Back to Journals » Therapeutics and Clinical Risk Management » Volume 11
Residual disease and risk factors in patients with high-grade cervical intraepithelial neoplasia and positive margins after initial conization
Authors Fu Y , Chen C, Feng S, Cheng X , Wang X , Xie X, Lü W
Received 29 January 2015
Accepted for publication 9 March 2015
Published 21 May 2015 Volume 2015:11 Pages 851—856
DOI https://doi.org/10.2147/TCRM.S81802
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Yunfeng Fu,1,2,* Chen Chen,3,* Suwen Feng,2 Xiaodong Cheng,2 Xinyu Wang,1,2 Xing Xie,1,2 Weiguo Lü2
1Department of Gynecology, Fourth Affiliated Hospital, School of Medicine, Zhejiang University, Yiwu, 2Department of Gynecologic Oncology, Women’s Hospital, School of Medicine, Zhejiang University, Hangzhou, 3Second Hospital of Shandong University, Jinan, People’s Republic of China
*These authors contributed equally to this work
Background: The purpose of this study was to determine the clinicopathologic predictors of residual disease in patients with high-grade cervical intraepithelial neoplasia (CIN) and margin involvement after initial conization.
Methods: Data from 145 patients who underwent subsequent surgery for high-grade CIN with positive margins were retrospectively analyzed.
Results: After subsequent surgery, residual disease was diagnosed in 47 (34.2%) patients, of whom five had invasive cervical carcinoma, 31 had CIN 3, nine had CIN 2, and two had CIN 1. Multivariate analysis revealed that only age ≥35 years (P=0.033), major abnormal cytology (P=0.002), and pre-cone high-risk human papillomavirus load ≥300 relative light units (P=0.011) were significant factors associated with residual disease.
Conclusion: Age ≥35 years, major abnormal cytology, and pre-cone high-risk human papillomavirus load ≥300 relative light units were the only significant factors predicting post-cone residual disease. Appropriate application of these predictive factors may avoid delayed treatment and overtreatment.
Keywords: cervical intraepithelial neoplasia, residual disease, conization, positive margin, predictor
Introduction
High-grade cervical intraepithelial neoplasia (CIN 2–3) carries a significant risk of developing invasive carcinoma if not treated. Conization is the standard procedure for treatment of high-grade CIN, since it allows histologic confirmation of the lesion, exclusion of invasive cancer, evaluation of the resection margins, and preservation of fertility.1 For young women who desire pregnancy, the surgeon should carefully balance complete excision of the lesion and minimal cervical damage in an attempt to reduce the risk of obstetric complications.
This poses a challenge for doctors to avoid incomplete excision during conization. In fact, there is a considerably high proportion of patients who have incomplete excision after conization. Incomplete excision is undoubtedly associated with an increased risk of residual/recurrent disease being found at subsequent follow-up of women treated by conization. A comprehensive meta-analysis by Ghaem-Maghami et al revealed that the rate of positive margins after conization was about 23.0% (8,091/35,109).2 High-grade post-treatment disease occurred in 18% (597/3,335) of women who had incomplete excision versus 3% (318/12,493) of women who had complete excision.2
The optimal management of women who have had incomplete excision remains controversial. It is important to avoid overtreatment by secondary excision of uninvolved tissue. However, residual high-grade CIN or invasive carcinoma should be treated without delay. Selecting the most rational treatment modality for women with positive margins is a challenge for both patients and doctors. Therefore, better understanding of the related risk factors for residual precancer or microinvasive cancer is necessary. Accordingly, this study was conducted to determine the clinicopathologic predictors of residual disease in women who had high-grade CIN with margin involvement after initial conization.
Materials and methods
Patients and clinical data
This retrospective study included 145 patients who were diagnosed as high-grade CIN with positive margins by first conization and underwent subsequent surgical treatment at the Women’s Hospital, School of Medicine, Zhejiang University between January 2006 and December 2011. The following data were abstracted from their medical records: demographic characteristics, preoperative cervical cytology, high-risk human papillomavirus (HPV) test results, and all histologic findings. This retrospective analysis was exempt from ethics committee approval at the Women’s Hospital, School of Medicine, Zhejiang University, because the committee did not consider approval necessary for a retrospective chart review.
Initial conization and subsequent surgery (repeat conization or hysterectomy)
All operations were performed by senior doctors. In most cases, loop electrosurgical excision procedure (LEEP) was performed in an outpatient setting. The electrical power for the loop electrode was set to a blended mode. The cervix was swabbed with Lugol’s iodine solution to assist in locating the ectocervical margin of the lesion. The loop was selected according to the size of the area to be excised. When possible, the cervix lesion was excised en bloc for better orientation and margin status interpretation. When an endocervical extension was suspected, a second selective endocervical sweep was performed. When the ectocervical lesion was too large to be accommodated by a single sweep, excision was achieved with two or more systematic sweeps. The base of the resulting crater was then coagulated by ball diathermy.
Cold knife conization was performed under epidural anesthesia. The cervix was exposed using a weighted posterior vaginal retractor and right angle retractor. After delineating the area of abnormality with Lugol’s iodine solution, a circular knife cut approximately 0.5 cm outside the area not stained with iodine was made using a pointed and angled cold knife. The depth of the cone was about 2 cm. The cervicoplasty was completed using a modified Sturmdorf procedure after the necessary electrocoagulation.
All subsequent surgical treatment was performed within 3 months (median 83 days) after the first conization. We attempted to perform repeat conization as the first choice of treatment after a positive margin. Hysterectomy was carried out when repeat conization was technically impossible.
Pathologic examination
All cone specimens and the cervical part of hysterectomy were opened longitudinally and sectioned serially along the entire length of the endocervix to the ectocervix at intervals of 2–3 mm and then embedded in paraffin. The surgical margins of the cones were marked with ink. All sections were then stained with hematoxylin and eosin. Cone margin involvement in this study was defined by histologic examination as the presence of neoplastic epithelium consistent with CIN 2–3 at the margin. Residual disease was defined as the presence of any degree of CIN or invasive cancer in specimens of second surgery.
Cytology
The screening cytology was performed and evaluated according to the Bethesda system.3 The liquid-based preparation test (ThinPrep, Hologic, Inc, Bedford, MA, USA) was performed using a soft plastic spatula and endocervical cytobrush. Diagnoses were classified as negative for intraepithelial lesion or malignancy (NILM), atypical squamous cells of undetermined significance (ASCUS), low-grade squamous intraepithelial lesion (LSIL), atypical squamous cells, cannot exclude high-grade squamous intraepithelial lesion (ASC-H), high-grade squamous intraepithelial lesion (HSIL), or squamous cell carcinoma (SCC). Cytology was divided into two groups, ie, a minor abnormal group including NILM, ASCUS, and LSIL, and a major abnormal group including ASC-H, HSIL, and SCC.
Detection of high-risk HPV
Analysis of high-risk HPV was performed using Hybrid Capture II tests (Digene, Gaithersburg, MD, USA) from cervical smears according to the manufacturer’s instructions. The samples were tested for 13 oncogenic genotypes (types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68), and the results were classified as positive at a relative light unit (RLU)/cutoff ratio of ≥1 pg/mL. Light measurements were quantified using a luminometer and are expressed as the ratio between the RLU of a clinical sample and that of the positive control. The luminescence of a specimen was compared with that of a 1.0 pg/mL HPV-16 cutoff standard.
Statistical analysis
Statistical analyses were performed using Statistical Package for the Social Sciences version 16.0 software (SPSS Inc, Chicago, IL, USA). The chi-square or Fisher’s exact test was used for univariate identification of factors related to the presence of residual disease. Multivariate analysis was performed using a logistic regression model. All tests were two-sided, and the level of significance was set at P<0.05.
Results
Patient characteristics
The average age of the 145 patients was 43.6±9.1 (range 16–71) years, and 29 were postmenopausal. Gravidity was less than three in 105 patients and parity was less than two in 140 patients. The cytology before first conization showed that nine (6.2%) patients had NILM, 18 (12.4%) had ASCUS, 15 (10.3%) had LSIL, 27 (18.6%) had ASC-H, 59 (40.7%) had HSIL, and two (1.4%) had SCC. The pre-cone high-risk HPV test was positive in 99 patients and negative in 14 patients. The initial conization was performed by LEEP in 69 and cold knife conization in 76 patients. All patient demographic and clinicopathologic characteristics are summarized in Table 1.
Residual disease in specimens from subsequent surgery
After initial conization, 67 of the 145 patients underwent repeat conization (16 LEEP and 51 cold knife conization), 74 underwent hysterectomy, and four underwent radical trachelectomy; 32.4% (47/145) of the patients had residual disease in specimens from subsequent surgery (five invasive cervical carcinoma, 31 CIN 3, nine CIN 2, and two CIN 1).
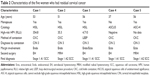
Unrecognized invasive cervical carcinoma was observed in five women who underwent extrafascial hysterectomy or modified radical hysterectomy because reconization was technically impossible. The detailed characteristics of these women are shown in Table 2.
Risk factors for residual disease
Table 3 shows the demographic and clinicopathologic variables in relation to residual disease after conization. Univariate analysis showed significantly higher percentages of residual disease in patients aged ≥35 years, those with menopause, those with major abnormal cytology (ASC-H, HSIL, and SCC), those with pre-cone high-risk HPV ≥300 RLU, and those with positive results of endocervical curettage. However, gravidity, parity, severity of disease, method of conization, glandular extension, and site of margin involvement were not significant factors. Multivariate analysis using a logistic regression model, which included all the above significant covariates, was then performed. According to this analysis, the independent factors significantly predictive of residual disease after conization were age ≥35 years, major abnormal cytology, and pre-cone high-risk HPV load ≥300 RLU (Table 3).
Discussion
The American Society for Colposcopy and Cervical Pathology recommends reassessment using cytology with endocervical sampling at 4–6 months after treatment as the preferred option if high-grade CIN is identified at the margins of conization. Repeat conization or hysterectomy, if a repeat conization is not feasible, is acceptable.4 Although most of these patients remain free of disease, the risk of residual disease or even unrecognized invasive cancer is not negligible.5 Both delayed treatment and overtreatment should be avoided with a better understanding of the risk factors in relation to residual disease.
In this study, we found that 32.4% of patients who had high-grade CIN with margin involvement after initial conization had residual disease on subsequent surgical treatment. This finding is similar to the reported incidence of about 20%–60% in previous studies.2,6–12 Additionally, the incidence of unrecognized invasive cervical carcinoma (3.4%) in this study was also comparable with previously reported incidences of 0.9%–9.6%.6,10–14
Risk factors related to CIN residual/recurrent disease after conization may include age, parity, cytologic grade, lesion grade, preoperative and follow-up HPV viral load, HPV genotype, and cone margin involvement. Most authors agree that margin involvement is one of the strongest predictors for residual/recurrent disease.15,16 However, predictors related to residual disease in patients with margin involvement remain uncertain. We systematically evaluated demographic, cytology, pre-cone high-risk HPV, and pathologic variables to determine the relationship with residual disease on second surgery. A logistic regression analysis revealed that age ≥35 years, major abnormal cytology, and pre-cone high-risk HPV load ≥300 RLU were significant independent predictors for residual disease.
Sarian et al reported that women older than 35 years had a significantly higher risk for persistent infection following LEEP, indicating older age as a predictive factor for a residual lesion or increased risk for disease recurrence.17 This is consistent with our results. A retrospective 10-year chart review showed that increasing age and severity of disease in the cone specimen were the only factors that accurately predicted residual dysplasia.8 The odds ratio of residual disease in the hysterectomy specimen for a 40-year-old woman whose odds ratio was 4.9 (95% confidence interval 2.2–10.8) compared with a 25-year-old woman was 2.7 (95% confidence interval 1.6–4.4).
Ryu et al reported that cytologic grade before LEEP was not a significant factor for residual disease or recurrence.18 In contrast, Ayhan et al showed that an HSIL result on a Papanicolaou smear was advantageous for predicting cancer in the repeat conization specimen of women with CIN 3 and a positive ectocervical margin.19 In the present study, cytology was divided into two groups, ie, minor abnormalities included NILM, ASCUS, and LSIL, and major abnormalities included ASC-H, HSIL, and SCC. We found that cytologic grade before conization was also a significant factor for residual disease.
High pre-conization high-risk HPV viral load as a predictor of residual/recurrent disease has been studied by several investigators.20,21 In our study, high-risk HPV viral load, using a cutoff of ≥300 RLU, was a significant risk factor for predicting residual disease after incomplete conization, in agreement with a previous report.11 Ryu et al reported contradictory results; however, they used RLU of 100 as the cutoff value for a high viral load.18
Although specific characteristics of patients with unrecognized invasive cancer could not be closely addressed in the present study due to the small study population, we found that 80% (4/5) of these women were postmenopausal. Consequently, the post-treatment surveillance for postmenopausal women who had margin involvement with high-grade CIN should be undertaken carefully if secondary surgery has not been performed.
In summary, multivariate analysis showed that age ≥35 years, major abnormal cytology, and pre-cone high-risk HPV load ≥300 RLU were predictive of post-cone residual disease for women who had margin involvement with high-grade CIN. Appropriate application of these predictive factors may further decrease the incidence of delayed treatment and over treatment.
Acknowledgments
This work was supported by the Foundation of Science and Technology Department of Zhejiang Province, People’s Republic of China (2012C13019-3, N20130174) and Special Fund for Scientific Research in the Public Interest from the National Health and Family Planning Commission of the People’s Republic of China (201402010).
Disclosure
The authors report no conflicts of interest in this work.
References
Prendiville W. The treatment of CIN: what are the risks? Cytopathology. 2009;20(3):145–153. | ||
Ghaem-Maghami S, Sagi S, Majeed G, Soutter WP. Incomplete excision of cervical intraepithelial neoplasia and risk of treatment failure: a meta-analysis. Lancet Oncol. 2007;8(11):985–993. | ||
Solomon D, Davey D, Kurman R, et al; Forum Group Members, Bethesda 2001 Workshop. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002;287(16):2114–2119. | ||
Massad LS, Einstein MH, Huh WK, et al; 2012 ASCCP Consensus Guidelines Conference. 2012 updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2013;17(5 Suppl 1):S1–S27. | ||
Höckel M. Insights into incomplete excision. Lancet Oncol. 2007;8(11):957–959. | ||
Husseinzadeh N, Shbaro I, Wesseler T. Predictive value of cone margins and post-cone endocervical curettage with residual disease in subsequent hysterectomy. Gynecol Oncol. 1989;33(2):198–200. | ||
White CD, Cooper WL, Williams RR. Cervical intraepithelial neoplasia extending to the margins of resection in conization of the cervix. J Reprod Med. 1991;36(9):635–638. | ||
Moore BC, Higgins RV, Laurent SL, Marroum MC, Bellitt P. Predictive factors from cold knife conization for residual cervical intraepithelial neoplasia in subsequent hysterectomy. Am J Obstet Gynecol. 1995;173(2):361–366. | ||
Mohamed-Noor K, Quinn MA, Tan J. Outcomes after cervical cold knife conization with complete and incomplete excision of abnormal epithelium: a review of 699 cases. Gynecol Oncol. 1997;67(1):34–38. | ||
Kietpeerakool C, Khunamornpong S, Srisomboon J, Siriaunkgul S, Suprasert P. Cervical intraepithelial neoplasia II–III with endocervical cone margin involvement after cervical loop conization: is there any predictor for residual disease? J Obstet Gynaecol Res. 2007;33(5):660–664. | ||
Park JY, Lee SM, Yoo CW, Kang S, Park SY, Seo SS. Risk factors predicting residual disease in subsequent hysterectomy following conization for cervical intraepithelial neoplasia (CIN) III and microinvasive cervical cancer. Gynecol Oncol. 2007;107(1):39–44. | ||
Siriaree S, Srisomboon J, Kietpeerakool C, et al. High-grade squamous intraepithelial lesion with endocervical cone margin involvement after cervical loop electrosurgical excision: what should a clinician do? Asian Pac J Cancer Prev. 2006;7(3):463–466. | ||
Huang LW, Hwang JL. A comparison between loop electrosurgical excision procedure and cold knife conization for treatment of cervical dysplasia: residual disease in a subsequent hysterectomy specimen. Gynecol Oncol. 1999;73(1):12–15. | ||
Natee J, Therasakvichaya S, Boriboonhirunsarn D. Prevalence and risk factors for residual cervical neoplasia in subsequent hysterectomy following LEEP or conization. J Med Assoc Thai. 2005;88(10):1344–1348. | ||
Lu CH, Liu FS, Kuo CJ, Chang CC, Ho ES. Prediction of persistence or recurrence after conization for cervical intraepithelial neoplasia III. Obstet Gynecol. 2006;107(4):830–835. | ||
Serati M, Siesto G, Carollo S, et al. Risk factors for cervical intraepithelial neoplasia recurrence after conization: a 10-year study. Eur J Obstet Gynecol Reprod Biol. 2012;165(1):86–90. | ||
Sarian LO, Derchain SF, Andrade LA, Tambascia J, Morais SS, Syrjänen KJ. HPV DNA test and Pap smear in detection of residual and recurrent disease following loop electrosurgical excision procedure of high-grade cervical intraepithelial neoplasia. Gynecol Oncol. 2004;94(1):181–186. | ||
Ryu A, Nam K, Kwak J, Kim J, Jeon S. Early human papillomavirus testing predicts residual/recurrent disease after LEEP. J Gynecol Oncol. 2012;23(4):217–225. | ||
Ayhan A, Boynukalin FK, Guven S, Dogan NU, Esinler I, Usubutun A. Repeat LEEP conization in patients with cervical intraepithelial neoplasia grade 3 and positive ectocervical margins. Int J Gynaecol Obstet. 2009;105(1):14–17. | ||
Houfflin Debarge V, Collinet P, Vinatier D, et al. Value of human papillomavirus testing after conization by loop electrosurgical excision for high-grade squamous intraepithelial lesions. Gynecol Oncol. 2003;90(3):587–592. | ||
Alonso I, Torné A, Puig-Tintoré LM, et al. Pre- and post-conization high-risk HPV testing predicts residual/recurrent disease in patients treated for CIN 2–3. Gynecol Oncol. 2006;103(2):631–636. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.