Back to Journals » Clinical Pharmacology: Advances and Applications » Volume 9
Retrospective analysis of the effects of a highly standardized mixture of Berberis aristata, Silybum marianum, and monacolins K and KA in patients with dyslipidemia
Authors Di Pierro F , Putignano P, Ferrara T, Raiola C, Rapacioli G, Villanova N
Received 18 August 2016
Accepted for publication 28 October 2016
Published 21 December 2016 Volume 2017:9 Pages 1—7
DOI https://doi.org/10.2147/CPAA.S120032
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Arthur E. Frankel
Francesco Di Pierro,1 Pietro Putignano,2 Tarcisio Ferrara,3 Carmela Raiola,4 Giuliana Rapacioli,5 Nicola Villanova6
1Scientific Department, Velleja Research, Milan, Italy; 2Outpatient Diabetic Clinic, University Hospital San Gerardo, Monza, Italy; 3District 63, Cava de’ Tirreni-Costa d’Amalfi, Salerno, Italy; 4Outpatient Clinic “Ordine di Malta”, Naples, Italy; 5AIOR, Piacenza, Italy; 6Metabolic Disorders, S. Orsola Malpighi Hospital, Bologna, Italy
Background: Berberis aristata, because of its berberine content, and Monascus purpureus fermented rice, because of the presence of monacolins (naturally derived statins), are widely investigated food-grade ingredients used to formulate cholesterol-lowering supplements. Although they are extensively used, berberine is poorly absorbed and monacolins are poorly chemically characterized, not standardized, and possibly contaminated with toxic compounds. Silymarin is reported to enhance berberine absorption, while Monakopure™-K20 (MK-20) is a highly standardized red yeast rice containing monacolins K and KA in the ratio of 1:1 but not secondary monacolins, dehydromonacolins, or citrinin.
Aim: The effects of a cholesterol-lowering supplement (Berberol®K) containing berberine, silymarin, and MK-20 (BSM) in patients with dyslipidemia were clinically analyzed.
Methods: The clinical role of BSM in naïve and in statin-intolerant patients was retrospectively evaluated and the effects observed were compared with those obtained in patients without treatment or treated with lovastatin.
Results: Total cholesterol, low density lipoprotein, and triglyceride levels were approximately 4%, 6%, and 11% lower, respectively, and the creatine phosphokinase increase was reduced in patients treated with BSM compared to those treated with lovastatin. Similar results were also obtained in statin-intolerant subjects where BSM was administered as add-on therapy to ezetimibe or fenofibrate.
Conclusion: BSM is a food supplement potentially useful 1) as a primary intervention in low-cardiovascular-risk subjects with dyslipidemia; 2) as add-on therapy in mildly statin-intolerant patients; and 3) in dyslipidemic patients with a negative perception of statins who prefer a treatment seen as natural.
Keywords: berberine, Berberol®K, silymarin, P-glycoprotein, cholesterol, triglycerides, Monascus purpureus, Monakopure™-K20
Introduction
Atherosclerosis plays a central role in the development of cardiovascular disease, the leading cause of death in Western countries.1 During the atherosclerotic process, cholesterol, mainly in the form of low density lipoprotein (LDL), accumulates in the walls of arteries, generating plaque which then obstructs the artery.2 Several drugs have been recently developed to lower cholesterol. The most commonly used are statins, also known as 3-hydroxy-3-methyl-glutaryl coenzyme A reductase inhibitors.3 They reduce cholesterol effectively but have potential side effects such as muscle pain, fatigue, and weakness, together with creatine phosphokinase (CPK) and liver enzyme increases.4 Consequently, especially in the case of low cardiovascular risk, physicians and consumers are now considering nutraceutical supplements,5 including berberine from Berberis aristata extract because of its hypocholesterolemic and anti-hyperglycemic properties.6-10 However, berberine has low oral bioavailability,11 which in humans appears to be mainly due to a P-glycoprotein (P-gp)-mediated gut extrusion process.12 The amount of berberine capable of crossing enterocytes seems to be reduced by approximately 90% by P-gp, which suggests that either the use of a potential P-gp inhibitor13 or chemical modification of berberine allowing it to overcome P-gp antagonism14 may enhance its poor oral bioavailability, thus increasing its clinical effectiveness. Among the potential P-gp inhibitors, silymarin from Silybum marianum, traditionally used as a liver protectant, is considered a good candidate owing to its very high safety profile.15 Combined B. aristata and S. marianum extracts have been shown to be more clinically effective in reducing cholesterol and glycemia than B. aristata extract alone16 and have proven efficacy in both diabetic and non-diabetic patients.17–21
Another nutraceutical agent used widely as a natural cholesterol controller is red yeast rice (RYR), a relatively safe extract derived from Monascus purpureus rice fermentation.22 The cholesterol-lowering effects of RYR are due to its content of monacolins, which are naturally derived statins.23 Recently, RYR has been formulated together with berberine from B. aristata.24 This association is thought to generate pharmacodynamic synergy due to the opposing effects exerted by berberine and monacolins on PCSK9.25 As silymarin is a pharmacokinetic enhancer of berberine, and berberine is a pharmacodynamic improver of monacolins, we studied a highly standardized mixture (Berberol®K) of berberine, silymarin, and MK-20 (BSM) in non-diabetic statin-tolerant and statin-intolerant subjects with dyslipidemia, comparing its effects to treatment with lovastatin and to no treatment in subjects with low cardiovascular risk.
Patients and methods
Study
The current study is a retrospective and controlled analysis of a 6-month routine use of a nutraceutical supplement (BSM), with possible hypocholesterolemic and anti-hyperglycemic properties, in subjects with dyslipidemia. The trial and retrospective analyses were conducted in accordance with the principles stated in the Declaration of Helsinki and were consistent with Good Clinical Practice, as defined by the International Conference on Harmonization and in accordance with the ethical principles underlying European Union Directive 2001/20/EC and the United States Code of Federal Regulations, Title 21, Part 50 (21CFR50).26 Ethics approval was obtained from Azienda Unità Sanitaria Locale (AUSL) Piacenza Ethical Board for this study. Written informed consent was obtained from all participants. Food supplement use in different outpatient clinics and hospitals in Italy (Piacenza, Bologna, Salerno, and Naples) between October 2015 and June 2016 were analyzed.
Patients
Potential patients, identified from reviewing case notes and/or computerized clinic registers, were contacted by the investigators in person or by telephone. A total of 226 patients diagnosed with dyslipidemia were enrolled for this retrospective analysis. Of these, 72 served as untreated controls and 69 as treated controls (lovastatin 20 mg/day), 67 were treated with the food supplement, and 18 were statin-intolerant subjects treated with the food supplement as add-on therapy to Absorcol®, Ezetrol®, and Zetia® (ezetimibe; 10 mg/day) or Fulcro® (fenofibrate; 200 mg/day).
Inclusion and exclusion criteria
European subjects aged ≥18 years of both sexes were considered eligible for our retrospective analysis if they had a diagnosis of hypercholesterolemia according to the 2016 European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) Guidelines for the Management of Dyslipidaemias and Atherosclerosis criteria, ie, LDL cholesterol >100 mg/dL and total cardiovascular risk score between 1% and 9%.27 All patients were treated according to the routine clinical practice. Subjects in the untreated group were considered eligible for our retrospective analysis if their total cholesterol was between 200 and 240 mg/dL and triglycerides were <400 mg/dL. Patients with a diagnosis of statin intolerance were considered eligible for our analysis if, following correct statin use, they showed a CPK increase that was 3–10 times higher than the upper laboratory limit, and/or a rise in transaminase values 3–5 times higher than the upper laboratory limit, and/or asthenia or myalgia. All subjects included in our study were overweight or obese (body mass index [BMI] between 25.0 and 40.0 kg/m2) and normotensive (systolic pressure <140 mmHg and diastolic pressure <90 mmHg). Patients were excluded from our analysis if they had secondary dyslipidemia, impaired hepatic or renal function, endocrine or gastroenterological disorders, current or previous heart disease or stroke, malignancy or suspected malignancy, neurological or psychiatric diseases, or a history of alcohol and/or drug abuse.
Product
The effect of the consumption of a finished food supplement in the form of a tablet and containing 500 mg/dose of berberine from B. aristata (extract tritation: 96% as berberine), 105 mg/dose of silymarin from S. marianum (extract tritation: ≥60% as flavanolignans), and 50 mg/dose of Monakopure™-K20 (MK-20) from M. purpureus fermented rice extract (extract tritations: 20% monacolins K and KA in the ratio 1:1; secondary monacolins J, JA, M, MA, L, LA, X, and XA, plus dehydromonacolins DMK, DMJ, DMM, DML, and DMX <0.2% in total; and citrinin <50 ppb) were retrospectively analyzed.28 The finished product was notified to the Italian Ministry of Health as Berberol®K, hereafter referred to as BSM, by PharmExtracta (Pontenure, PC, Italy), according to the provisions of law No 169 of 2004, on May 2015 (notification number: 77055). BSM is a food supplement manufactured by Labomar (Istrana, TV, Italy) using food-grade active ingredients and excipients. The B. aristata and S. marianum extracts are provided by Labomar, and MK-20 by Labiotre (Tavarnelle Val di Pesa, FI, Italy). BSM was administered once a day after the main meal.
Diet and lifestyle
At the beginning of treatment, all participants were instructed to follow a hypocaloric, low-glycemic-index diet. The controlled-energy diet (with a daily caloric deficit of about 500–600 kcal) was based on National Cholesterol Education Program-Adult Treatment Panel III recommendations29 with 50% of calories provided by carbohydrates, 30% by fat (<7% saturated, up to 10% polyunsaturated, and up to 20% monounsaturated fat), and 20% by protein, with a maximum cholesterol content of 300 mg/day, and 35 g/day of fiber. Participants were also encouraged to perform regular physical activity three or four times a week (riding a stationary bike for 20–30 minutes, or brisk walking for 30 minutes).
Outcomes
The aim of this study was to retrospectively evaluate the following clinical outcomes in patients with dyslipidemia: body weight, BMI (calculated as weight in kilograms divided by the square of the height in meters), waistline (measured midway between the lateral lower rib margin and the iliac crest), fasting blood glucose, glycated hemoglobin, basal insulin, homeostatic model assessment of insulin resistance (calculated as fasting blood glucose × basal insulin/405), total cholesterol (TC), LDL, high density lipoprotein-cholesterol, triglycerides, CPK, creatinine, thyroid-stimulating hormone, aspartate aminotransferase, and alanine aminotransferase. Treatment tolerability was assessed through patient interview and comparison of clinical and laboratory values with baseline levels.
Statistical analysis
Between-subjects and within-subjects analysis of variance and analysis of covariance were used for analysis depending on the variables being considered. A multiple comparison test (Tukey’s honest significant difference) was used to analyze possible differences between average values during the observation period. The α level was set at 0.05 and values were considered significant at P<0.05. NCSS 8 (NCSS, Kaysville, UT, USA) and JMP 10 (SAS Institute, Cary, NC, USA) software packages were used for analysis.
Results
This study is a retrospective analysis of changes in clinical outcomes following 6-month treatment with BSM in 226 patients with dyslipidemia. Seventy-two of these subjects, considered to be at low cardiovascular risk, were left untreated; 69 were treated with 20 mg/day of lovastatin; 67 were treated with BSM; and 18, considered statin-intolerant and already receiving ezetimibe (10 mg/day) or fenofibrate (200 mg/day) for 6 months or more, received add-on therapy with BSM to improve their suboptimal lipid control.
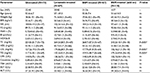
Table 1 shows that the four groups were similar regarding all parameters except dyslipidemia. Subjects from all groups were overweight, with a BMI ranging from 25.0 and 40.0 kg/m2. Subjects in the first group were not treated as they were at low cardiovascular risk due to their TC and TG values (200–240 mg/dL and <400 mg/dL, respectively) and the absence of other cardiovascular risk factors; these patients were asked to improve their diet and amount of physical activity. Subjects in the second and third groups with worse hypercholesterolemia were treated with lovastatin or BSM, respectively. The statin-intolerant subjects in the fourth group, who were already receiving treatment with ezetimibe or fenofibrate to control their cholesterol levels, were given BSM as add-on therapy. At enrollment, this fourth group was already under treatment with drugs since not less than 6 months. This accounts for why at T=0 their lipidic values are the lowest between the four groups.
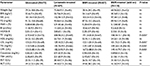
Table 2 shows that TC, LDL, TG, and CPK levels were statistically different among the groups after 6 months of treatment with BSM. TC, LDL, and TG levels varied because of different starting values and different treatments, while the significant difference in CPK values between the untreated and lovastatin-treated groups was likely due to administration of the statin.
Table 3 provides the percentage and statistical differences between the values recorded at T=6 months (Table 2) and T=0 (Table 1) within the same treatment groups. Glycated hemoglobin and homeostatic model assessment of insulin resistance values were significantly lower (by approximately 9% and 15%, respectively) in the two groups treated with BSM, likely due to the berberine content of the tablets. Lovastatin significantly reduced TC, LDL, and TG by approximately 21%, 26%, and 8%, respectively, while BSM significantly reduced TC, LDL, and TG by approximately 25%, 31%, and 19%, respectively. In statin-intolerant subjects, BSM significantly reduced TC, LDL, and TG by approximately 25%, 25%, and 14%, respectively. Lovastatin was the only treatment to significantly affect CPK, increasing it by approximately 34%, although BSM, likely due to its content of 10 mg/dose of monacolins K and KA, showed a non-significant tendency to increase CPK by approximately 12%. Increases in liver enzyme values observed in groups treated with lovastatin or BSM were not significant.
No effect or differences between groups were observed in terms of weight. This could be linked to a possible low adherence to the prescribed diet and lifestyle changes.
Concerning side effects, no differences in gastric pain, gastric reflux, insomnia, headache, or skin rash were observed between the four groups. However, considerable differences were observed regarding moderate constipation, meteorism, and flatulence in approximately 18% of the subjects treated with BSM, likely due to its content of berberine, which has anti-diarrheal activity.30 Our analysis revealed good compliance in all groups with only mild side effects and no drop-out (data not shown).
Discussion
A retrospective analysis comparing the effect on dyslipidemia of 1) diet modification and physical exercise (lifestyle intervention); 2) lifestyle intervention plus lovastatin; 3) lifestyle intervention plus a food supplement containing berberine, silymarin, and monacolins K and KA from RYR; and 4) lifestyle intervention plus the food supplement as add-on therapy to ezetimibe or fenofibrate prescribed because of statin intolerance was conducted. The results of the analysis indicated that the lifestyle intervention has poor efficacy but confirmed the cholesterol-lowering action of lovastatin and its ability to enhance CPK values. Also the analysis confirmed that food supplements containing proper doses of either berberine and silymarin or berberine and RYR significantly improved the lipid profile of patients. In light of the modest CPK increase observed, our results also suggested the possible safety of add-on therapy with food supplements containing low doses of RYR in statin-intolerant subjects. Our finding is likely due to the low content (10 mg/dose/day) of monacolins administered. We speculate that higher dosages, comparable to those of the lovastatin-treated group, would have likely generated the same CPK increase. However, lovastatin-induced CPK elevation was not clinically significant and did not lead to treatment discontinuation. Furthermore, the last 2016 ESC/EAS guidelines recommend the follow-up of muscular pain instead of CPK level monitoring in asymptomatic patients. Our analysis also suggests that treatment with BSM is better than treatment with lovastatin: TC, LDL, and TG values were approximately 4%, 6%, and 11% lower and the CPK increase reduced, but non-significant, following BSM alone compared to lovastatin treatment. Similar results were obtained for TC, TG, and CPK when BSM was administered as add-on therapy to ezetimibe or fenofibrate. Likely the considerable LDL decreases due to ezetimibe or fenofibrate reduced the ability of BSM to further lower this value.
Our work has some limitations and possible bias which may have affected our results. It was not a prospective study, with endpoints determined before study commencement, but a retrospective evaluation carried out according to clinical practice guidelines; drugs or supplements were not administered under blind conditions; subjects were not randomized; the study size was fairly small; and the group treated with add-on BSM contained only 18 subjects.
To our knowledge, this is one of the first clinical testing of a food supplement containing RYR derivative where the raw material, the extract, has been modified and highly standardized. The widespread use of RYR is mainly due to its content of monacolin K, a natural-derived form of lovastatin. Both are pro-drugs and need to be metabolized to their acid forms, respectively, KA and β-hydroxyl-acid-lovastatin, to inhibit 3-hydroxy-3-methyl-glutaryl coenzyme A reductase. Lovastatin pharma products contain, as a unique active ingredient, lovastatin. Differently, RYR besides monacolin K, also contains secondary monacolins such as J, L, X, and M along with their acid forms named KA, JA, LA, XA, and MA. Furthermore, RYR contains some degradation products derived from monacolins, named dehydromonacolins (particularly DMK). Secondary monacolins are poorly active, while dehydromonacolins are inactive and likely cytotoxic.31-33 Due to this non-standardized chemical complexity, biological effects of fermented red yeast extracts are difficult to evaluate.34 Besides the issue of non-standardization, a more important issue, safety, regards RYR. RYR extracts, in fact, besides containing the cytotoxic dehydromonacolins and statins, the latter even if naturally derived could generate important side effects,35-38 can contain a third harmful ingredient named citrinin, a secondary toxic metabolite produced by fermentation and endowed with nephrotoxicity, hepatotoxicity, and maybe carcinogenic, in humans and animals.39,40 RYR used to formulate BSM contains <50 ppb citrinin, only monacolins K and KA in a ratio of 1:1, corresponding to 5 mg/dose per each molecule, and <0.2% secondary monacolins together with dehydromonacolins. Because of its chemical profile,28 we consider this RYR extract safer than the usually marketed RYR products and a better guarantee especially for those consumers, at low cardiovascular risk, who prefer to use a “natural” treatment instead of statins as primary intervention due to dyslipidemia. In conclusion, if these results were to be confirmed by future studies, in accordance with ESC/EAS guidelines, BSM might be considered a safe and effective hypolipidemic tool in the management of low cardiovascular risk patients displaying a LDL value <190 mg/dL, and as “add-on therapy” to achieve lipidic targets in statin-intolerant subjects taking ezetimibe or fenofibrate.
Disclosure
FDP is a member of the Scientific Council of PharmExtracta, the company marketing Berberol®K. The authors report no other conflicts of interest in this work.
References
Müller-Nordhorn J, Binting S, Roll S, Willich SN. An update on regional variation in cardiovascular mortality within Europe. Eur Heart J. 2008;29(10):1316–1326. | ||
Borén J, Williams KJ. The central role of arterial retention of cholesterol-rich apolipoprotein-B-containing lipoproteins in the pathogenesis of atherosclerosis: a triumph of simplicity. Curr Opin Lipidol. 2016;27(5):473–483. | ||
Stefanutti C, Morozzi C, Di Giacomo S. New clinical perspectives of hypolipidemic drug therapy in severe hypercholesterolemia. Curr Med Chem. 2012;19(28):4861–4868. | ||
McClure DL, Valuck RJ, Glanz M, Hokanson JE. Systematic review and meta-analysis of clinically relevant adverse events from HMG CoA reductase inhibitor trials worldwide from 1982 to present. Pharmacoepidemiol Drug Saf. 2007;16(2):132–143. | ||
Derosa G, Limas CP, Macías PC, Estrella A, Maffioli P. Dietary and nutraceutical approach to type 2 diabetes. Arch Med Sci. 2014;10(2):336–344. | ||
Zhang Y, Li X, Zou D, et al. Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. J Clin Endocrinol Metab. 2008;93(7):2559–2565. | ||
Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57(5):712–717. | ||
Dong H, Zhao Y, Zhao L, Lu F. The effects of berberine on blood lipids: a systemic review and meta-analysis of randomized controlled trials. Planta Med. 2013;79(6):437–446. | ||
Dong H, Wang N, Zhao L, Lu F. Berberine in the treatment of type 2 diabetes mellitus: a systemic review and meta-analysis. Evid Based Complement Alternat Med. 2012;2012:591654. | ||
Derosa G, Maffioli P, Cicero AF. Berberine on metabolic and cardiovascular risk factors: an analysis from preclinical evidences to clinical trials. Expert Opin Biol Ther. 2012;12(8):1113–1124. | ||
Chen W, Miao YQ, Fan DJ, et al. Bioavailability study of berberine and the enhancing effects of TPGS on intestinal absorption in rats. AAPS PharmSciTech. 2011;12(2):705–711. | ||
Pan GY, Wang GJ, Liu XD, Fawcett JP, Xie YY. The involvement of P-glycoprotein in berberine absorption. Pharmacol Toxicol. 2002;91(4):193–197. | ||
Chae HW, Kim IW, Jin HE, Kim DD, Chung SJ, Shim CK. Effect of ion-pair formation with bile salts on the in vitro cellular transport of berberine. Arch Pharm Res. 2008;31(1):103–110. | ||
Shan YQ, Ren G, Wang YX, et al. Berberine analogue IMB-Y53 improves glucose-lowering efficacy by averting cellular efflux especially P-glycoprotein efflux. Metabolism. 2013;62(3):446–456. | ||
Zhou S, Lim LY, Chowbay B. Herbal modulation of P-glycoprotein. Drug Metab Rev. 2004;36(1):57–104. | ||
Di Pierro F, Putignano P, Villanova N, Montesi L, Moscatiello S, Marchesini G. Preliminary study about the possible glycemic clinical advantage in using a fixed combination of Berberis aristata and Silybum marianum standardized extracts versus only Berberis aristata in patients with type 2 diabetes. Clin Pharmacol. 2013;5:167–174. | ||
Derosa G, Bonaventura A, Bianchi L, et al. Berberis aristata/Silybum marianum fixed combination on lipid profile and insulin secretion in dyslipidemic patients. Expert Opin Biol Ther. 2013;13(11):1495–1506. | ||
Derosa G, Bonaventura A, Bianchi L, et al. Effects of Berberis aristata/Silybum marianum association on metabolic parameters and adipocytokines in overweight dyslipidemic patients. J Biol Regul Homeost Agents. 2013;27(3):717–728. | ||
Derosa G, Romano D, D’Angelo A, Maffioli P. Berberis aristata combined with Silybum marianum on lipid profile in patients not tolerating statins at high doses. Atherosclerosis. 2015;239(1):87–92. | ||
Di Pierro F, Villanova N, Agostini F, Marzocchi R, Soverini V, Marchesini G. Pilot study on the additive effects of berberine and oral type 2 diabetes agents for patients with suboptimal glycemic control. Diabetes Metab Syndr Obes. 2012;5:213–217. | ||
Di Pierro F, Bellone I, Rapacioli G, Putignano P. Clinical role of a fixed combination of standardized Berberis aristata and Silybum marianum extracts in diabetic and hypercholesterolemic patients intolerant to statins. Diabetes Metab Syndr Obes. 2015;8:89–96. | ||
Li Y, Jiang L, Jia Z, et al. A meta-analysis of red yeast rice: an effective and relatively safe alternative approach for dyslipidemia. PLoS One. 2014;9(6):e98611. | ||
Li X, Liu C, Duan Z, Guo S. HMG-CoA reductase inhibitors from Monascus-fermented rice. J Chem. 2013:2013;872056. | ||
Millán J, Cicero AF, Torres F, Anguera A. Effects of a nutraceutical combination containing berberine (BRB), policosanol, and red yeast rice (RYR), on lipid profile in hypercholesterolemic patients: a meta-analysis of randomised controlled trials. Clin Investig Arterioscler. 2016;28(4):178–187. | ||
Cameron J, Ranheim T, Kulseth MA, Leren TP, Berge KE. Berberine decreases PCSK9 expression in HepG2 cells. Atherosclerosis. 2008;201(2):266–273. | ||
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Postgrad Med. 2002;48(3):206–208. | ||
Atherosclerosis. 2016 ESC/EAS Guidelines for the Management of Dyslipidaemias. Available from: http://dx.doi.org/10.1016/j.atherosclerosis.2016.08.018. Accessed October 20, 2016. | ||
Nannoni G, Alì A, Di Pierro F. Development of a new highly standardized and granulated extract from Monascus purpureus with a high content of monacolin K and KA and free of inactive secondary monacolins and citrinin. Nutrafoods. 2015;14(4):197–205. | ||
NCEP. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. | ||
Chen C, Yu Z, Li Y, Fichna J, Storr M. Effects of berberine in the gastrointestinal tract – a review of actions and therapeutic implications. Am J Chin Med. 2014;42(5):1053–1070. | ||
Huang HN, Hua YY, Bao GR, Xie LH. The quantification of monacolin K in some red yeast rice from Fujian province and the comparison of the other product. Chem Pharm Bull (Tokyo). 2006;54(5):687–689. | ||
Gordon RY, Cooperman T, Obermeyer W, Becker DJ. Marked variability of monacolin levels in commercial red yeast rice products: buyer beware! Arch Intern Med. 2010;170(19):1722–1727. | ||
Zhu L, Yau LF, Lu JG, et al. Cytotoxic dehydromonacolins from red yeast rice. J Agric Food Chem. 2012;60(4):934–939. | ||
Gordon RY, Becker DJ. The role of red yeast rice for the physician. Curr Atheroscler Rep. 2011;13(1):73–80. | ||
Prasad GV, Wong T, Meliton G, Bhaloo S. Rhabdomyolysis due to red yeast rice (Monascus purpureus) in a renal transplant recipient. Transplantation. 2002;74(8):1200–1201. | ||
Halbert SC, French B, Gordon RY, et al. Tolerability of red yeast rice (2,400 mg twice daily) versus pravastatin (20 mg twice daily) in patients with previous statin intolerance. Am J Cardiol. 2010;105(2):198–204. | ||
Kuncl RW. Agents and mechanisms of toxic myopathy. Curr Opin Neurol. 2009;22(5):506–515. | ||
Klimek M, Wang S, Ogunkanmi A. Safety and efficacy of red yeast rice (Monascus purpureus) as an alternative therapy for hyperlipidemia. P T. 2009;34(6):313–327. | ||
Lin YL, Wang TH, Lee MH, Su NW. Biologically active components and nutraceuticals in the Monascus-fermented rice: a review. Appl Microbiol Biotechnol. 2008;77(5):965–973. | ||
Flajs D, Peraica M. Toxicological properties of citrinin. Arh Hig Rada Toksikol. 2009;60(4):457–464. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.