICH secondary to AIS. The rates of new AF in patients with ICH reportedly range from 2.6% to 6%; however, these studies were limited by classifying AF patterns and no risk factor verification.8–10 Newly diagnosed AF during hospitalization is independently related to an unfavorable 3-month outcome among patients with a cardioembolic stroke.11 Nevertheless, whether this new-onset, transient, and accidentally discovered AF is associated with poor functional outcome in patients with ICH remains unknown. Thus, this study aimed to investigate the prevalence and risk factors of new-onset PAF in patients who were hospitalized for ICH and assess the association between new-onset PAF and functional outcomes at discharge.
Methods
Patient Selection
This study enrolled consecutive patients diagnosed with ICH at the First Affiliated Hospitals of Sun Yat-sen University between October 2013 and May 2022. All study procedures were approved by the independent ethics committee of the First Affiliated Hospitals of Sun Yat-sen University, and obtaining informed consent from patients was not required due to its retrospective nature. The inclusion criteria were (1) Age ≥18 years; (2) Evidence of cerebral hemorrhage on head computed tomography (CT); (3) Onset time of less than 7 days; (4) At least 24 hours of continuous stroke unit electrocardiography monitoring (CEM); and (5) Modified Rankin Scale (mRS) score ≤1 prior to ICH. Patients were excluded if they met one or more of the following criteria: (1) Surgery before admission; (2) Hospital stay less than 24 hours; (3) Post-cardiopulmonary resuscitation; (4) History of AF; (5) Traumatic ICH; (6) A recent cerebral ischemia (<3 months); and (7) Isolated intraventricular hemorrhage (IVH).
Data Collection
Baseline clinical information, including gender, age, systolic blood pressure (SBP), pneumonia, surgical interventions, intensive care unit (ICU) admission, duration of CEM, and length of hospital stay were extracted. Blood tests on admission were available for creatinine, N-terminal pro-B-type natriuretic peptide (NT-proBNP), and glucose levels. Hypertension was defined as a medical history of hypertension or systolic BP ≥140mm Hg or diastolic BP ≥90mm. Diabetes mellitus was defined by a fasting blood glucose ≥7.0mmol/L or postprandial blood glucose ≥11.1mmol/L or HbA1c ≥7% or a medical history of diabetes. Smoking status was based on self-report and defined as current smoker, never smoker, or past smoker. Coronary heart disease was defined as a medical history of myocardial infarction or coronary revascularization.12 Heart failure was defined by the presence of symptoms and signs of heart failure, and one of the following diagnostic criteria: a plasma NT-proBNP ≥125 ng/L or a left ventricular ejection fraction (LVEF) ≤40%.13
AF episodes were evaluated by CEM with an automated detection of AF. All episodes of AF were confirmed by a trained neurologist and classified as having paroxysmal or sustained AF according to the 2010 European Society of Cardiology guidelines for the management of AF.14 We defined new-onset PAF as AF that was detected during the hospitalization of patients who had no history of AF and that terminated spontaneously within 7 days of onset.
The baseline head CT was assessed by two independent neurologists. We determined the location of the insula based on the identification of the Alberta stroke program early CT score region.15 We considered that the insula was damaged when it was directly involved or deformation was caused by the mass effect of ICH.10 Hematoma location was determined and classified as follows: lobar (occipital, parietal, temporal, and frontal), deep (basal ganglia and thalamus), and infratentorial (cerebellar and brainstem). The ABC/2 method was used to measure the hematoma volume.16 In addition, the presence of IVH and/or subarachnoid hemorrhage (SAH) was documented.
Evaluation of Clinical Outcomes
The Glasgow Coma Scale (GCS) score was used to assess the clinical status at the time of patient admission. Functional outcomes at discharge were assessed using the mRS on a scale of 0–6. Outcomes were dichotomized into good functional outcome, indicated by an mRS of 0–3, and poor functional outcome, indicated by an mRS of 4–6.17,18
Statistical Analysis
Continuous variables with a normal distribution are expressed as mean ± standard deviation, while not normally distributed data are presented as medians with interquartile ranges, and differences between groups are assessed using the Student’s t-test or Wilcoxon rank-sum test, respectively. Categorical variables are presented as frequencies with percentages and compared using Pearson’s chi-square test or Fisher’s exact test. Potential risk factors for new-onset PAF were selected based on medical judgment and were assessed using univariate analysis, and a multivariable regression model based on a set of all potential predictors (P > 0.1) using forward selection was created. The multivariable regression model was used for a subset of patients with NT-proBNP data.
To analyze ICH outcomes at discharge, we performed multivariate logistic regression to investigate whether new-onset PAF was an independent predictor for poor functional outcome. The variables for the models initially included variables related to poor functional outcome in the univariate analysis, and we subsequently performed a forward stepwise selection procedure. All statistical analyses were performed using the R software (version 4.1.1), and significance was set at P values <0.05.
Results
Baseline Characteristics of Patients with and without New-Onset PAF
Among 1656 patients who were diagnosed with ICH, 650 patients met the inclusion criteria, and their data were included in the final analysis (Figure 1). Baseline characteristics of 650 patients with ICH stratified by new-onset PAF are summarized in Table 1. New-onset PAF was detected in 24 (3.7%) patients, and all of them admitted within 3 days of symptoms onset. Patients with new-onset PAF were older and more likely to have heart failure, pneumonia, and longer duration of ECM. Regarding the radiological information, the presence of IVH and larger hematoma volume were significantly more frequent in patients with new-onset PAF. Furthermore, patients with new-onset PAF had higher mRS at discharge and lower GCS scores on admission than patients without new-onset PAF. Information on baseline NT-proBNP levels was available for 428 patients. The median NT-proBNP levels were 647 (268–2328) pg/mL and 160 (69–514) pg/mL in patients with and without new-onset PAF, respectively (P<0.001; Table 1).
 |
Table 1 Baseline Characteristics of Patients with Intracerebral Hemorrhage with and without New-Onset PAF |
 |
Figure 1 Study flow chart. Abbreviations: ICH, intracerebral hemorrhage; AF, atrial fibrillation; IVH, intraventricular hemorrhage. |
Risk Factors for New-Onset PAF
The univariable risk factors for new-onset PAF in patients with ICH are shown in Table 2. Older age (odds ratio [OR] per 10-y increase, 2.50 [95% CI, 1.69–3.68]; P<0.001), larger hematoma volume (OR per 10-mL increase, 1.63 [95% CI, 1.19–2.24]; P=0.003), heart failure (OR, 29.48 [95% CI, 9.00–96.59]; P<0.001), and duration of ECM (OR, 1.03 [95% CI, 1.01–1.05]; P=0.011) were significantly associated with new-onset PAF.
 |
Table 2 Univariable Regression Model of Risk Factors for New-Onset PAF in Patients with Intracerebral Hemorrhage |
The results of the multivariable analyses are presented in Table 3. Significant risk factors included older age (OR per 10-y increase, 2.26 [95% CI, 1.52–3.35]; P<0.001), larger hematoma volume (OR per 10-mL increase, 1.80 [95% CI, 1.26–2.57]; P=0.001), and heart failure (OR, 21.77 [95% CI, 5.52–85.91]; P<0.001).
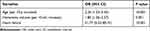 |
Table 3 Multivariate Logistic Regression Analyses of Risk Factors for New-Onset PAF Among Patients with Intracerebral Hemorrhage |
Sensitivity Analysis
We performed an analysis of multivariable risk factors for new-onset PAF among 428 patients with baseline NT-proBNP levels, and the results are shown in Table 4. Older age (OR per 10-y increase, 2.16 [95% CI, 1.44–3.24]; P<0.001), larger hematoma volume (OR per 10-mL increase, 1.69 [95% CI, 1.17–2.45]; P=0.005), heart failure (OR, 8.35 [95% CI, 1.91–36.55]; P=0.005), and higher NT-proBNP levels (OR per 1-U increase on log scale, 1.32 [95% CI, 1.00–1.73]; P=0.049) were independently associated with new-onset PAF. There was no statistically significant interaction between heart failure and NT-proBNP.
 |
Table 4 Sensitivity Analysis: Multivariable Analyses of Risk Factors for New-Onset PAF Restricted to Patients with Baseline NT-proBNP Levels (n = 428) |
New-Onset PAF and Functional Outcomes at Discharge
The characteristics of the included patients stratified by functional outcomes at discharge are shown in Table 5. Compared with patients with good functional outcome, new-onset PAF was significantly more frequent in patients with poor functional outcome (0.32% vs 6.82%, P<0.001).
 |
Table 5 Characteristics of Patients with Intracerebral Hemorrhage Stratified by Functional Outcomes at Discharge |
Univariable analysis was performed to define the predictors of poor functional outcome at discharge, and the results are shown in Table 6. In the multivariate analysis, new-onset PAF (OR, 10.35 [95% CI, 1.08–98.8]; P=0.042), larger hematoma volume (OR per 10–mL increase, 1.30 [95% CI,1.05–1.60]; P=0.016), heart failure (OR, 10.81 [95% CI, 1.09–107.38]; P=0.042), pneumonia (OR, 1.93 [95% CI, 1.11–3.34]; P=0.019), and lower GCS scores (OR, 0.51 [95% CI, 0.44–0.58]; P<0.001) were independent predictors of poor functional outcome in patients with ICH (Table 6).
 |
Table 6 Univariable and Multivariable Regression Model of Predictors of Poor Functional Outcome at Discharge in Patients with Intracerebral Hemorrhage |
Discussion
In this study of patients with ICH, 24 (3.7%) cases of new-onset PAF were detected during hospitalization. Older age, larger hematoma volume, and heart failure were associated with a higher risk for new-onset PAF in patients with ICH. When NT-proBNP was available, older age, larger hematoma volume, heart failure, and increased NT-proBNP levels were independent risk factors for new-onset PAF. Furthermore, new-onset PAF was independently associated with poor functional outcome at discharge.
Previous studies have mainly focused on the PAF detection in patients with AIS, especially in those diagnosed with ESUS.19,20 Nevertheless, few studies have specifically investigated the prevalence of PAF in patients with ICH. In our study, 3.7% of patients had new-onset PAF detection after ICH during hospitalization. The results presented are comparable to those of a study of unselected patients with AIS and revealed that new AF was detected in 68 of 1717 patients (4.0%) after monitoring using usual diagnostic procedures in the hospital.21 Furthermore, another study using at least 24 h of rhythm monitoring in patients with AIS aged ≥60 years reported slightly higher rates of new AF detection than our results.22 Although there are no data regarding the differences in the prevalence of new-onset PAF in patients with ICH versus to that in patients with AIS, our study suggests that new-onset PAF is not uncommon in patients with ICH, and this needs to be further investigated.
Our study demonstrated that older age, heart failure and increased NT-proBNP were independently associated with the risk of developing new-onset PAF in patients with ICH. This result is in line with results of previous studies conducted among patients with AIS and in high-risk populations.5,7,23–26 Interestingly, we found that larger hematoma volume was significantly associated with the incidence of new-onset PAF after ICH. However, the exact underlying mechanisms remain unclear. Inflammation and its associated immune responses play an important role in AF pathogenesis.27 When ICH occurs, a pronounced inflammatory reaction occurs immediately, which is characterized by the breakdown of the blood–brain barrier,28 activation of microglia, and production of inflammatory factors.29–31 Therefore, new-onset PAF may be a complication of systemic inflammation following ICH. Furthermore, autonomic dysregulation has been observed in patients with ICH, with decreased heart rate variability and baroreflex sensitivity.32,33 Evidence from clinical studies and animal models revealed that autonomic dysfunction contributes to atrial electrical and structural remodeling, thereby increasing AF inducibility.34–38 Altogether, these data indicate that systemic inflammation and autonomic dysfunction may be the important pathophysiology of new-onset PAF in patients with ICH.
Our study showed that the new-onset PAF is an independent predictor of poor functional outcome after ICH. However, it remains unknown whether new-onset PAF in these patients is a direct cause of poor functional outcome or just a marker of disease severity. It is well known that AF can trigger or worsen heart failure, then leading to reduced cardiac output.39 Although the duration of AF episodes was relatively short, the adverse hemodynamic consequences may persist after AF episodes terminated.40 Therefore, this effect could be harmful for patients who were diagnosed with new-onset PAF after ICH. In addition, although new-onset PAF remained significantly associated with poor functional outcome after adjusting for potential confounders, the magnitude of the correlation was obviously diminished, indicating that the poor functional outcome can be affected by other risk factors. Consistent with previous studies,41–43 we found that hematoma volume, pneumonia, heart failure, and lower GCS scores were strongly correlated with poor functional outcome after ICH. Therefore, they may explain most of the association between new-onset PAF and poor functional outcome. Nevertheless, screening for new-onset PAF among patients with high-risk ICH remains important, and further studies are needed to determine the risk of ischemic stroke and optimal management of these patients.
Our study had some limitations. First, the incidence of PAF after ICH may be underestimated, because of the lack of an AF detection workup and standardized use of long-term cardiac monitoring during hospitalization. Second, although the patients diagnosed with recent cerebral ischemia were not included, we could not exclude the possibility that some patients may have occult PAF before a stroke event. Finally, this was a retrospective, single-center study with a small sample size and low number of events. To further validate these findings, a multicenter prospective study with more patients and a longer follow-up period is required.
Conclusion
In this study, older age, larger hematoma volume, and heart failure were independent risk factors of new-onset PAF in patients with ICH. When data on NT-proBNP were available, increased NT-proBNP levels were also associated with a higher likelihood of detecting new-onset PAF. Furthermore, new-onset PAF was predictive of poor functional outcome after ICH. However, because of the retrospective nature and small sample size of this study, further investigations are needed.
Abbreviations
AF, atrial fibrillation; ICH, intracerebral hemorrhage; PAF, paroxysmal atrial fibrillation; NT-proBNP, N-terminal pro-B-type natriuretic peptide; AIS, acute ischemic stroke; CEM, continuous stroke unit electrocardiography monitoring; IVH, intraventricular hemorrhage; SAH, subarachnoid hemorrhage; SBP, systolic blood pressure; ICU, intensive care unit; GCS, Glasgow Coma Scale; OR, odds ratio; CI, confidence interval.
Ethics Statement
The study was performed according to the Declaration of Helsinki guidelines and was approved by the independent ethics committee of the First Affiliated Hospitals of Sun Yat-sen University. Written informed consent from patients was not required due to its retrospective nature, and all data used in this study was anonymized.
Funding
This study was supported by grants from the National Key R&D Program of China (2017YFC1307500), the Natural Science Foundation of China (Key Program: 82130035; General Program: 81771137, 81971103), the Scientific and Technical Project of Guangdong Province (2017A030303011), Sun Yat-sen University Clinical Research 5010 Program (2018001), the Guangdong Provincial Key Laboratory for Diagnosis and Treatment of Major Neurological Diseases (2017B030314103), Guangdong Provincial Clinical Research Center for Neurological Diseases (2020B1111170002), the Southern China International Cooperation Base for Early Intervention and Functional Rehabilitation of Neurological Diseases (2015B050501003), Guangdong Provincial Engineering Center for Major Neurological Disease Treatment, and Guangdong Provincial Translational Medicine Innovation Platform for Diagnosis and Treatment of Major Neurological Disease.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42:373–498. doi:10.1093/eurheartj/ehaa612
2. Thijs VN, Brachmann J, Morillo CA, et al. Predictors for atrial fibrillation detection after cryptogenic stroke: results from crystal af. Neurology. 2016;86(3):261–269. doi:10.1212/WNL.0000000000002282
3. Gladstone DJ, Dorian P, Spring M, et al. Atrial premature beats predict atrial fibrillation in cryptogenic stroke: results from the embrace trial. Stroke. 2015;46(4):936–941. doi:10.1161/STROKEAHA.115.008714
4. Israel C, Kitsiou A, Kalyani M, et al. Detection of atrial fibrillation in patients with embolic stroke of undetermined source by prolonged monitoring with implantable loop recorders. Thromb Haemost. 2017;117(10):1962–1969. doi:10.1160/TH17-02-0072
5. Bisson A, Bodin A, Clementy N, Babuty D, Lip GYH, Fauchier L. Prediction of incident atrial fibrillation according to gender in patients with ischemic stroke from a nationwide cohort. Am J Cardiol. 2018;121:437–444. doi:10.1016/j.amjcard.2017.11.016
6. Schnabel RB, Sullivan LM, Levy D, et al. Development of a risk score for atrial fibrillation (Framingham Heart Study): a community-based cohort study. Lancet. 2009;373:739–745. doi:10.1016/S0140-6736(09)60443-8
7. Friberg L, Rosenqvist M, Lindgren A, Terént A, Norrving B, Asplund K. High prevalence of atrial fibrillation among patients with ischemic stroke. Stroke. 2014;45:2599–2605. doi:10.1161/STROKEAHA.114.006070
8. Putaala J, Lehto M, Meretoja A, et al. In-hospital cardiac complications after intracerebral hemorrhage. Int J Stroke. 2014;9:741–746. doi:10.1111/ijs.12180
9. Horstmann S, Rizos T, Jenetzky E, Gumbinger C, Hacke W, Veltkamp R. Prevalence of atrial fibrillation in intracerebral hemorrhage. Eur J Neurol. 2014;21(4):570–576. doi:10.1111/ene.12215
10. Prats-Sanchez L, Guisado-Alonso D, Painous C, et al. Insular damage, new-onset atrial fibrillation and outcome after acute intracerebral hemorrhage. Eur J Neurol. 2018;25:491–496. doi:10.1111/ene.13522
11. Henninger N, Goddeau RP
12. Du X, Guo L, Xia S, et al. Atrial fibrillation prevalence, awareness and management in a nationwide survey of adults in China. Heart. 2021;107(7):535–541. doi:10.1136/heartjnl-2020-317915
13. Masini G, Graham FJ, Pellicori P, et al. Criteria for iron deficiency in patients with heart failure. J Am Coll Cardiol. 2022;79:341–351. doi:10.1016/j.jacc.2021.11.039
14. Camm AJ, Kirchhof P, Lip GY, et al. Guidelines for the management of atrial fibrillation: the task force for the management of atrial fibrillation of the European society of cardiology (esc). Eur Heart J. 2010;31(19):2369–2429. doi:10.1093/eurheartj/ehq278
15. Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. Aspects study group. Alberta stroke programme early ct score. Lancet. 2000;355(9216):1670–1674. doi:10.1016/S0140-6736(00)02237-6
16. Kothari RU, Brott T, Broderick JP, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996;27(8):1304–1305. doi:10.1161/01.STR.27.8.1304
17. Hanley DF, Lane K, McBee N, et al. Thrombolytic removal of intraventricular haemorrhage in treatment of severe stroke: results of the randomised, multicentre, multiregion, placebo-controlled clear iii trial. Lancet. 2017;389(10069):603–611. doi:10.1016/S0140-6736(16)32410-2
18. Qureshi AI, Palesch YY, Barsan WG, et al. Intensive blood-pressure lowering in patients with acute cerebral hemorrhage. N Engl J Med. 2016;375(11):1033–1043. doi:10.1056/NEJMoa1603460
19. Sanna T, Diener HC, Passman RS, et al. Cryptogenic stroke and underlying atrial fibrillation. N Engl J Med. 2014;370(26):2478–2486. doi:10.1056/NEJMoa1313600
20. Gladstone DJ, Spring M, Dorian P, et al. Atrial fibrillation in patients with cryptogenic stroke. N Engl J Med. 2014;370(26):2467–2477. doi:10.1056/NEJMoa1311376
21. Haeusler KG, Kirchhof P, Kunze C, et al. Systematic monitoring for detection of atrial fibrillation in patients with acute ischaemic stroke (mondafis): a randomised, open-label, multicentre study. Lancet Neurol. 2021;20(6):426–436. doi:10.1016/S1474-4422(21)00067-3
22. Wachter R, Gröschel K, Gelbrich G, et al. Holter-electrocardiogram-monitoring in patients with acute ischaemic stroke (find-af randomised): an open-label randomised controlled trial. Lancet Neurol. 2017;16(4):282–290. doi:10.1016/S1474-4422(17)30002-9
23. Bahit MC, Sacco RL, Easton JD, et al. Predictors of atrial fibrillation development in patients with embolic stroke of undetermined source: an analysis of the re-spect esus trial. Circulation. 2021;144(22):1738–1746. doi:10.1161/CIRCULATIONAHA.121.055176
24. Kim BS, Chun KJ, Hwang JK, et al. Predictors and long-term clinical outcomes of newly developed atrial fibrillation in patients with cardiac implantable electronic devices. Medicine. 2016;95(28):e4181. doi:10.1097/MD.0000000000004181
25. Fonseca AC, Brito D, Pinho e Melo T, et al. N-terminal pro-brain natriuretic peptide shows diagnostic accuracy for detecting atrial fibrillation in cryptogenic stroke patients. Int J Stroke. 2014;9:419–425. doi:10.1111/ijs.12126
26. Wachter R, Lahno R, Haase B, et al. Natriuretic peptides for the detection of paroxysmal atrial fibrillation in patients with cerebral ischemia--The find-af study. PLoS One. 2012;7:e34351. doi:10.1371/journal.pone.0034351
27. Hu YF, Chen YJ, Lin YJ, Chen SA. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol. 2015;12:230–243. doi:10.1038/nrcardio.2015.2
28. Keep RF, Xiang J, Ennis SR, et al. Blood-brain barrier function in intracerebral hemorrhage. Acta Neurochir Suppl. 2008;105:73–77.
29. Wang J. Preclinical and clinical research on inflammation after intracerebral hemorrhage. Prog Neurobiol. 2010;92(4):463–477. doi:10.1016/j.pneurobio.2010.08.001
30. Wang J, Doré S. Inflammation after intracerebral hemorrhage. J Cereb Blood Flow Metab. 2007;27(5):894–908. doi:10.1038/sj.jcbfm.9600403
31. Keep RF, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. 2012;11(8):720–731. doi:10.1016/S1474-4422(12)70104-7
32. Sykora M, Diedler J, Rupp A, Turcani P, Rocco A, Steiner T. Impaired baroreflex sensitivity predicts outcome of acute intracerebral hemorrhage. Crit Care Med. 2008;36(11):3074–3079. doi:10.1097/CCM.0b013e31818b306d
33. Sykora M, Steiner T, Poli S, Rocco A, Turcani P, Diedler J. Autonomic effects of intraventricular extension in intracerebral hemorrhage. Neurocrit Care. 2012;16(1):102–108. doi:10.1007/s12028-011-9637-1
34. Coumel P, Attuel P, Lavallée J, Flammang D, Leclercq JF, Slama R. [The atrial arrhythmia syndrome of vagal origin]. Arch Mal Coeur Vaiss. 1978;71(6):645–656. French.
35. Amar D, Zhang H, Miodownik S, Kadish AH. Competing autonomic mechanisms precede the onset of postoperative atrial fibrillation. J Am Coll Cardiol. 2003;42:1262–1268. doi:10.1016/S0735-1097(03)00955-0
36. Bettoni M, Zimmermann M. Autonomic tone variations before the onset of paroxysmal atrial fibrillation. Circulation. 2002;105(23):2753–2759. doi:10.1161/01.CIR.0000018443.44005.D8
37. Tomita T, Takei M, Saikawa Y, et al. Role of autonomic tone in the initiation and termination of paroxysmal atrial fibrillation in patients without structural heart disease. J Cardiovasc Electrophysiol. 2003;14(6):559–564. doi:10.1046/j.1540-8167.2003.02462.x
38. Tan AY, Zhou S, Ogawa M, et al. Neural mechanisms of paroxysmal atrial fibrillation and paroxysmal atrial tachycardia in ambulatory canines. Circulation. 2008;118(9):916–925. doi:10.1161/CIRCULATIONAHA.108.776203
39. Clark DM, Plumb VJ, Epstein AE, Kay GN. Hemodynamic effects of an irregular sequence of ventricular cycle lengths during atrial fibrillation. J Am Coll Cardiol. 1997;30(4):1039–1045. doi:10.1016/S0735-1097(97)00254-4
40. O’Neill PG, Puleo PR, Bolli R, Rokey R. Return of atrial mechanical function following electrical conversion of atrial dysrhythmias. Am Heart J. 1990;120(2):353–359. doi:10.1016/0002-8703(90)90079-D
41. Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 1993;24:987–993. doi:10.1161/01.STR.24.7.987
42. Fogelholm R, Murros K, Rissanen A, Avikainen S. Long term survival after primary intracerebral haemorrhage: a retrospective population based study. J Neurol Neurosurg Psychiatry. 2005;76:1534–1538. doi:10.1136/jnnp.2004.055145
43. Lindner A, Kofler M, Rass V, et al. Early predictors for infectious complications in patients with spontaneous intracerebral hemorrhage and their impact on outcome. Front Neurol. 2019;10:817. doi:10.3389/fneur.2019.00817
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
