Back to Journals » Pragmatic and Observational Research » Volume 6
Remission, response, and relapse rates in patients with acute schizophrenia treated with olanzapine monotherapy or other atypical antipsychotic monotherapy: 12-month prospective observational study
Authors Takahashi M, Nakahara N, Fujikoshi S, Iyo M
Received 27 March 2014
Accepted for publication 31 December 2014
Published 14 July 2015 Volume 2015:6 Pages 39—46
DOI https://doi.org/10.2147/POR.S64973
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Michihiro Takahashi,1 Naohiro Nakahara,2 Shinji Fujikoshi,3 Masaomi Iyo4
1Takahashi Psychiatric Clinic, Ashiya, Hyogo, Japan; 2Zimmer KK, Tokyo, Japan; 3Lilly Research Laboratories Japan, Lilly Japan KK, Kobe, Japan; 4Department of Psychiatry, Graduate School of Medicine, Chiba University, Chiba, Japan
Purpose: To compare the rates of antipsychotic response, remission, and relapse in patients with schizophrenia treated with olanzapine or other antipsychotics in usual clinical care in Japan.
Patients and methods: This analysis of a 12-month, prospective, noninterventional study examined outcomes for 1,089 inpatients and outpatients with schizophrenia who initiated antipsychotic monotherapy. All treatment decisions, including medication choice, were left to the discretion of the treating physician. The rates of treatment response, relapse, and 6-month sustained remission were compared between olanzapine monotherapy (OLZ) and other antipsychotic monotherapy (OAN), and between OLZ and other atypical antipsychotic monotherapy (OAT). Visit-wise comparisons of treatment response and remission were examined using repeated-measures logistic regressions. Propensity scores were used to control for potential baseline differences between groups.
Results: Response rates were higher for OLZ patients and relapse rates were consistently lower for OLZ patients, however the differences were not statistically significant. Rates of 6-month sustained remission were significantly higher for OLZ than OAN patients (P=0.032) and for OLZ than OAT patients (P=0.041). An exploratory analysis of OLZ and OAN comparison found outpatients treated with OLZ or OAN had similar sustained remission rates (OLZ: 22.2%, OAN: 22.8%), while inpatients treated with OLZ had significantly higher sustained remission rates than inpatients treated with OAN (OLZ: 17.1%, OAN: 6.6%, odds ratio [95% confidence interval] =3.54 [2.00–6.25]).
Conclusion: In usual care in Japan, treating the acute symptoms of schizophrenia with olanzapine was not found to be significantly different for response and relapse rates; however, treatment with olanzapine was found to have significantly greater sustained remission rates than treatment with other antipsychotics. In the inpatient setting, where patients tend to be more severe and difficult to manage, olanzapine treatment may lead to higher sustained remission rates than other antipsychotics.
Keywords: inpatients, Japan, outpatients, prospective studies
Introduction
Major treatment guidelines from Japan and across the globe recommend antipsychotics as the primary pharmacological treatment for schizophrenia.1–3 These medications have been broadly grouped into typical or atypical antipsychotics.4 The newer atypical antipsychotics have largely replaced older typical antipsychotics both in Japan5,6 and abroad.7 Although atypical antipsychotics are often grouped together, a growing body of literature has found some consistent differences in efficacy and tolerability suggesting that atypicals represent a heterogeneous group of medications.4,8–10 Recent reviews and meta-analyses of randomized controlled trials have reported greater efficacy with clozapine as well as olanzapine, while these two agents were also associated with a greater risk of weight gain and changes in metabolic parameters.4,8–12
Evaluating clinically relevant outcomes such as treatment response, remission, and relapse is crucial for optimizing the management of patients with schizophrenia in usual clinical care.13 Multiple definitions of treatment response,14–16 remission,17–19 and relapse14,20 have been used, and some consensus has emerged.17 Across all definitions, treatment response refers to a meaningful reduction in symptoms;14,16 remission refers to a sustained period of time when symptoms remain below a threshold of mild impairment;21 and relapse refers to a meaningful exacerbation of symptoms following symptomatic response or remission.14,19 Some studies of remission in schizophrenia have not included the duration criteria, and these studies have tended to find higher rates of remission than those that require sustained remission.21
Outside of Japan, large-scale observational studies have begun to quantify these clinically relevant outcomes in usual clinical care. Two of the largest observational studies in schizophrenia were the pan-European Schizophrenia Outpatient Health Outcomes study (EU-SOHO), conducted in ten European counties,19,22–24 and the Intercontinental Schizophrenia Outpatient Health Outcomes study (IC-SOHO), conducted in 27 counties across Africa, the Middle East, Latin America, Central and Eastern Europe, and Asia.14,25 The 12-month response rates for different antipsychotics in the EU-SOHO study ranged from 45% to 64% with olanzapine (64%) having significantly higher response rates than amisulpride (45%), quetiapine (46%), oral typicals (47%), and depot typicals (48%), but not risperidone (55%) or clozapine (64%).23 Similarly, in IC-SOHO, the response rates at the 12-month visit varied by antipsychotic with significantly higher response rates for olanzapine (74%) than risperidone (64%), quetiapine (48%), and haloperidol (41%).14 In the IC-SOHO study, the relapse rates following response were 12% for olanzapine, 14% for risperidone, 18% for quetiapine, and 20% for haloperidol.25 Over the full 36-months of the EU-SOHO study, 65% of the patients met the sustained remission criteria and treatment with olanzapine was a significant predictor of sustained remission.19 When the EU-SOHO and IC-SOHO studies were combined into the Worldwide SOHO study, the overall sustained remission rate (66%) regardless of treatment over 36 months varied substantially by geographic region.26 Little information exists regarding the rates of response, remission, and relapse for individuals with schizophrenia treated in usual clinical care in Japan.
The objective of this secondary analysis of a 1-year observational study was to examine the response, relapse, and remission rates for patients treated with olanzapine monotherapy (OLZ) or other antipsychotic monotherapy (OAN) in usual care in Japan. When outcomes differed by treatment, an exploratory analysis examined baseline predictors of the outcome and whether the baseline predictors varied by OLZ or OAN.
Methods
Participants
All participants enrolled in this study were diagnosed with chronic schizophrenia based on the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR)27 criteria and were experiencing an acute exacerbation that warranted switching or starting antipsychotic monotherapy per the treating physician’s discretion. A total of 86 study sites, including both inpatient and outpatient settings, were selected to be representative of usual clinical care in Japan. For this noninterventional study, Institutional Review Board approval was obtained based on the requirements at each site and all patients or their representatives gave informed consent.
Procedures
In this prospective, noninterventional, observational study, all treatment decisions, including the choice of antipsychotic, were left to the discretion of the treating physician. Assessments were made at baseline (within 2 weeks of initiating antipsychotic monotherapy), then again in 2 weeks, 1 month, 3 months, 6 months, and 12 months. Special research visits were not required in the protocol; information was collected at regularly scheduled office visits. All patients were at least 20 years of age, experiencing a first acute episode or an acute exacerbation of schizophrenia within 1 month of study initiation, and had a Clinical Global Impression – Severity (CGI-S) score of at least 4 (moderately ill). Patients were excluded if they were considered to be treatment resistant, were currently receiving clozapine, were being treated with long-acting injectable antipsychotics, were pregnant, or had an acute, serious, or unstable medical condition. This analysis was restricted to individuals initiating treatment with antipsychotic monotherapy. If a patient discontinued the initial antipsychotic treatment, data were no longer collected for that patient. Based on their initial treatments, patients were grouped into either OLZ or OAN. In addition, the outcomes for the OLZ group were contrasted with those treated with other atypical antipsychotic monotherapy (OAT).
Measures
Severity of illness was measured by the CGI-S, a seven-point rating of the patient’s severity of mental illness during the previous week, where 1= normal, not at all ill; 2= borderline mentally ill; 3= mildly ill; 4= moderately ill; 5= markedly ill; 6= severely ill; and 7= extremely ill. In this sample, which was restricted to patients with a baseline CGI-S score of at least 4, response was defined as a two-point improvement in the CGI-S rating from baseline for at least one of the post-baseline visits.23 For the subset of patients who met the criteria for response, relapse was defined as an increase in the overall CGI-S score by at least two points from the lowest (best) overall score recorded at previous visits.14,25 Remission was defined as achieving a score of 3 (mildly ill) or less on the CGI-S. Sustained remission was defined as meeting the remission severity criteria and maintaining this score for at least 6 months.28 The Clinical Global Impressions – Parkinsonism is a physician rating of extrapyramidal symptoms that ranges from 0= not present to 8= extremely severe.
Several categorical variables were coded at baseline that could potentially predict later outcomes. A first episode patient code was applied for those who entered the study during their first acute episode of schizophrenia rather than with a returning acute exacerbation of symptoms. Treatment setting was coded as inpatient for those who were initially treated in the hospital as an inpatient, and was coded as outpatient for all other patients. Finally, patients who discontinued one antipsychotic and started another at baseline or switched from antipsychotic polypharmacy to antipsychotic monotherapy were considered as antipsychotic switch patients.
Statistical analysis
Due to potential differences between individuals treated with olanzapine and other antipsychotics, propensity scores were calculated using multiple baseline characteristics including age, sex, treatment setting (inpatient or outpatient), first episode patient, and antipsychotic switch patient. Treatment-group differences in the overall proportion of patients achieving response, relapse, and sustained remission during the study were analyzed using logistic regression while controlling for the propensity scores. Visit-wise rates of response and remission were analyzed using repeated measures logistic regressions that were estimated with generalized estimating equations29 while adjusting for the propensity score. Each model initially compared outcomes for OLZ and OAN and then this was repeated to compare OLZ and OAT using a two-tailed alpha level of 0.05.
An exploratory backward stepwise (P<0.1) logistic regression was conducted to identify baseline predictors of sustained remission for the combined treatment groups and baseline predictors that varied between the treatment groups. The candidate variables for this model were age, sex, treatment setting, first episode patient, and antipsychotic switch patient. The odds ratio (OR) and 95% confidence interval (95% CI) for each identified predictor was estimated, and if the interaction between the baseline predictor and the treatment contrast was significant, then the OR was estimated for each treatment group separately. All analyses were completed using SAS version 9.13 (SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics
At baseline, 578 patients were treated with OLZ and 511 patients were treated with OAN. The majority of the OAN patients (95.3%) were treated with OAT. The number of patients treated with each atypical antipsychotic and average daily doses were olanzapine: n=578; 14.0 mg; risperidone: n=160; 4.6 mg; aripiprazole: n=154; 19.1 mg; blonanserin: n=67; 13.5 mg; quetiapine: n=44; 270.7 mg; paliperidone: n=40; 9.3 mg; perospirone: n=16; 17.3 mg; and zotepine: n=6; 291.7 mg. For typical antipsychotics, the number of patients and doses were haloperidol: n=13; 10.5 mg; bromperidol: n=4; 7.8 mg; sulpiride: n=3; 133.3 mg; chlorpromazine: n=2; 75.0 mg; levomepromazine: n=1; 16.5 mg; and fluphenazine: n=1; 2.0 mg. Chlorpromazine equivalent doses30 were 560.7±257.0 mg/day for the OLZ cohort, 424.0±285.7 mg/day for the OAN cohort, and 426.8±261.0 mg/day for OAT sub-cohort. The 12-month study completion rates were 46.4% for OLZ, 40.5% for OAN, and 40.2% for OAT. Table 1 summarizes baseline characteristics for the three groups of patients. Relative to OAN and OAT, physicians were significantly more likely to choose OLZ for patients who did not have diabetes mellitus, who had lower body mass indices, and higher CGI-S scores.
Treatment response
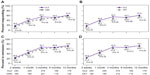
Across the full study period, there was no significant difference in the odds of response between the OLZ (54.4%) and OAN (46.4%) groups (OR [95% CI] =1.29 [0.97–1.72], P=0.08) or between the OLZ (54.4%) and OAT (47.3%) groups (OR [95% CI] =1.26 [0.94–1.69], P=0.12). In the repeated measures logistic regression, the percentage of patients responding was descriptively higher for the OLZ group at each visit (Figure 1) and there was a statistically significant difference in response at the 3-month visit between OLZ and OAN (P=0.048); however, there were no statistically significant differences at any other visit.
Relapse
Among the subset of patients who responded to treatment, there was no significant difference in the odds of relapse between the OLZ (11.7%, 21/179) and OAN (12.8%, 16/125) groups (OR [95% CI] =0.78 [0.38–1.61], P=0.50) or between the OLZ (11.7%, 21/179) and OAT (13.0%, 16/123) groups (OR [95% CI] =0.77 [0.37–1.58], P=0.48).
Remission
The OLZ group was significantly more likely to meet the definition of sustained treatment remission (19.0%) than both the OAN group (13.7%, OR [95% CI] =1.45 [1.03–2.04], P=0.032) and the OAT group (14.0%; OR [95% CI] =1.43 [1.02–2.01], P=0.041). When examining the rates of remission (without the 6-month duration requirement for sustained remission) at each study visit, the OLZ group had descriptively higher rates of remission at each visit; however, none of the visit-wise comparisons were statistically significant (Figure 1).
Because there was a significant difference in sustained treatment remission between the OLZ and OAN groups, an exploratory backward stepwise logistic regression was conducted to identify baseline characteristics and treatment interactions with the baseline characteristics that predicted greater sustained remission rates (Table 2). Regardless of treatment group, higher rates of sustained remission were found for antipsychotic switch patients at baseline (19.8% versus 14.5%, P=0.009) and for first episode patients (20.5% versus 15.7%, P=0.068). In addition, there was a main effect for treatment (P=0.008), treatment setting (P<0.001), and a treatment-by-treatment setting interaction (P=0.006). For outpatients, a similar percentage of patients achieved sustained remission for both treatments (OLZ: 22.2%, OAN: 22.8%), whereas for inpatients, significantly more OLZ than OAN patients achieved sustained remission (OLZ: 17.1%, OAN: 6.6%, OR [95% CI] =3.54 [2.00–6.25]).
Discussion
This analysis of usual clinical care in Japan estimated the 12-month rates of response, relapse, and sustained remission for patients with schizophrenia who were treated with antipsychotic monotherapy. About half of the patients responded to treatment (46.4%–54.4%), and among the responders, only a few patients subsequently relapsed (11.7%–13.0%). Although many patients met the criteria for symptomatic remission at the 12-month visit (69.2%–74.1%), fewer met the 6-month criteria for sustained remission (13.7%–19.0%) during the study. Treatment with OLZ was associated with significantly greater rates of sustained remission than OAN (P=0.032) and OAT (P=0.041), particularly for patients treated in an inpatient setting. Although the results of this secondary analysis were not statistically significant for response and relapse, the numerical advantage for olanzapine relative to other typical and atypical antipsychotics were similar to those reported in the EU-SOHO and IC-SOHO studies.14,23
The Worldwide SOHO (combined EU-SOHO and IC-SOHO) study, which included 17,384 patients with schizophrenia, reported an overall sustained symptom remission rate of 66.1% over 3 years, with higher rates in East Asia (84.4%), Latin America (79.4%), and North Africa/Middle East (79.6%) than in European counties (60.1%–65.1%).26 In the current study, the remission rates at 1 year (74.1% for OLZ and 69.2% for OAN) were similar; however, the 6-month sustained remission rates (19.0% for OLZ and 13.7% for OAN) were much lower, possibly due to the inclusion of a large number of inpatients in the sample; the shorter 1-year follow-up leading to lower rates of 6-month sustained remission relative to a 3-year follow-up period;19,21,23 the CGI-S ≥4 inclusion criteria;21,26 or some other regional difference in patient characteristics or treatment practices between the studies. The EU-SOHO and IC-SOHO findings, which indicate that patients treated with olanzapine tend to have somewhat higher treatment response rates14,23 and lower relapse rates,14,19 are descriptively consistent with the findings in the current study. The lack of statistical significance in the current study may be due to differences in study design, particularly the lower statistical power due to a smaller sample size, the shorter follow-up period, the restriction to only moderately ill patients, or the inclusion of inpatients.
In this study, there was a significant interaction between choice of antipsychotic (olanzapine versus other antipsychotics) and treatment setting (inpatient versus outpatient) in predicting sustained remission. For inpatients, olanzapine treatment led to higher sustained remission rates than other antipsychotic treatments. The difference in sustained remission rates was similar for olanzapine and other antipsychotics in the outpatient setting. This finding is consistent with a randomized trial of newly admitted inpatients with schizophrenia in Japan which, based on time to treatment discontinuation, found that olanzapine was significantly more effective than quetiapine or aripiprazole and that olanzapine-treated patients had significantly greater symptom reduction as measured by the Clinical Global Impression – Change scores than aripiprazole-treated patients.11 Generally, inpatients are more severely ill and difficult to treat, and among these patients, treatment with olanzapine appears to lead to improved sustained remission rates.
Improving remission rates in schizophrenia has important implications. Achieving symptomatic remission has been associated with significantly reduced total treatment costs, medication costs, and emergency department costs.31 Higher rates of remission not only benefit the patients, but also may benefit the health care system by reducing overall treatment costs for patients with schizophrenia.
Limitations
Although some meaningful differences between treatments were observed in this analysis, several important limitations need to be considered when interpreting the study findings. Because this was an observational study, the medication treatment groups were not formed by randomization and differed at baseline, creating the potential for confounding and biased comparisons. Analyses were adjusted for the propensity score based on a select set of baseline covariates; however, the potential for bias due to unmeasured confounders or other baseline differences remains. To ensure the study reflected real-life clinical practice, choice of antipsychotics and the dose prescribed was at the discretion of the psychiatrist, although the study protocol stated that the oral antipsychotics should be prescribed within the approved dosage and administration in Japan. As a result, the average chlorpromazine-equivalent dose in the OLZ group was higher than in either the OAN or OAT groups. In this secondary analysis, the sample size may have been insufficient to detect difference in response, relapse, and remission. In addition, the 1-year observation period may be too short to allow for a sufficient number of relapses or sustained remissions to detect differences, and future research could be conducted to evaluate the impact of a longer follow-up period. The study did not adjust for the number of statistical comparisons so the overall type I error rate may have been greater than 0.05. Remission in schizophrenia is not synonymous with functional recovery, and patients may still have meaningful functional deficits.
Conclusion
In usual care in Japan, treating the acute symptoms of schizophrenia with olanzapine was not found to be significantly different for response and relapse rates; however, treatment with olanzapine was found to have significantly greater sustained remission rates than treatment with other antipsychotics. In the inpatient setting, where patients tend to be more severe and difficult to manage, olanzapine treatment appeared to lead to higher sustained remission rates than other commonly used antipsychotics.
Acknowledgment
Technical writing support was provided by Michael D Stensland of Agile Outcomes Research, Inc., Rochester, MN, USA and Susan Dennett of Strategic Health Outcomes, Inc., Carmel, IN, USA.
Author contributions
MT, NN, SF, and MI were involved with the study design, data collection, data analysis, or preparation and critical review of the manuscript. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work. All authors worked to ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
Eli Lilly Japan KK provided funding for this work. SF is an employee of Eli Lilly Japan KK. MT and NN were employees of Eli Lilly Japan KK in 2013 while this research and manuscript were under development. MI has received honoraria from Eli Lilly Japan KK.
References
Falkai P, Wobrock T, Lieberman J, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, Part 1: acute treatment of schizophrenia. World J Biol Psychiatry. 2005;6(3):132–191. | |
Lehman AF, Lieberman JA, Dixon LB, et al. Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry. 2004;161 (2 Suppl):1–56. | |
Japanese Psychopharmacology Algorithm Project. Acute Psychotic Episode. Tokyo: Igaku-Shoin Ltd; 2006. | |
Leucht S, Kissling W, Davis JM. Second-generation antipsychotics for schizophrenia: can we resolve the conflict? Psychol Med. 2009;39(10):1591–1602. | |
Yoshi T, Uno J, Nakagawa M, et al. Survey of the prescription for psychotherapy in Japanese inpatients with schizophrenia in 2006. Jpn J Clin Psychopharmacol. 2010;13(8):1535–1545. | |
Yoshimura R, Okamoto T, Nakamura J, et al. Prescription pattern of antipsychotic drugs for schizophrenic inpatients in Japan: research on East Asia Psychotropic Prescription Pattern-Antipsychotics study. Psychiatry Clin Neurosci. 2006;60(6):778–779. | |
Bitter I, Treuer T, Dyachkova Y, Martenyi F, McBride M, Ungvari GS. Antipsychotic prescription patterns in outpatient settings: 24-month results from the Intercontinental Schizophrenia Outpatient Health Outcomes (IC-SOHO) study. Eur Neuropsychopharmacol. 2008;18(3):170–180. | |
Leucht S, Komossa K, Rummel-Kluge C, et al. A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry. 2009;166(2):152–163. | |
Boter H, Peuskens J, Libiger J, et al. Effectiveness of antipsychotics in first-episode schizophrenia and schizophreniform disorder on response and remission: an open randomized clinical trial (EUFEST). Schizophr Res. 2009;115(2–3):97–103. | |
Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–1223. | |
Hatta K, Sato K, Hamakawa H, et al. Effectiveness of second-generation antipsychotics with acute-phase schizophrenia. Schizophr Res. 2009;113(1):49–55. | |
Attard A, Taylor DM. Comparative effectiveness of atypical antipsychotics in schizophrenia: what have real-world trials taught us? CNS Drugs. 2012;26(6):491–508. | |
Correll CU, Kishimoto T, Nielsen J, Kane JM. Quantifying clinical relevance in the treatment of schizophrenia. Clin Ther. 2011;33(12):B16–B39. | |
Dossenbach M, Arango-Dávila C, Silva Ibarra H, et al. Response and relapse in patients with schizophrenia treated with olanzapine, risperidone, quetiapine, or haloperidol: 12-month follow-up of the Intercontinental Schizophrenia Outpatient Health Outcomes (IC-SOHO) study. J Clin Psychiatry. 2005;66(8):1021–1030. | |
Gaebel W. Prediction of response to acute neuroleptic treatment in schizophrenia. Int Clin Psychopharmacol. 1996;11 Suppl 2:47–54. | |
Kinon BJ, Chen L, Ascher-Svanum H, et al. Predicting response to atypical antipsychotics based on early response in the treatment of schizophrenia. Schizophr Res. 2008;102(1–3):230–240. | |
Andreasen NC, Carpenter WT Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162(3):441–449. | |
Lambert M, Schimmelmann BG, Naber D, et al. Prediction of remission as a combination of symptomatic and functional remission and adequate subjective well-being in 2960 patients with schizophrenia. J Clin Psychiatry. 2006;67(11):1690–1697. | |
Haro JM, Novick D, Suarez D, et al. Remission and relapse in the outpatient care of schizophrenia: three-year results from the Schizophrenia Outpatient Health Outcomes study. J Clin Psychopharmacol. 2006; 26(6):571–578. | |
Almond S, Knapp M, Francois C, Toumi M, Brugha T. Relapse in schizophrenia: costs, clinical outcomes and quality of life. Br J Psychiatry. 2004;184:346–351. | |
Lambert M, Karow A, Leucht S, Schimmelmann BG, Naber D. Remission in schizophrenia: validity, frequency, predictors, and patients’ perspective 5 years later. Dialogues Clin Neurosci. 2010;12(3):393–407. | |
Haro JM, Edgell ET, Jones PB, et al. The European Schizophrenia Outpatient Health Outcomes (SOHO) study: rationale, methods and recruitment. Acta Psychiatr Scand. 2003;107(3):222–232. | |
Novick D, Ascher-Svanum H, Haro JM, Bertsch J, Takahashi M. Schizophrenia Outpatient Health Outcomes study: twelve-month findings. Pragmatic and Observational Research. 2012;3:27–40. | |
Suarez D, Haro JM. Overview of the findings from the European SOHO study. Expert Rev Neurother. 2008;8(6):873–880. | |
Dossenbach M, Pecenak J, Szulc A, et al. Long-term antipsychotic monotherapy for schizophrenia: disease burden and comparative outcomes for patients treated with olanzapine, quetiapine, risperidone, or haloperidol monotherapy in a pan-continental observational study. J Clin Psychiatry. 2008;69(12):1901–1915. | |
Haro JM, Novick D, Bertsch J, Karagianis J, Dossenbach M, Jones PB. Cross-national clinical and functional remission rates: Worldwide Schizophrenia Outpatient Health Outcomes (W-SOHO) study. Br J Psychiatry. 2011;199(3):194–201. | |
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). Washington, DC: American Psychiatric Publishing, Inc.; 2000. | |
Haro JM, Ochoa S, Gervin M, Mavreas V, Jones P. Assessment of remission in schizophrenia with the CGI and CGI-SCH scales. Acta Psychiatr Scand. 2007;115(2):163–164. | |
Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. | |
Inagaki A, Inada T. [Dose equivalence of psychotropic drugs. Part 18: Dose equivalence of psychotropic drugs: 2006-version.] Jpn J Clin Psychopharmacol. 2006;9:1443–1447. Japanese. | |
Haynes VS, Zhu B, Stauffer VL, et al. Long-term healthcare costs and functional outcomes associated with lack of remission in schizophrenia: a post-hoc analysis of a prospective observational study. BMC Psychiatry. 2012;12:222. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.