Back to Journals » Infection and Drug Resistance » Volume 15
Risk Factors and Clinical Impact of Carbapenem-Resistant Enterobacterales Coinfections Among Hospitalized Patients with Clostridioides difficile Infection
Authors Lee CC , Chiu CW, Lee JC, Tsai PJ , Ko WC , Hung YP
Received 16 August 2022
Accepted for publication 26 October 2022
Published 31 October 2022 Volume 2022:15 Pages 6287—6295
DOI https://doi.org/10.2147/IDR.S386309
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Ching-Chi Lee,1– 3,* Chun-Wei Chiu,4,* Jen-Chieh Lee,1 Pei-Jane Tsai,5– 7 Wen-Chien Ko,1,8 Yuan-Pin Hung1,4,8,9
1Department of Internal Medicine, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan; 2Graduate Institute of Medical Sciences, College of Health Sciences, Chang Jung Christian University, Tainan, 711, Taiwan; 3Clinical Medicine Research Center, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan; 4Department of Internal Medicine, Tainan Hospital, Ministry of Health and Welfare, Tainan, 700, Taiwan; 5Department of Medical Laboratory Science and Biotechnology, National Cheng Kung University, College of Medicine, Tainan, 704, Taiwan; 6Department of Pathology, National Cheng Kung University Hospital, Tainan, Taiwan; 7Centers of Infectious Disease and Signaling Research, National Cheng Kung University, Tainan, Taiwan; 8Department of Medicine, College of Medicine, National Cheng Kung University, Tainan, 704, Taiwan; 9Department of Microbiology & Immunology, College of Medicine, National Cheng Kung University, Tainan, Taiwan
*These authors contributed equally to this work
Correspondence: Yuan-Pin Hung, Department of Internal Medicine, Tainan Hospital, Ministry of Health and Welfare, Tainan, Taiwan, Email [email protected] Wen-Chien Ko, Department of Internal Medicine, College of Medicine, National Cheng Kung University Hospital, Tainan, Taiwan, Email [email protected]
Introduction: The risk factors and clinical impact of carbapenem-resistant Enterobacterales (CRE) coinfection among hospitalized patients with Clostridioides difficile infection (CDI) were analyzed in this study.
Materials and Methods: A clinical study was performed at the medical wards of Tainan Hospital, Ministry of Health and Welfare in southern Taiwan. Patients with CDI between January 2013 and April 2020 were included.
Results: Among 238 patients included for analysis, 22 (9.2%) patients developed CRE coinfections within 14 days before or after the onset of CDI. CDI patients with CRE coinfection had longer hospitalization stays (103.0 ± 97.0 days vs 42.5 ± 109.6 days, P = 0.01) than those without CRE coinfection. In the multivariate analysis, age (odds ratio [OR] 1.05, 95% confidence interval [CI] 1.01– 1.10, P = 0.02) was independently associated with CRE coinfection. In contrast, underlying old stroke (OR 0.15, 95% CI 0.03– 0.70, P = 0.02) was negatively linked to CRE coinfection.
Conclusion: Among patients with CDI, CRE coinfections were associated with prolonged hospitalization for CDI. Age was an independent risk factor for CRE coinfection among patients with CDI.
Keywords: carbapenem-resistant Enterobacterales, Clostridioides difficile infection, age, hypertension, recurrence, prolonged hospitalization
Introduction
Clostridioides difficile infections (CDIs) often cause intestinal infections with variable clinical presentations, ranging from mild diarrhea, pseudomembranous colitis, and toxic megacolon to death.1–10 An important factor associated with the disease severity of CDI is host immunity.5,9,11 One of the determinant factors of host immunity is the composition of the gut microbiota, which is critical in the development of CDI.12 Many host or environmental factors, including diet, sleep, and disease, can alter the diversity and abundancy of microbiota.13,14 Moreover, oral vancomycin had been suggested as drug of therapy for CDI and their use further disturbs the fragile microbiota, for example reduced proportion of Bacteroidia and Clostridia and increased proportion of Proteobacteria.15 The disturbance of microbiota can result in the rise of multidrug-resistant organisms (MDROs).16
The prevalence rate of carbapenem-resistant Enterobacterales (CRE), one of the most notorious MDRO, has increased in recent years.17 The colonization of these antimicrobial-resistant Enterobacterales in the gut is linked to lower phylogenetic diversity, dysbiotic microbiota, and depletion of anaerobic commensals in the microbiota of gut,18,19 as well as the increased risk of subsequent systemic infection and bacteremia due to CRE.18 Among CRE, carbapenem-resistant Klebsiella pneumoniae (CRKP) with evolution and complex genomic profiling has been an emerging public health problem.20,21 Carbapenem resistance rates among K. pneumoniae isolates from intensive care units (ICUs) were higher than those among Escherichia coli isolates in a meta-analysis restricted to the hospitals in Taiwan.22 Most importantly, clinical impact of the infections due to Enterobacterales with reduced carbapenem susceptibility is grave as evidenced by the finding of a multicenter ICU study that the 30-day mortality rate of 46 patients with carbapenem-nonsusceptible K. pneumoniae and/or E. coli infection was as high as 50%.23
As the prescription of antimicrobial therapy increases, the risk of intestinal colonization of more than one MDROs accordingly increases. In the real world, an active surveillance has been performed for rectal colonization of C. difficile and CRE among 301 residents in a long-term care facility. C. difficile colonization occurred in 58 (19.3%) patients, CRE in 57 (18.9%) patients, and both in 17 (5.7%).24 However, the incidence and impact of CRE coinfections among hospitalized patients with CDI remain undetermined. The implementation of mixed educational and semi-restrictive antimicrobial stewardship projects has decreased the incidence of CRE bloodstream infections but did not influence the occurrence of CDI.25 Moreover, CRE infections have resulted in substantial morbidity and mortality among hospitalized patients worldwide.26–28 In the era of the increasing incidence of CRE infections, the clinical impact of the coexistence of CRE infections among hospitalized patients with CDI was not clear. The objective of this study is to investigate the risk factors and clinical impact of CRE infections among hospitalized patients with CDI.
Materials and Methods
A retrospective study based on chart reviews was performed in the medical wards of the Tainan Hospital, Ministry of Health and Welfare, a regional hospital in southern Taiwan, between January 2013 and April 2020. The Institutional Review Board of National Cheng Kung University Hospital, Taiwan, approved this study (approval number: B-ER-103-098). Hospitalized adults (aged ≥20 years) with hospital-onset CDI (ie, symptom onset at least 48 hours after admission) were included. Antimicrobial susceptibility of identified Enterobacterales isolates was determined using disk diffusion in accordance with the procedures of the Clinical and Laboratory Standards Institute (CLSI) and interpreted according to the zone criteria of the CLSI issued in 2018 (M100-S21).29 Carbapenem resistance was defined as resistance to at least one of the three carbapenems (ie, ertapenem, imipenem, or meropenem) by the disk diffusion method.29 The events of acute CRE infections within 14 days before or after the onset of CDI were retrieved from medical records. CRE infections were distinguished from CRE colonization, according to the following criteria: those exhibited clinical signs and symptoms of inflammatory responses related to a documented or suspected site of infection, and were treated for CRE infection by at least two consecutive doses of antimicrobial agents.30 Otherwise, those with CRE colonization were excluded. No routine screening of intestinal CRE colonization for specific population was conducted in the hospital.
CDI was diagnosed as the presence of unexplained diarrhea and a positive result of glutamate dehydrogenase (GDH) and toxin A/B using an enzyme immunoassay (EIA) (Abbott, Santa Clara, USA) in fecal samples or the detection of tcdB-carrying C. difficile isolates in stool culture.31 Diarrhea was defined as at least three unformed bowel movements per day for at least two days. C. difficile cultures were performed on the cycloserine-cefoxitin-fructose agar (CCFA) plates, which were incubated anaerobically for 24–48 hours. A multiplex polymerase chain reaction (PCR) was used to detect tcdA, tcdB, cdtA, cdtB, and tcdC deletion in C. difficile isolates, as described previously.32
Clinical data, including sex, age, nasogastric tube use, underlying diseases, and laboratory data, were collected from electronic medical records using a predetermined record form. Medications, including antibiotics, proton pump inhibitors, histamine 2 (H2)-receptor antagonists, or steroids, prescribed within one month before the onset of CDI was recorded. The place of CDI onset, such as wards or intensive care units (ICUs), was recorded. Chronic kidney disease (CKD) was defined as an estimated glomerular filtration rate (eGFR) of <60 mL/min/1.73 m2 for at least three months.33 Colonization or infection with vancomycin-resistant enterococci (VRE), carbapenem-resistant Pseudomonas aeruginosa (CRPA), or carbapenem-resistant Acinetobacter baumannii (CRAB) during hospitalization was recorded based on medical charts.
Leukocyte count ≥15,000 cells/mL and serum creatinine of >1.5 mg/dL are two important predictors of severe CDI, according to the clinical guidelines issued by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA) updated in 2021.34 The duration of hospitalization preceding CDI was the period from admission to CDI onset, and only the first CDI episode was included. The appearance of relapsing diarrhea in combination with the detection of C. difficile toxin or tcdB-carrying C. difficile in unformed stools at least three weeks following initial treatment success was defined as having recurrent CDI.35
Statistical analysis was performed using statistical software (IBM SPSS, version 22.0). Continuous data are expressed as the means ± standard deviations. The χ2 or Fisher’s test was used for categorical variables, and Student’s t test was used for continuous variables. A two-tailed P value of <0.05 was considered statistically significant. The Bonferroni correction was applied for multiple comparisons. Variables with a P value <0.15 in univariate analysis were selected for multivariate analysis, which was performed using the Hosmer–Lemeshow test for goodness of fit in the logistic regression model. Since gut colonization with CRE was identified among patients with recurrent CDI, the impact of CRE coinfection on CDI recurrence was analyzed in multivariate analysis.25,36
Results
Of the 243 patients with CDI, 5 patients who did not require hospitalization were excluded (Figure 1). Among the 238 patients included, 114 (47.9%) patients were male, with a mean age (± standard deviation) of 75.7 (± 12.7) years. Twenty-two (9.2%) patients developed CRE coinfections within 14 days before or after the onset of CDI. For the timing of diagnosis of CRE coinfection, 10 patients were diagnosed at 4.5 ± 3.6 (mean ± standard deviation) days (range: 1–10 days) before onset of CDI, 2 at the day of onset of CDI, and 10 at 6.0 ± 3.1 days (1–11 days) after onset of CDI, with an in-hospital mortality rate of 31.8% (7 patients). Among 22 CRE isolates, 3 were E. coli and 19 were K. pneumoniae. Two E. coli and four 9 K. pneumoniae isolates were resistant to ertapenem but susceptible to meropenem, and the rest were resistant to ertapenem, meropenem, and imipenem. Five K. pneumoniae isolates were regarded as the etiological agents of pneumonia, and other CRE isolates were regarded as the causes of urinary tract infection. As for 216 patients with CDI but without CRE coinfection, 52 (24.1%) patients died in the hospital.
Twenty-two patients with CDI and CRE coinfection were more likely to have ICU-onset CDI (31.8% vs 13.0%, P = 0.03) and underlying diabetes mellitus (68.2% vs 44.9%, P = 0.04), but were less likely to have an old stroke (9.1% vs 39.8%, P = 0.004) than 216 CDI patients without CRE coinfection (Table 1). There were no differences in terms of sex, age, other underlying diseases, or prior drug exposure within one month before CDI onset in the two groups.
According to the definition by the IDSA/SHEA, the proportions of severe CDI (36.4% vs 35.2%, P = 1.00), blood leukocyte count ≥15,000 cells/mL (36.4% vs 25.0%, P = 0.31), or serum creatinine >1.5 mg/L (4.5% vs 13.4%, P = 0.33) were not significantly different in those with and without CDI-CRE coinfections (Table 2). Moreover, the proportion of tcdC deletion in C. difficile isolates and drug therapy for CDIs were similar in the two groups. However, CDI patients with CRE coinfection had a longer hospitalization duration (103.0 ± 97.0 days vs 42.5 ± 109.6 days, P = 0.01) and a higher recurrence rate of CDI (9.1% vs 6.0%, P = 0.64), although without statistical significance, than those without CRE coinfection. CDI patients with CRE coinfection were more likely to have CRAB colonization or infection (22.7% vs 8.3%, P = 0.046). In the multivariate analysis, age (odds ratio [OR] 1.05, 95% confidence interval (CI 1.01–1.10, P = 0.02) was independently associated with CRE coinfection. In contrast, underlying old stroke was negatively linked to the coexistence of CRE infection (OR 0.15, 95% CI 0.03–0.70, P= 0.02) (Table 3).
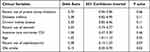 |
Table 3 Multivariate Analyses of Variables Associated with Carbapenem-Resistant Enterobacterales Coinfections Among Hospitalized Patients with Clostridioides difficile Infection (CDI) |
The impact of CRE coinfections on the recurrence of CDI was analyzed in multivariate analysis. Those with CDI recurrence more often had underlying hypertension than those without CDI recurrence (93.3% vs 61.4%, P = 0.01) (Table 4). There were no differences in terms of sex, age, or other underlying diseases between the two groups. In the multivariate analysis, CRE coinfection and chronic kidney disease were not associated with CDI recurrence, but hypertension was an independent risk factor for CDI recurrence (OR 8.46, 95% CI 1.09–65.92, P = 0.04).
 |
Table 4 Underlying Diseases and Prior Antibiotic or Medication Exposure in Patients with Clostridioides difficile Infection (CDI), Stratified by the Presence or Absence of Recurrence |
Discussion
CRE coinfection was found among 9.2% of patients with CDI in our study which was associated with prolonged hospitalization and probably a higher risk of CDI recurrence. The clinical impact of CRE infections was diverse among patients from different regions. The 30-day all-cause mortality rate was higher in South America (28%) than in China (12–19.7%), the United States (23%), or Taiwan (23.2%).26–28 Despite there are geographic variations in the prognostic impact of CRE infections among general population, CRE infections lead to more significant impact among ICU patients. Among patients in the respiratory ICU, CRKP infections resulted in the in-hospital mortality rate up to 42.1%.37 Accordingly, coinfections of CRE and CDI may be linked to a grave outcome, especially among those admitted to the ICU.
Age and CRAB colonization or infection are associated with CRE coinfections among our patients with CDI. Several characteristics of the elderly have been proposed as risk factors for CRE infections, including the presence of indwelling urinary catheters,37,38 central venous catheter use,38 nasogastric tubes,28,39 and multiple comorbidities.37,40 Moreover, these characteristics are risk factors for CRAB colonization or infection.41 There is no doubt that elderly patients or those with CRAB colonization or infection are prone to suffer from CRE coinfections among patients with CDI.
CRE coinfections might be associated with recurrence of CDI in the univariate analysis, but such an association became statistically insignificant in the multivariate analysis. Recognized risk factors for recurrent CDI included age, healthcare-associated CDI, prior hospitalization, antibiotic use, and proton pump inhibitor use, which were also risk factors for CRE infections.42,43 Therefore, recurrence of CDI should be closely monitored among patients with comorbidities and CRE coinfections.
The presence of prior stroke was related to a lower risk of CRE coinfection among our cases of CDI, but its rationale remains obscure. In the study hospital, most patients with stroke were hospitalized in the neurology ward, which is apart from other general wards. The different location might be one of the reasons that those with stroke had a lower risk of CRE coinfection. However, the causal effect of medications commonly prescribed for those with prior stroke and CRE infection warrants further evaluations. In contrast, hypertension, a common comorbidity in elderly individuals with CDI,44 was independently associated with recurrence of CDI. Moreover, the presence of hypertension has been independently associated with the development of CDI.45 Not surprisingly, CDI is related to dysbiosis, an imbalance in the composition and function of gut microbiota.16 Furthermore, dysbiosis was associated with hypertension in both animal models and humans.46 However, the complex interactions among hypertension, CDI recurrence, and gut dysbiosis merit further epidemiological or clinical investigations.
Routine screening for CRE colonization at admission was not performed in our hospital, and thus the patients with CRE colonization before admission or acquired in the community, if any, could not be identified. However, CRE colonization has been recognized as a risk factor of CRE infection,47 and those with non-intestinal CRE colonization would have similar clinical outcomes as those with CRE infection.48 Prospective investigations of the direct or indirect outcome impact of CRE colonization on patients with CDI, who often have imbalanced intestinal microbiota due to multifactorial predisposing factors, are warranted.
In our study, CRE coinfections were found among 9.2% of patients with CDI and were associated with prolonged hospitalization and probably a higher risk of CDI recurrence. In the United States, the case number of CDI and CRE infection in 2016 was estimated to be 468,567 and 9620, respectively.49 These infections caused 17,630 deaths and an annual loss of 8624 quality-adjusted life years in the survivors.49 Because of significant mortality and morbidity related to these infections, the estimated societal willingness to pay to avoid these diseases is high at $176.7 billion per year, of which 93.9% is for CDI.49 Therefore, it is urgent and essential to set up infection control policies, including antibiotic stewardship program, toward preventing CDI and CRE infections.50 According to the clinical practice guidelines proposed by the Infectious Diseases Society of America (IDSA)/Society for Healthcare Epidemiology of America (SHEA), discontinuing unnecessary antibiotics is one of the important measurements for CDI treatment and prevention.34 The incidence of nosocomial infections due to ertapenem-resistant Enterobacteriaceae before and after the prescription intervention by an antimicrobial restriction system was 48.0 and 9.5 infections per 10,000 patient-days.50 Therefore, it is critical for physicians, pharmacists, and healthcare professionals to recognize risk factors and clinical impact of CRE coinfections among hospitalized patients with CDI and promptly formulate plausible strategies of antimicrobial stewardship programs.
There were some limitations in this study. First, the molecular mechanisms of carbapenem resistance were not analyzed, and antimicrobial susceptibility or the therapeutic efficacy of antimicrobial therapy and the intrinsic virulence of different bacterial species were not assessed in this study. The confounding variables of clinical outcome cannot be fully considered. Second, in this study, CRE coinfections included CRE infections occurring before, after, or at the time of the onset of CDI. The prognostic impact of CRE infections discovered at different timings based on the onset of CDI is likely to vary. It is worth separately examining the influence of CRE infections that develop before, after or at the same time of onset of CDI if there are more cases of CDI included. Third, the coexistence of VRE, CRAB, or CRPA was noted from medical charts, and infection or colonization could not be distinguished perfectly due to limited clinical data. Their presence in CDI patients with or without CRE coinfection highlighted the clinical complexity among these hospitalized patients. Finally, the study conclusions were based on a small number of patients with both CDI and CRE (ie, 22 patients in total), and it is too early to apply the study findings to diverse patient cohorts in different hospitals.
In conclusion, CRE coinfections, of which age was an independent risk factor, were associated with prolonged hospitalization among patients with CDI.
Data Sharing Statement
The datasets used and/or analyzed during the current the study are available from the corresponding author on reasonable request.
Ethics Approval
The Institutional Review Board of National Cheng Kung University Hospital, Taiwan, approved this study (approval number: B-ER-103-098). The ethics committee waived the need for written informed consent provided by participants due to the retrospective nature of the study. Based on the Declaration of Helsinki, no additional informed consent was required, because all patient data were analyzed in anonymity.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The present study was supported by research grants from the Ministry of Science and Technology, Taiwan (109-2314-B-006-089-MY3, 110-2320-B-006-024 and 110-2314-B-675-001), Ministry of Health and Welfare, Taiwan (MOHW 110-TDU-B-211-124003); and National Cheng Kung University Hospital, Tainan, Taiwan (NCKUH-11004029).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Zhang RF, Man YX, Bai YY., et al. Molecular characterization of Clostridioides difficile ribotype 027 in a major Chinese hospital. J Microbiol Immunol Infect. 2021;54(6):1179–1183. doi:10.1016/j.jmii.2021.01.003
2. Lee JC, Hung YP, Tsai BY, et al. Severe Clostridium difficile infections in intensive care units: diverse clinical presentations. J Microbiol Immunol Infect. 2021;54(6):1111–1117. doi:10.1016/j.jmii.2020.07.012
3. Chang TH, Hsu WY, Yang TI, et al. Increased age and proton pump inhibitors are associated with severe Clostridium difficile infections in children. J Microbiol Immunol Infect. 2020;53(4):578–584. doi:10.1016/j.jmii.2018.09.002
4. Hung YP, Lee JC, Tsai BY, et al. Risk factors of Clostridium difficile-associated diarrhea in hospitalized adults: vary by hospitalized duration. J Microbiol Immunol Infect. 2021;54(2):276–283. doi:10.1016/j.jmii.2019.07.004
5. Hung YP, Tsai CS, Tsai BY, et al. Clostridioides difficile infection in patients with hematological malignancy: a multicenter study in Taiwan. J Microbiol Immunol Infect. 2021;54(6):1101–1110. doi:10.1016/j.jmii.2021.02.002
6. Lin TC, Hung YP, Ko WC, et al. Fecal microbiota transplantation for Clostridium difficile infection in Taiwan: establishment and implementation. J Microbiol Immunol Infect. 2019;52(6):841–850. doi:10.1016/j.jmii.2019.08.009
7. Wu KS, Syue LS, Cheng A, et al. Recommendations and guidelines for the treatment of Clostridioides difficile infection in Taiwan. J Microbiol Immunol Infect. 2020;53(2):191–208. doi:10.1016/j.jmii.2020.02.002
8. Chang FC, Liu CP, Sun FJ, et al. Optimizing laboratory workflow for the diagnosis of Clostridiodes difficile infection in a medical center in Northern Taiwan. J Microbiol Immunol Infect. 2021;54(2):284–289. doi:10.1016/j.jmii.2019.08.004
9. Lai YH, Tsai BY, Hsu CY, et al. The role of Toll-Like receptor-2 in Clostridioides difficile infection: evidence from a mouse model and clinical patients. Front Immunol. 2021;12:691039. doi:10.3389/fimmu.2021.691039
10. Chiu CW, Tsai PJ, Lee CC, et al. Inhibition of spores to prevent the recurrence of Clostridioides difficile infection - A possibility or an improbability? J Microbiol Immunol Infect. 2021;54(6):1011–1017. doi:10.1016/j.jmii.2021.06.002
11. Lee CC, Lee JC, Chiu CW, et al. Clinical significance of toxigenic Clostridioides difficile growth in stool cultures during the era of nonculture methods for the diagnosis of C. difficile infection. Microbiol Spectr. 2021;9(2):e0079921. doi:10.1128/Spectrum.00799-21
12. Di Tommaso N, Gasbarrini A, Ponziani FR. Intestinal barrier in human health and disease. Int J Environ Res Public Health. 2021;18(23):12836. doi:10.3390/ijerph182312836
13. Giuffre M, Campigotto M, Campisciano G, et al. A story of liver and gut microbes: how does the intestinal flora affect liver disease? A review of the literature. Am J Physiol Gastrointest Liver Physiol. 2020;318(5):G889–G906. doi:10.1152/ajpgi.00161.2019
14. Giuffre M, Moretti R, Campisciano G, et al. You talking to me? Says the enteric nervous system (ENS) to the microbe. How intestinal microbes interact with the ENS. J Clin Med. 2020;9(11):3705. doi:10.3390/jcm9113705
15. Yamaguchi T, Konishi H, Aoki K, et al. The gut microbiome diversity of Clostridioides difficile-inoculated mice treated with vancomycin and fidaxomicin. J Infect Chemother. 2020;26(5):483–491. doi:10.1016/j.jiac.2019.12.020
16. Wuethrich I, Khodamoradi Y, Vehreschild M. The role of the human gut microbiota in colonization and infection with multidrug-resistant bacteria. Gut Microbes. 2021;13(1):1–13. doi:10.1080/19490976.2021.1911279
17. Lin TC, Hung YP, Lin WT, et al. Risk factors and clinical impact of bacteremia due to carbapenem-nonsusceptible Enterobacteriaceae: a multicenter study in southern Taiwan. J Microbiol Immunol Infect. 2021;54(6):1122–1129. doi:10.1016/j.jmii.2021.05.005
18. Korach-Rechtman H, Hreish M, Fried C, et al. Intestinal dysbiosis in carriers of carbapenem-resistant Enterobacteriaceae. mSphere. 2020;5(2):e00173–20. doi:10.1128/mSphere.00173-20
19. Piewngam P, Quinones M, Thirakittiwatthana W, et al. Composition of the intestinal microbiota in extended-spectrum beta-lactamase-producing Enterobacteriaceae carriers and non-carriers in Thailand. Int J Antimicrob Agents. 2019;53(4):435–441. doi:10.1016/j.ijantimicag.2018.12.006
20. Saavedra SY, Bernal JF, Montilla-Escudero E, et al. Complexity of genomic epidemiology of carbapenem-resistant Klebsiella pneumoniae isolates in Colombia urges the reinforcement of whole genome sequencing-based surveillance programs. Clin Infect Dis. 2021;73(Suppl4):S290–S299. doi:10.1093/cid/ciab777
21. Nagaraj G, Shamanna V, Govindan V, et al. High-resolution genomic profiling of carbapenem-resistant Klebsiella pneumoniae isolates: a multicentric retrospective Indian study. Clin Infect Dis. 2021;73(Suppl4):S300–S307. doi:10.1093/cid/ciab767
22. Jean SS, Lee NY, Tang HJ, et al. Carbapenem-resistant Enterobacteriaceae infections: Taiwan aspects. Front Microbiol. 2018;9:2888. doi:10.3389/fmicb.2018.02888
23. Chang YY, Chuang YC, Siu LK, et al. Clinical features of patients with carbapenem nonsusceptible Klebsiella pneumoniae and Escherichia coli in intensive care units: a nationwide multicenter study in Taiwan. J Microbiol Immunol Infect. 2015;48(2):219–225. doi:10.1016/j.jmii.2014.05.010
24. Prasad N, Labaze G, Kopacz J, et al. Asymptomatic rectal colonization with carbapenem-resistant Enterobacteriaceae and Clostridium difficile among residents of a long-term care facility in New York City. Am J Infect Control. 2016;44(5):525–532. doi:10.1016/j.ajic.2015.11.021
25. Giacobbe DR, Del Bono V, Mikulska M, et al. Impact of a mixed educational and semi-restrictive antimicrobial stewardship project in a large teaching hospital in Northern Italy. Infection. 2017;45(6):849–856. doi:10.1007/s15010-017-1063-7
26. Wang M, Earley M, Chen L, et al. Clinical outcomes and bacterial characteristics of carbapenem-resistant Klebsiella pneumoniae complex among patients from different global regions (CRACKLE-2): a prospective, multicentre, cohort study. Lancet Infect Dis. 2022;22(3):401–412. doi:10.1016/S1473-3099(21)00399-6
27. Chen IR, Huang PH, Wu PF, et al. Clinical characteristics and outcomes of 56 patients with pneumonia caused by carbapenem-resistant Klebsiella pneumoniae. J Glob Antimicrob Resist. 2021;25:326–330. doi:10.1016/j.jgar.2021.03.028
28. Zhang H, Guo Z, Chai Y, et al. Risk Factors for and clinical outcomes of carbapenem-resistant Klebsiella pneumoniae nosocomial infections: a retrospective study in a tertiary hospital in Beijing, China. Infect Drug Resist. 2021;14:1393–1401. doi:10.2147/IDR.S298530
29. The Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. In: CLSI Supplement M100.
30. Lim FK, Liew YX, Cai Y, et al. Treatment and outcomes of infections caused by diverse carbapenemase-producing carbapenem-resistant Enterobacterales. Front Cell Infect Microbiol. 2020;10:579462. doi:10.3389/fcimb.2020.579462
31. Loo VG, Bourgault AM, Poirier L, et al. Host and pathogen factors for Clostridium difficile infection and colonization. N Engl J Med. 2011;365(18):1693–1703. doi:10.1056/NEJMoa1012413
32. Hung YP, Cia CT, Tsai BY, et al. The first case of severe Clostridium difficile ribotype 027 infection in Taiwan. J Infect. 2015;70(1):98–101. doi:10.1016/j.jinf.2014.08.003
33. Levey AS, Eckardt KU, Tsukamoto Y, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: improving Global Outcomes (KDIGO). Kidney Int. 2005;67(6):2089–2100. doi:10.1111/j.1523-1755.2005.00365.x
34. Johnson S, Lavergne V, Skinner AM, et al. Clinical practice guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 focused update guidelines on management of Clostridioides difficile infection in adults. Clin Infect Dis. 2021;73(5):e1029–e1044. doi:10.1093/cid/ciab549
35. Zar FA, Bakkanagari SR, Moorthi KM, et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis. 2007;45(3):302. doi:10.1086/519265
36. Ponte A, Pinho R, Mota M. Fecal microbiota transplantation: is there a role in the eradication of carbapenem-resistant Klebsiella pneumoniae intestinal carriage? Rev Esp Enferm Dig. 2017;109(5):392. doi:10.17235/reed.2017.4425/2016
37. Zhang H, Wang J, Zhou W, et al. Risk factors and prognosis of carbapenem-resistant Klebsiella pneumoniae infections in respiratory intensive care unit: a retrospective study. Infect Drug Resist. 2021;14:3297–3305. doi:10.2147/IDR.S317233
38. Zhu WM, Yuan Z, Zhou HY. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection relative to two types of control patients: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2020;9(1):23. doi:10.1186/s13756-020-0686-0
39. Xiao T, Zhu Y, Zhang S, et al. A retrospective analysis of risk factors and outcomes of carbapenem-resistant Klebsiella pneumoniae bacteremia in nontransplant patients. J Infect Dis. 2020;221(Suppl2):S174–S183. doi:10.1093/infdis/jiz559
40. Lapp Z, Han JH, Wiens J, et al. Patient and microbial genomic factors associated with carbapenem-resistant Klebsiella pneumoniae extraintestinal colonization and infection. mSystems. 2021;6(2):e00177–21. doi:10.1128/mSystems.00177-21
41. Rodriguez-Villodres A, Martin-Gandul C, Penalva G, et al. Prevalence and risk factors for multidrug-resistant organisms colonization in long-term care facilities around the world: a review. Antibiotics. 2021;10(6):680. doi:10.3390/antibiotics10060680
42. van Rossen TM, Ooijevaar RE, Vandenbroucke-Grauls C, et al. Prognostic factors for severe and recurrent Clostridioides difficile infection: a systematic review. Clin Microbiol Infect. 2022;28(3):321–331. doi:10.1016/j.cmi.2021.09.026
43. Finn E, Andersson FL, Madin-Warburton M. Burden of Clostridioides difficile infection (CDI) - a systematic review of the epidemiology of primary and recurrent CDI. BMC Infect Dis. 2021;21(1):456. doi:10.1186/s12879-021-06147-y
44. Medaglia AA, Buffa S, Gioe C, et al. An emergent infectious disease: Clostridioides difficile infection hospitalizations, 10-year trend in Sicily. Infection. 2021;49(6):1221–1229. doi:10.1007/s15010-021-01683-w
45. Bovonratwet P, Bohl DD, Malpani R, et al. Incidence, risk factors, and impact of Clostridium difficile colitis following primary total Hip and knee arthroplasty. J Arthroplasty. 2018;33(1):205–210e1. doi:10.1016/j.arth.2017.08.004
46. Mishima E, Abe T. Role of the microbiota in hypertension and antihypertensive drug metabolism. Hypertens Res. 2022;45(2):246–253. doi:10.1038/s41440-021-00804-0
47. Yin L, He L, Miao J, et al. Carbapenem-resistant Enterobacterales colonization and subsequent infection in a neonatal intensive care unit in Shanghai, China. Infect Prev Pract. 2021;3(3):100147. doi:10.1016/j.infpip.2021.100147
48. Howard-Anderson JR, Earley M, Komarow L, et al. Poor outcomes in both infection and colonization with carbapenem-resistant Enterobacterales. Infect Control Hosp Epidemiol. 2022:1–7. doi:10.1017/ice.2022.4
49. Sertkaya A, Wong HH, Ertis DH, Jessup A. Societal willingness to pay to avoid mortality and morbidity from Clostridioides difficile and carbapenem-resistant Enterobacteriaceae infections in the United States. Am J Infect Control. 2019;47(5):521–526. doi:10.1016/j.ajic.2018.11.008
50. Wanla W, Katip W, Supakul S, Apiwatnakorn P, Khamsarn S. Effects of an antimicrobial restriction system on appropriate carbapenem use in a hospital without infectious diseases consultation. Int J Gen Med. 2017;10:443–449. doi:10.2147/IJGM.S145133
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



