Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Retention in Care and Health Outcomes of HIV-Exposed Infants in a Prevention of Mother-to-Child Transmission of HIV (PMTCT) Cohort in Addis Ababa, Ethiopia
Received 12 October 2020
Accepted for publication 19 January 2021
Published 10 February 2021 Volume 2021:13 Pages 171—179
DOI https://doi.org/10.2147/HIV.S286347
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Andamlak Gizaw Alamdo,1 Elizabeth J King2
1Department of Public Health, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 2Department of Health Behavior and Health Education, School of Public Health, University of Michigan, Ann Arbor, MI, USA
Correspondence: Andamlak Gizaw Alamdo
Department of Public Health, St. Paul’s Hospital Millennium Medical College, PO Box 1271, Swaziland Street, Addis Ababa, Ethiopia
Tel +251 912038993
Email [email protected]
Purpose: Currently, a high number of mother–infant cohorts do not complete the full cascade of prevention of mother-to-child transmission of HIV (PMTCT) services in Ethiopia. This study examined the level of HIV-exposed infants discharged negative and rate of loss to follow-up (LTFU) in a mother–infant cohort in Addis Ababa, Ethiopia.
Methods: A retrospective cohort study was conducted in selected public health facilities of Addis Ababa. Data were abstracted from infant and mother registration cards and mother–infant cohort follow-up charts. The proportion of HIV-exposed infants discharged negative was examined. LTFU was then analyzed and a Kaplan–Meier survival curve was used to estimate Cumulative probability of LTFU among the different groups. Cox proportional hazard model was used to determine significant factors associated with LTFU.
Results: Three hundred fifty six mother–infant pairs were included in this study. The LTFU rate at the end of follow-up period was of 13.2% (95% CI= 9.83– 17.6%) and an overall HIV transmission rate of 0.61% was observed. Younger women (AHR=0.90, 95% CI = 0.83– 0.97) and those who were newly diagnosed at the time of entry to PMTCT (AHR=0.35, 95% CI = 0.18– 0.68) were less likely to complete PMTCT.
Conclusion: High retention to PMTCT services and low mother-to-child HIV transmission rate was observed. To successfully achieve the PMTCT program outcomes, more emphasis should be given to younger women and to those newly enrolled in the PMTCT program.
Keywords: PMTCT, loss to follow-up, option B+, ART, Ethiopia
Introduction
In 2017, an estimated 36.9 million people were living with HIV globally. The percentage of people who were newly infected with HIV was 1.8 million and 940,000 million people died from AIDS-related illnesses.1,2 According to the 2016 Ethiopian Demographic and Health survey (EDHS), the national HIV prevalence among women and men age 15–49 years in Ethiopia was 0.9%, indicating the country has more than achieved the Millennium Development Goal 6 target of 2.5%.1,3 In Ethiopia, HIV prevalence is higher among women than men (1.2% versus 0.6%) and higher among women in urban areas than women in rural areas (3.6% versus 0.6%).3 HIV risk is largely driven by a lack of awareness, mobility, and risky sexual behaviors in most-at-risk populations.4
The government of Ethiopia is maximizing its efforts to rapidly reduce and subsequently eliminate mother-to-child transmission (MTCT) in order to realize the vision of an HIV-free generation by 2020. The 2012 programmatic update by WHO paved the way for implementing lifelong antiretroviral therapy (ART) for HIV-positive pregnant and lactating women and creating the opportunity for faster elimination of MTCT and for keeping the mother alive.5
The percentage of women who are accessing prevention of mother-to-child transmission (PMTCT) services in Ethiopia was 25.5% in 2010; and, it increased to 73% in 2015.6 Antenatal care-based sentinel HIV surveillance in Ethiopia in 2014 indicated a 2.2% prevalence of HIV among pregnant women. The prevalence was higher among urban resident pregnant women (3.9%) than rural residents (1.14%).7 While great success has been made in Ethiopia, over 90% of new pediatric HIV infections are the result of vertical transmission from mother-to-child. Of the estimated new HIV infections in 2014, children constitute 23%.8 Half of these new pediatric cases were due to MTCT.8
The existing literature shows that a large percentage of women in sub-Saharan Africa are lost along the PMTCT cascade.9 While the evidence on postpartum retention is sparse, depending on the setting and follow-up period, approximately 25–50% of women on ART at delivery may be lost from care during the postpartum period.10,11 Recent large-scale PMTCT trials have experienced percentages of lost to follow-up (LTFU) ranging from 3.5% at 7 months in a study conducted in Botswana12 to 14.0% at 9 months in a trial conducted in Malawi.13 A 16.5% LTFU rate was reported in a study from Northeastern Ethiopia.14 These statistics have not been previously documented in Addis, the largest city and capital of Ethiopia.
High attrition rate from PMTCT is problematic due to the increased risk of HIV-related morbidity and mortality, HIV transmission, and the development of drug-resistant HIV strains.15 According to a recent study from the northwestern part of Ethiopia; additional large-scale studies on the determinants of MTCT of HIV were recommended.16 Thus, determining the level and factors associated with mother–infant pairs’ retention in care and examining the health outcomes of HIV exposed infants can provide key insights into the barriers to completing PMTCT services and longer-term engagement in HIV care and treatment for HIV-positive mothers. Furthermore, finding ways to transition women initiating HIV treatment in the antepartum period to lifelong ART postpartum, and retaining them in ART care, will be critical to reducing both vertical and sexual HIV transmission, and to improving the mother’s health. The objective of this study was to assess the level of PMTCT service uptake and retention in care, and the health outcomes of HIV-exposed infants in a mother–infant cohort in Addis Ababa, Ethiopia.
Methods
A retrospective cohort study design was used. The study was conducted in three public health facilities of Addis Ababa, Ethiopia. The city administration is subdivided into ten sub-cities. First, three sub-cities, namely, Gulelle, Kolfe keraniyo, and Nefas silk Lafto, were selected by using a lottery method. Then, by considering the criteria such as provision of integrated MNCH/PMTCT services to HIV-positive women and the number of clients served in the facility; one hospital, namely St. Paul’s Hospital Millennium Medical College was selected from Gullele sub-city and two health centers; Kolfe Health Center and Woreda 03 Health Center were selected for the study from Kolfe keraniyo, and Nefas silk Lafto sub-cities, respectively.
Data were obtained from the registries at the selected clinics for the time period of December 2015 to November 2018. Data from all HIV-exposed infants and their mothers since the start of PMTCT service in each of the selected public health facilities were included in the study. Mother–infant pairs for which there were incomplete medical records were excluded from the study. Among 387 mother–infant pairs registered for PMTCT cascade, PMTCT follow-up information for 356 complete mother–infant pairs were included in our study (Figure 1).
 |
Figure 1 Schematic presentation of the sampling procedure in public health facilities of Addis Ababa Ethiopia, 2018. |
The data abstraction checklist was developed from the HIV-exposed infant follow-up card, ANC follow-up registration, adult HIV care and treatment follow-up registration, and intake form of Ethiopian National HIV Care and Treatment Package. Data were abstracted from infant and mother registration cards and mother–infant cohort follow-up charts. Data collectors and supervisors were recruited and trained prior to the data collection period. Ongoing data supervision ensured that data collectors properly categorized and coded all the data. All data were cleaned and checked for completeness, accuracy, outliers, missing values and consistency by the principal investigator and the supervisors, immediately after the data were collected. Double entry and comparison of the data were done to avoid entry error. All data were entered in Epi Data version 3.5.
The outcome variables of interest in this study were mother–infant pairs’ retention in care (Mother–infant pairs’ retain in HIV care until the 18–24 month follow-up period), LTFU (Loss to follow up: Mother–infant pairs who were in the PMTC service cascade and not seen within 90 days of their scheduled appointment and dropped out before the infant turned 18–24 months old), and the proportion of HIV-exposed infants who were discharged negative at the end of up the 18–24 month follow-up period. The independent variables included: baseline information about the mother and the infant, extent of time between HIV diagnosis and ART initiation, healthcare delivery, type of health facility, method of delivery, breastfeeding practices, and the clinical characteristics of the mother and the infant.
STATA SE version 13 software was used for analysis. The number (percentage, proportion) of HIV-exposed infants discharged negative was examined. LTFU was then analyzed and a Kaplan–Meier survival curve was used to estimate Cumulative probability of LTFU among the different groups with censoring on 01 November 2018, LTFU or discharged negative. To ascertain the association; variables found to be significant at the p=0.25 level in the bivariate analysis were included in the final model. Cox proportional hazard model was used to determine which factors were associated with LTFU from PMTCT services. A 95% confidence interval and hazard ratio (HR) with a p-value less than 0.05 was used to determine the statistical significance of the strength of association between the factors and the outcome variables.
Results
Baseline Description of the Mothers
A total of 356 mother–infant pairs were included in the study. The mean length of follow-up for mother–baby pairs in this period was 21.97 months. The majority of women were clients of a health center 275 (77.2%). The median age of the mothers was 29 years. The majority (68.8%) of women were already known to be HIV-positive before entry to PMTCT. Among these, 238 (96.7%) were on HAART before they enrolled in PMTCT (Table 1). Nearly 96% of the mothers were provided ferrous sulfate. More than 85% were counselled on family planning methods. And, 85% tested negative for syphilis. As part of PMTCT services, about half (48%) were provided male condoms, and about a quarter were provided with implants. Almost 91% of the pregnancies resulted in live births.
 |
Table 1 Baseline Information About the Mothers in Public Health Facilities of Addis Ababa Ethiopia, 2018 |
HIV Care Provided to Mothers
HIV care was provided to all 356 mothers. The initial CD4 count was done for 319 (89.7%) mothers. The median initial CD4 count for mothers was 462.5 with IQR (285–602.25), and the majority had an initial CD4 count of greater than 350 cells/µL. Based on the Ethiopian Option B+ PMTCT guidelines, only pregnant women with Stage I and II HIV are enrolled in the PMTCT Program. Accordingly, in this study among 356 mothers enrolled in the program, the majority were WHO clinical stage I 293 (82.3%) and 46 (12.9%) mothers were WHO clinical stage II. Nearly fifty percent of the mothers started Cotrimoxazole preventive therapy, and most women 253 (71.1%) received a fixed-dose combination of tenofovir, lamivudine, and efavirenz as the initial regimen. Among these women, 272 (76.4%) had partners who got tested for HIV and knew their HIV status. The data on partners’ HIV testing was unknown for 12 of the women.
HIV-Exposed Infants
The majority of HIV-exposed infants (HEI) started CPT prophylaxis 292 (82.0%). Most were tested for DNA/PCR 288 (80.9%) at the age of 6 weeks, and 296 (83.1%) had a negative test result. Moreover, 297 (83.4%) of HEI received nevirapine (Table 2).
 |
Table 2 HIV Care Provided to Mothers in Public Health Facilities of Addis Ababa Ethiopia, 2018 |
The proportion of HEI who had completed the follow-up period (18–24 months) was 78.65% (n=280). While 41 (11.52%) infants were lost to follow up, 32 (8.99%) transferred out of the clinic, and the remaining 3 (0.84%) died (Figure 2). After excluding the infants who were transferred out of the clinic, 86.69% of HEI in the cohort were discharged as HIV-negative. While only 2 (0.61%) HEI were HIV-positive.
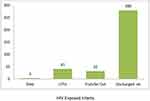 |
Figure 2 HIV-exposed infants’ status at the end of the follow-up period in public health facilities of Addis Ababa, 2018. |
Loss to Follow-Up (LTFU) and Associated Factors
Study participants were retained in care for different time periods in the cohort, which resulted in the LTFU rate of 13.2% (95% CI= 9.83–17.6%). The minimum and the maximum time to LTFU were 2 months and 23 months, respectively. A separate analysis of the rate of LTFU in three-month interval demonstrated that the period of greatest LUFU was in 3–6 months, during which time 10 (3.0%) mother–infant pairs were lost from PMTCT. An additional 9 (2.7%) participants were lost during the 6–9 month period. The LTFU rate declined after 15–18 months (0.3%).
A statistically significant difference was observed for the rate of LTFU by mother’s HIV status at the time of enrollment into PMTCT (p=0.001). Figure 3 shows the cumulative probabilities of LTFU for mothers diagnosed during their enrollment into PMTCT and mothers who were known to be HIV-positive before PMTCT. This illustrates the significantly lower rate of LTFU among the women known to HIV-positive before pregnancy.
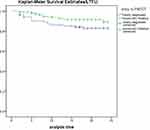 |
Figure 3 Cumulative probability of LTFU by mothers’ enrolment status in public health facilities of Addis Ababa, 2018. |
Factors significantly associated with LTFU in bivariate analysis were type of health facility (p=0.02), age of the mother (p=0.001), and HIV status at the time of entry into PMTCT (p=0.001). Mothers from health centers had 2.3 times higher risk of LTFU compared to those mothers from the hospitals [HR=2.30; 95% CI (1.41–74.84)]. The risk of LTFU for mothers in the older age group was 14% lower than the risk for younger aged mothers (HR=0.86, 95% CI = 0.80–0.92). Mothers who were diagnosed for HIV at the time of entry into PMTCT had a 74% higher risk of LTFU compared to mothers who were known to be HIV-positive before PMTCT (HR=0.26, 95% CI = 0.14–0.49). These results are presented in Table 3.
 |
Table 3 Bivariate Cox Regression Analysis of Baseline and HIV Care Information of the Mother-Infant Pair Cohort in Public Health Facilities of Addis Ababa, 2018 (N=324) |
All variables which had a significant association with LTFU at the 0.25 significant level in the bivariate analysis and WHO clinical stage (which was shown to be a risk factor in previous studies)17,18 were retained for multivariable analysis. In the adjusted model, only the mother’s age and HIV status at the time of entry into PMTCT remained significantly associated with LTFU. Mothers who were diagnosed for HIV at PMTCT had a 65% higher risk of LTFU compared to mothers who were known to be HIV-positive (AHR=0.35, 95% CI = 0.18–0.68). The risk of LTFU for the mothers with older age was 10% lower than the risk for the mothers with younger age (HR=0.86, 95% CI = 0.83–0.97). Results from the multivariable analysis are shown in Table 4.
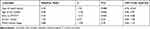 |
Table 4 Multivariable Cox Regression Analysis of Baseline and HIV Care Information of the Mother-Infant Pair Cohort in Public Health Facilities of Addis Ababa, 2018 (N=324) |
Discussion
Our study examined the proportion of HIV-exposed infants discharged negative, determined the rate of LTFU, and also identified the determinants of LTFU in a mother-infant pair cohort in Addis Ababa, Ethiopia. Our study is indicative of important changes that have been made in regard to PMTCT and mother’s access to lifetime treatment in Ethiopia. Among the total 356 mother–infant pairs, 86.69% were retained in PMTCT for a follow-up period of 18 to 24 months and infants were discharged negative. The proportion of mother–infant pairs’ retention in the care in our study was higher than the reports from Kenya19 and South Africa.18 We observed an overall HIV transmission rate of 0.61% among infants for whom DNA PCR results were available. The HIV transmission rates of 8.2% to 15.7% were reported in earlier studies in Ethiopia.20–22 A very low HIV mother-to-child transmission rate reflects the effectiveness of the current Option B+ PMTCT procedure where mothers receive a fixed dose of combined ARV regimen for life.
Although the proportion of mother–infant pairs retained in PMTCT follow-up care in our study was higher than retention reported from other studies,17,18 the rate of LTFU remains a significant challenge to achieving successful PMTCT program outcomes. In our study, an overall LTFU rate of 13.2% was reported, which is less than the level of LTFU in South Africa, where more than a third (34.9%) of mothers dropped out from one or more steps in the PMTC service cascade18 and 65% dropped out before the infant turned 18 months old in rural Kenya.19 However, it is higher than the report from a prospective cohort study conducted earlier in Addis Ababa.23 Among the reasons reported for a higher rate of LTFU from other studies were high numbers of home deliveries18,24 and the distance between the mother’s home and the healthcare facilities24 reflecting the time and cost of travel to health services. The lower rate of LTFU in our study might be due to the fact that the majority of the mothers delivered in the health institution (97.3%) and they were residing in the capital city where most of the health facilities are concentrated.
In our study, mothers who were diagnosed with HIV at enrollment in PMTCT had a 65% (AHR=0.35, 95% CI = 0.18–0.68) higher risk of LTFU compared to mothers who were already known to be HIV-positive before enrolling in PMTCT. This might be due to mothers who only recently knew their HIV status not perceiving themselves or their infants to be at risk for disease and be less likely to stay engaged in care. A similar finding was reported in a study conducted in Kericho County, Kenya.25 Accordingly, mothers knowing their HIV status pre-pregnancy was protective to LTFU (AOR=0.23 CI 0.05–0.71). Moreover, a recent prospective cohort study in Dar es Salaam, Tanzania reported that being on ART for the duration of 12 months or more prior to pregnancy was protective to LTFU from PMTCT services (p < 0.001).26 Mothers diagnosed with HIV during pregnancy may need additional interventions to ensure continued engagement throughout the PMTCT cascade.
Our study also demonstrated several factors associated with LTFU that warrant further attention in Ethiopia. Younger mothers were at higher risk of LTFU than older mothers. This finding is comparable with research from Dar es Salaam, Tanzania, where younger age (<40 years) was associated with higher LTFU risks.27 Similarly, in a South African study mother under the age of 20 had an increased risk of dropping out of the PMTCT cascade compared to older mothers.6 Mothers from health centers had 2.3 times higher risk of LTFU compared to those mothers from the hospitals (AHR=2.30; 95% CI (1.41–74.84)). However, this finding was not statistically significant in multivariable analyses. The difference may be explained by the fact that the majority (77.2%) of the study participants were from the health center, and this might make the association unstable.
Our study has limitations worth noting. First, our study relied on secondary data sources; thus, we were limited in the variables we could include in our regression models. There may be other factors associated with LTFU that were not included in this study. Second, we had to exclude mother–infant pairs for which there were incomplete medical records. Information which was not included in the study might have affected our findings. Nonetheless, the results from our large mother–infant cohort study in Addis Ababa revealed important information about women’s retention in PMTCT and the risk of LTFU.
Conclusion
In conclusion, our study indicated high rates of HEI discharged negative among a large mother–infant pair cohort and low mother-to-child HIV transmission rates. These results reflect the effectiveness of the current Option B+ PMTCT procedure in Ethiopia where mothers receive a triple ARV regimen for life.
Compared to previous studies, our study documented a lower rate of LTFU. Mothers who were diagnosed for HIV at PMTCT and younger age mothers had a higher risk to be LTFU. Program planners, higher officials at the Ministry of Health and at the national level should give special attention to the mothers who are newly enrolled in PMTCT program and younger age women. In addition, health workers should give more emphasis to mothers who are newly enrolled in PMTCT care and younger aged mothers during counseling and routinely offer healthcare services. Furthermore, more research is needed to better understand the higher rates of LTFU among women diagnosed with HIV during pregnancy, childbirth, and postpartum as this population is arguably in need of particular interventions to ensure longer-term engagement in HIV care and treatment.
Abbreviations
ART, antiretroviral treatment; HAART, highly active antiretroviral treatment; HEI, HIV-exposed infants; AHR, adjusted hazard ratio; AIDS, acquired immunodeficiency syndrome; ANC, antenatal care; CI, confidence interval; CPT, cotrimoxazole preventive therapy; HIV, human immunodeficiency virus; IQR, interquartile range; L&D, labor and delivery; LTFU, loss to follow-up; MTCT, mother-to-child transmission; PP, postpartum; WHO, World Health Organization; UNAIDS, United Nation Agency for International Development.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethical Approval
The proposal was submitted to the SPHMMC Institutional Ethical Review Committee/IERC/for ethical approval. The SPHMMC IERC approved this study, and it was conducted in accordance with the Declaration of Helsinki. At all levels, Addis Ababa City Administration, Health Bureau, and health facility officials were contacted. All the necessary explanations about the purpose of the study and its procedure was explained to them with the assurance of confidentiality of the information collected. The relevant officials provided their permission to include the data from their health facilities in this study.
Acknowledgments
We are very grateful to St. Paul’s Hospital Millennium Medical College for providing the opportunity to conduct the research through its financial support. We would also like to thank the Office of Global Public Health at the University Of Michigan School Of Public Health for supporting a short-term scholar period. Finally, we would like to acknowledge the Department of Public Health at St. Paul’s Hospital Millennium Medical College for the valuable support in each step of the research.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
St. Paul’s Hospital Millennium Medical College supported the research financially. However, the authors have declared that no financial support in authorship and publication of this article was received.
Disclosure
The authors declare that they have no financial or non-financial conflicts of interest for this work.
References
1. Joint United Nations Programme on HIV/AIDS. Global AIDS UP DATE 2016 [Internet]. UNAIDS. 2016.
2. UNAIDS. Indicators for monitoring the 2016 political declaration on ending AIDS. 2016
3. Central Statistical Agency. Ethiopia Demographic and Health Survey HIV Prevalence Report [Internet]; 2016.
4. President’s emergency plan for AIDS relief (PEPFAR) | Ethiopia | U.S. Agency for International Development [Internet]. 2018
5. WHO. Uso de medicamentos anti-retrovirais para tratar mulheres grávidas e evitar a infecção dos bebés pelo VIH. 2012;1:10.
6. Ethiopian Federal Ministry of Health. National Comprehensive PMTCT Training Participants Manual. Adama, Ethiopia: MNCH Directorate; 2016.
7. Ababa A Report on the 2014 round antenatal care based sentinel HIV surveillance in Ethiopia. 2015.
8. EPHI. HIV related estimates and projections for Ethiopia – 2017. 2017.
9. Geldsetzer P, Yapa HMN, Vaikath M, et al. A systematic review of interventions to improve postpartum retention of women in PMTCT and ART care. J Int AIDS Soc. 2016;19(1):20679. doi:10.7448/IAS.19.1.20679
10. Kurewa EN, Kandawasvika GQ, Mhlanga F, et al. Realities and challenges of a five year follow up of mother and child pairs on a PMTCT program in Zimbabwe. Open AIDS J. 2011;5(1):51–58. doi:10.2174/1874613601105010051
11. Phillips T, Thebus E, Bekker LG, et al. Disengagement of HIV-positive pregnant and postpartum women from antiretroviral therapy services: a cohort study. J Int AIDS Soc. 2014;8:17.
12. Powis KM, Smeaton L, Hughes MD, et al. In-utero triple antiretroviral exposure associated with decreased growth among HIV-exposed uninfected infants in Botswana. AIDS. 2016;30(2):211–220. doi:10.1097/QAD.0000000000000895
13. Kumwenda NI, Hoover DR, Mofenson LM, et al. Extended antiretroviral prophylaxis to reduce breast-milk HIV-1 transmission. N Engl J Med. 2008;359(2):119–129. doi:10.1056/NEJMoa0801941
14. Mitiku I, Arefayne M, Mesfin Y, et al. Factors associated with loss to follow-up among women in Option B+ PMTCT programme in northeast Ethiopia: a retrospective cohort study. J Int AIDS Soc. 2016;19(1):20662. doi:10.7448/IAS.19.1.20662
15. Thiers BH. CD4+ count–guided interruption of antiretroviral treatment. In: Year Book of Dermatology and Dermatologic Surgery 2007. 2007:156–157
16. Moges NA, Kassa GM, Boneya DJ, et al. Rate of HIV transmission and associated factors among HIV-exposed infants in selected health facilities of East and West Gojjam Zones, Northwest Ethiopia; retrospective cohort study. BMC Infect Dis. 2017;17(1). doi:10.1186/s12879-017-2578-3.
17. Chetty T, Knight S, Giddy J, et al. A retrospective study of Human Immunodeficiency Virus transmission, mortality and loss to follow-up among infants in the first 18 months of life in a prevention of mother-to-child transmission programme in an urban hospital in KwaZulu-Natal, South Africa. BMC Pediatr. 2012;12(1):146. doi:10.1186/1471-2431-12-146
18. Woldesenbet S, Jackson D, Lombard C, et al. Missed opportunities along the prevention of mother-to-child transmission services cascade in South Africa: uptake, determinants, and attributable risk (the SAPMTCTE). Anglewicz P, editor. PLoS One. 2015;10(7):e0132425. doi:10.1371/journal.pone.0132425
19. Hassan AS, Sakwa EM, Nabwera HM, et al. Dynamics and constraints of early infant diagnosis of HIV infection in rural Kenya. AIDS Behav. 2012;16(1):5–12. doi:10.1007/s10461-010-9877-7
20. Mirkuzie AH, Hinderaker SG, Sisay MM, et al. Current status of medication adherence and infant follow up in the prevention of mother to child HIV transmission programme in Addis Ababa: a cohort study. J Int AIDS Soc. 2011;14(1):1–10.
21. Koye DN, Zeleke BM. Mother-to-child transmission of HIV and its predictors among HIV-exposed infants at a PMTCT clinic in northwest Ethiopia. BMC Public Health. 2013;13(1). doi:10.1186/1471-2458-13-398.
22. Wudineh F, Damtew B. Mother-to-child transmission of HIV infection and its determinants among exposed infants on care and follow-up in Dire Dawa City, Eastern Ethiopia. AIDS Res Treat. 2016;2016:1–6. doi:10.1155/2016/3262746
23. Girma M, Wendaferash R, Shibru H, et al. Uptake and performance of prevention of mother-to-child transmission and early infant diagnosis in pregnant HIV-infected women and their exposed infants at seven health centres in Addis Ababa, Ethiopia. Trop Med Int Heal. 2017;22(6):765–775. doi:10.1111/tmi.12881
24. Lerebo W, Callens S, Jackson D, et al. Identifying factors associated with the uptake of prevention of mother to child HIV transmission programme in Tigray region, Ethiopia: a multilevel modeling approach. BMC Health Serv Res. 2014;14(1). doi:10.1186/1472-6963-14-181.
25. Kigen HT, Galgalo T, Githuku J, et al. Predictors of loss to follow up among HIV-exposed children within the prevention of mother to child transmission cascade, Kericho county, Kenya, 2016. Pan Afr Med J. 2018;30:30. doi:10.11604/pamj.2018.30.178.15837
26. Siril HN, Kaaya SF, Smith Fawzi MK, et al. CLINICAL outcomes and loss to follow-up among people living with HIV participating in the NAMWEZA intervention in Dar es Salaam, Tanzania: a prospective cohort study. AIDS Res Ther. 2017;14(1). doi:10.1186/s12981-017-0145-z.
27. Berhan Z, Abebe F, Gedefaw M, et al. Prevalence of HIV and associated factors among infants born to HIV positive women in Amhara Region, Ethiopia. Int J Clin Med. 2014;05(08):464–474. doi:10.4236/ijcm.2014.58065
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
