Back to Journals » International Journal of General Medicine » Volume 15
Reliability of Hounsfield Unit for Assessing Asymmetrical Vertebral Bone Mass in Adult Degenerative Scoliosis
Authors Jin LY, Su XJ, Xu S, Liu HY , Li XF
Received 30 March 2022
Accepted for publication 17 June 2022
Published 30 June 2022 Volume 2022:15 Pages 5869—5877
DOI https://doi.org/10.2147/IJGM.S368718
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Lin-Yu Jin,1,2,* Xin-Jin Su,3,* Shuai Xu,1 Hai-Ying Liu,1 Xin-Feng Li2
1Department of Spinal Surgery, Peking University People’s Hospital, Peking University, Beijing, People’s Republic of China; 2Department of Orthopedics, Shanghai Key Laboratory for Prevention and Treatment of Bone and Joint Diseases, Shanghai Institute of Traumatology and Orthopedics, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People’s Republic of China; 3Department of Spinal Surgery, Renji Hospital, School of Medicine, Shanghai Jiaotong University, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xin-Feng Li, Department of Orthopedics, Shanghai Key Laboratory for Prevention and Treatment of Bone and Joint Diseases, Shanghai Institute of Traumatology and Orthopedics, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, 200025, People’s Republic of China, Email [email protected] Hai-Ying Liu, Department of Spinal Surgery, Peking University People’s Hospital, Peking University, No. 11, South Xizhimen Street, Beijing, 100044, People’s Republic of China, Email [email protected]
Objective: Hounsfield Unit (HU) has been used to investigate the asymmetrical vertebral bone mass in patients associated with adult degenerative scoliosis (ADS). Therefore, there is an inevitable need to evaluate the performance of HU values in ADS subjects.
Methods: A total of 162 patients (81 ADS patients and 81 non-ADS patients) aged ≥ 50 years undergoing the CT examination were reviewed. The HU values of the lumbar vertebral body (including total, convex side, and concave side) at bilateral pedicle plane were obtained and compared. The paired t-test, chi-squared test, independent samples t-test, and interclass correlation coefficient (ICC) were used for statistical analyses.
Results: The HU values were significantly different between the convex and concave sides of the lumbar vertebral body (P < 0.01). The total prevalence of osteoporosis (OP) in ADS patients was higher than that of non-ADS patients. The prevalence of OP in female or male of ADS patients was higher than that of non-ADS patients, respectively. Intra- and inter-rater reliability were very strong (both > 0.8) for measuring asymmetrical vertebral bone mass in ADS patients.
Conclusion: HU value was a high reproducibility method for evaluating the vertebral bone mass in ADS patients. The HU values at the concave sides were significantly higher than that of convex sides at the lumbar vertebral body on the pedicle plane. The prevalence of OP in ADS patients was higher than that of non-ADS patients, especially for females associated with ADS. Moreover, the static asymmetric load did not enhance the bone mass at the concave side compared with the left/right side of non-ADS patients.
Keywords: adult degenerative scoliosis, bone mass, Hounsfield units, reliability
Introduction
Adult degenerative scoliosis (ADS) was believed to be a predominant spinal disorder disease in recent years.1 It may cause low back pain or disability in elderly patients. Hospital admissions for ADS have increased in recent years with the aging population. Osteoporosis (OP) was a common degenerative condition in aging people,2 and the prevalence of OP was higher in ADS patients compared with other patients.3 Given that a part of ADS patients may need fixation surgery, OP conditions in ADS patients should be taken into consideration by the surgeon before surgery. ADS itself produces asymmetrical mechanics on the convex and concave sides of the spine, which can aggravate the procedure of ADS. Accumulating evidence has shown that sustained biomechanical imbalance of scoliosis may contribute to asymmetric remolding of vertebral microstructure.4,5 However, much of our understanding of asymmetric loading-induced bone remodeling comes from data collected on adolescent idiopathic scoliosis patients (AIS),5 and microstructural changes and remolding of AIS vertebral body between concave and convex sides have been demonstrated by several studies.6,7 Whether there was an ultrastructural difference between the concave and convex side in the vertebral body of ADS spine has not been well elucidated until now.
The gold standard method for determining osteoporosis was the dual-energy x-ray (DXA) absorptiometry.2 Yet, degenerative lumbar conditions often lead to falsely increasing scores of DXA measurements of lumbar bone mineral density (BMD).8 Moreover, the bone microstructure of the vertebral body cannot be precisely evaluated by DXA.9 As an alternate measurement to DXA, the Hounsfield units (HU) value, measuring CT attenuation of tissue, has been proposed to evaluate the BMD in recent years.10–12 The HU measurement can avoid degenerative conditions and cortical bone in 3-dimensional CT images. Surgeons can manually set the region of interest (ROI) to measure the HU value of vertebral trabecular bone, which is more sensitive to detecting the bone mass of the vertebral body than DXA method. Therefore, the HU value may be a useful tool to evaluate the bone mass difference between the concave and convex side of the vertebral body of ADS spine. In recent years, Wang et al found that HU measurement was valuable for evaluating the asymmetrical vertebral bone mass.13 However, no studies have so far addressed the issue of the reliability of HU values on bone mass associated with ADS. Hence, the aim of this study was to evaluate the performance of HU value on the vertebral bone mass and characterize the bone mass features of lumbar vertebrae in ADS patients by comparing with non-ADS patients. The results we got here prove that HU value was a valuable and reliable tool to evaluate the bone quality of vertebral body. Special attention should be taken by the surgeon when facing the elderly ADS patients.
Materials and Methods
Patient Cohort
After IRB approval (2021PHB238), we retrospectively reviewed all patients aged 50 years or older in our hospital from June 2015 to June 2020, and finally include 81 ADS and 81 pared-non-ADS patients according to the inclusion and exclusion criteria. The inclusion criteria were as follows: (1) patients aged 50 years and older; for ADS patients (2) with diagnosis of ADS based on physical examination and whole spinal radiography (Cobb angle ≥10°);14,15 (3) the upper end vertebrae (the vertebrae with the greatest inclination at the rostral side of spine) should be upon the L1 vertebrae; for non-ADS patients (4) with diagnosis of lumbar spinal stenosis or lumbar disc herniation based on CT or MR examinations without lumbar scoliosis (Cobb angle <10°). (5) all included patients underwent three-dimension CT scanning at hospital. While, exclusion criteria were (1) patients with spinal spondylolysis, tuberculosis, tumor, trauma, and skeletal hyperostosis; (2) patients with history of lumbar spinal surgery; (3) patients with metabolic bone disease or taking medications such as chronic glucocorticoids; (4) patients without lumbar CT in our hospital. The informed consents were obtained from all included patients.
HU Value
All included patients underwent three-dimension reconstructive CT (GE discovery, a tube voltage of 120kV). The parameters of CT had a slice thickness of 1.25 mm with 0.625 mm intervals. The coronal and sagittal planes were acquired from the 3D reconstruction of lumbar CT. The supine position was adopted by patients, and lumbar spine should be ensured in a neutral position. Picture archiving and communication systems was used to get the HU value with the method shown in Figure 1: an oval ROI of 400 mm2 was placed at an axial image on the pedicle plane; two oval ROI of 75 mm2 were respectively positioned at the bilateral regions of vertebral body also on the pedicle plane. The ROI should focus on trabecular bone as possible and avoid cortical bone, hemangiomas, and dense bone islands. As shown in Figure 2, a 59 years old male patient was diagnosed as ADS, the HU values were obtained from CT images, and we found that the HU values on the concave side was higher than that of convex side. Measurements were performed by one independent observer, and mean values were calculated. The HU value of L1 vertebral body ≤110HU with specificity (90%) was used to determine the osteoporosis.10,11,16,17
After training of ROI drawing, two observers (observer 1: with 10 years of experience in degenerative spinal surgery, and observer 2: with 6 years of experience in spinal surgery) independently measured the data of HU value of L1-L5 in each patient. The measurement results of these two observers were used to assess the inter-rater reliability, and the measurement was repeated by the first observer with a washout period of at least 2 weeks, in order to assess the intra-rater reliability. The information of patients was blinded to each other’s results.
Statistical Analysis
All numeric results were recorded as mean ± SD. The HU values in non-ADS patients were presented as mean ± SD, and the HU values on the left and right sides of lumbar vertebral body in non-ADS patients were compared with paired t-test. The chi-squared test was used to compare the prevalence between ADS and non-ADS patients. The HU values on the convex and concave sides of lumbar vertebral body in ADS patients and those on left and right sides in non-ADS patients were compared with two independent samples t-test. The HU values were compared among different lumbar vertebral bodies in ADS patients with one-way analysis of variance. The intra-rater and inter-rater reliability of the HU values was evaluated by the two-way intraclass correlation coefficient (ICC). The ICC values were 0–1.00, and values closer to 1.00 represent better reliability. They were defined as very weak (0.01 to 0.19), weak (0.20–0.39), moderate (0.40–0.59), strong (0.60–0.79) or very strong (≥0.080).18 Moreover, the 95% confidence intervals of the ICC were calculated along with Cronbach’s α. Statistical analysis was conducted using SPSS for Windows (version 24.0, Statistical Product and service Solutions, Chicago, IL). P value <0.05 was considered statistically significant.
Results
A total of 162 patients were included in the final analysis. The basic information of ADS and non-ADS patients is summarized in Table 1. There were no significant differences in the terms of age, height, weight, and BMI, between ADS patients and non-ADS patients (p > 0.05). The mean HU values of each vertebrae in ADS patients are lower than that of non-ADS patients, but there is no statistically significant difference between them. Strong to very strong reliability was obtained during the measurements of all the HU values. Both inter-rater and intra-rater ICCs were larger than 0.80, and all the ICC values, 95% CI, and Cronbach’s α are shown in Tables 2 and 3. The strong reliability of HU values suggests a reliable indicator for evaluating the bone mass of vertebrae in ADS patients.
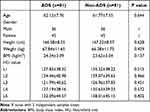 |
Table 1 Basic Information of ADS and Non-ADS Patients |
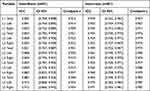 |
Table 2 Inter- and Intra-Rater Reliability (Intra-Class Correlation Coefficients, ICC) with 95% Confidence Interval (CI) and Cronbach’s Alpha of the HU Values Gained from Non-ADS Patients |
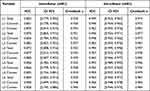 |
Table 3 Inter- and Intra-Rater Reliability (Intra-Class Correlation Coefficients, ICC) with 95% Confidence Interval (CI) and Cronbach’s Alpha of the HU Values Gained from ADS Patients |
The gender-related distribution of osteoporosis diagnosed based on HU value was shown in Table 4. The total prevalence of osteoporosis (OP) in ADS patients was higher than that of non-ADS patients. There is no statistically difference regarding the prevalence of OP in female or male of ADS patients.
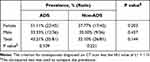 |
Table 4 Gender-Related Distribution of Osteoporosis Diagnosed on HU Values in ADS and Non-ADS Patients |
As shown in Table 5, the total HU values on the convex side (L1-4) were significantly lower than that on the concave side (p < 0.05). The HU values on the convex side of each vertebral body were significantly lower than those on the concave side in ADS patients (all p < 0.05). While, there were no differences of HU values between the left and right side of each vertebral body in non-ADS patients (p > 0.05). In addition, there were no significant differences in HU values between the concave side in ADS patients and the left/right side in non-ADS patients.
 |
Table 5 HU Values in Different Side of Each Vertebral Body |
Discussion
In this study, we performed an in vivo bone mass investigation of ADS. Intra-rater and inter-rater analysis showed that HU methods might be a useful tool to evaluate the vertebral body mass in elder patients according to the strong reliability. The female objectives have a higher prevalence of OP than males in ADS patients and non-ADS patients, and the prevalence of OP in ADS patients was higher than that of non-ADS patients. We here also reported a significant difference in HU values between the convex and concave sides of the lumbar vertebral body on the pedicle plane, which suggests that asymmetrical loading might lead to irregular cancellous bone remodeling of the vertebral body.
The Hounsfield unit value is a relative quantitative measurement of radio density based on the CT images.19 HU value has been used to evaluate the bone mineral density in recent studies due to obtaining easily from CT images without added cost or radiation.12 Therefore, many studies have recommended the use of Hounsfield unit (HU) measurements in computed tomography (CT) images to assess BMD, and a positive correlation between HU value and DXA value was also confirmed.3,10,12,13,20 In addition, several advantages of HU measurements have been proposed, such as avoiding areas with obvious degenerative conditions and removing the interferences of cortical bone when compared with the DXA method. To the best of our knowledge, this study was the first time to assess the reliability of HU value on the vertebral bone mass associated with ADS. In this study, we obtained the HU values of the L1-L5 vertebral body from ADS patients and pared-non-ADS patients. All the results of ICC were larger than 0.8, both in the dimensions of intra-class and inter-class. The previous study has shown HU measurement has excellent inter-and intra-rater reliability in assessing bone quality.21 However, few studies have focused on the asymmetrical vertebral bone mass in ADS patients. The present study, focusing on the asymmetrical bone mass, showed a different bone mass distribution in the same vertebrae of ADS patients. The HU measurement could be used as a reproductivity spinal instrumentation for evaluating the bone quality associated with ADS.
Osteoporosis was a common degenerative condition associated with decreased bone mass and strength, which occurred in the aging population. This pathological condition was the most frequent cause of bone fractures (such as spine, proximal femur, distal forearm fractures) in the elderly.2 The prevalence of OP in the Chinese general aging population ranges from 30% to 40% among females and from 10% to 20% among males.22,23 While in the current study, we found that the prevalence of OP in ADS and non-ADS female patients was 51.11% and 37.77%, respectively, and the prevalence of OP in ADS and non-ADS male patients was 33.33% and 25.00%, respectively. The results of our study were higher than previous studies. Several reasons may explain this different trait. First, the traditional gold standard method for determining OP, DXA, used in previous studies, usually measured the BMD of lumbar vertebral bodies (L1-L4) and hips. However, the degenerative spine conditions may lead to a lower prevalence of OP using the DXA measurements of lumbar BMD.8,11 In recent years, HU value detected by CT has been broadly studied to evaluate the bone mineral density because acquiring the HU values by CT can avoid vertebral degenerative changes and cortical bone and directly focus on the cancellous bone of vertebral body, which was more sensitivity than DXA.10–12 The other reason for the difference may be the lack of physical activity related to spine degenerative diseases. Low back and leg pain, claudication, and neural symptom are common among the ADS and non-ADS patients. These pain conditions may directly lead to decreased physical activity, for that the lack of physical activity was associated with bone mass loss and development of OP. In addition, our study showed that the prevalence of OP in ADS patients was higher than that of non-ADS patients. Zou et al3 reported that the incidence of OP in ADS patients was higher than in patients with other lumbar degenerative conditions. Furthermore, lumbar scoliosis was a useful clinical marker for OP.24 A possible cause of this group difference may be that asymmetric loading in ADS patients may enhance the progression of bone resorption.14
According to the Wolff’s law, it was reported that mechanical loading may influence the bone mass distribution.25 Bones can adjust their micro-structure to ensure that they were strong enough to withstand the load which they were carrying without too much microdamage or fracture.26 This functional adaptation to habitual mechanical load led to bone mass changes through the process of bone remodeling.27 To date, much of the cognizing on mechanics-induced bone remodeling mainly comes from research focused on young and healthy individuals.28 However, little information clarified the process of bone remodeling in aging populations who suffered from the asymmetric load. The remodeling progression of bone was different between young and elderly patients’ micro-architecture, and it has been shown that aging changed the activity of bone mechano-adaptation.29 In the current study, we focused on ADS patients whose spine deformity naturally led to asymmetric loading on the vertebral body. There were significant differences in bone mass between the concave and convex sides of the vertebral body on the pedicel plane. The results of this study supported that the process of bone remodeling occurred in the vertebral body of ADS patients. In our previous finite element analysis study,30 we found that the mechanic load on the concave side was more extensive than that of the convex side in the major curve of the spine. The upper end vertebrae and above suffered from the opposite asymmetric load (the mechanic load at the concave side was larger than that of convex side). Thus, the HU values at the concave side were higher than those of convex side in the major curve vertebrae. Several clinical and experimental studies have confirmed the connection between the mechanical environment and bone structure under sports31 or bed rest conditions.32 Moreover, weight-bearing or gymnastic activities can enhance the bone mineral density in human and animal.33,34 However, our results demonstrated that the static asymmetric load did not enhance the bone mass at the concave side compared with the left/right side of non-ADS patients. Aging-related changes may play an important role in the mechanic-induced process of bone remodeling,29 but the underlying mechanism has yet to be identified in future research.
For spinal surgeons, OP conditions in ADS patients should be placed in a relatively important position. Pedicle screw fixation is the gold standard method to stabilize the spine and get a rigid fixation to correct the deformity.35 Non-rigid fusion after fixation surgery often led to non-fusion of the surgical segments, which in turn resulted in screw loosening. The quality of bone tissue was considered as one of the predictors for the occurrence of screw loosening.36 It was reported that elderly patients had a higher incidence of screw loosening,36 and screw loosening was more common in osteopenia and osteoporotic conditions.37 Seller et al38 reported that bone mineral density was a good predictor for the pullout resistance of pedicle screw. Furthermore, cancellous, not cortical bone, affected the stability and anchorage of pedicle screws.6 Here, we evaluated the local cancellous bone mass of lumbar vertebrae in ADS patients using the HU values and found that bone mass on the concave side of lumbar vertebrae was higher than that of the convex side. In addition, the prevalence of OP in ADS patients was higher than in non-ADS patients. Thus, special attention should be taken by the surgeon when they are facing elderly ADS patients. Although our study did not include the information about the incidence of screw loosening, it would be important to arouse the attention of surgeons to focus on the OP in ADS patients before surgery. It would be interesting to investigate the cut-off HU values of screw augmentation in the future study.
There are several limitations in our study. Firstly, this retrospective study may cause selection bias. Secondly, the number of patients was relatively small in a single center. A further larger sample prospective study may strengthen the reliability of our findings. Thirdly, the present study did not include the correlation between the incidence of screw loosening and asymmetric bone mass of the vertebral body, and it would be interesting to investigate the relationships in future studies.
In conclusion, HU measurement could be a reliable method in assessing the asymmetrical vertebral bone mass in ADS patients. OP was common among ADS patients compared with non-ADS patients. The static asymmetric load did not enhance the bone mass at the concave side compared with the left/right side of non-ADS patients. The HU values at the concave sides were significantly higher than that of convex side at the lumbar vertebral body on the pedicle plane. Surgeons should carefully evaluate the bone quality of ADS patients to avoid screw loosening.
Abbreviations
ADS, adult denigrative scoliosis; OP, osteoporosis; CT, computer tomography; HU, Hounsfield unit; ROI, the region of interest.
IRB Approval Statement
This study was approved by the institutional review board of Peking University people’s hospital (2021PHB238). The informed consents were obtained from all included patients. This study was also conducted in accordance with the Declaration of Helsinki.
Data Sharing Statement
Yes.
Acknowledgments
We thank Dr Cheng-Cheng Liu from the Office of Cancer Screening, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100021, China, for supervising and improving the confidence of statistical analysis. Lin-Yu Jin and Xin-Jin Su are co-first authors for this study.
Funding
This work was supported by grants from the Procurement of Government of National Health Commission of China (No. 2127000218), and the project of Screening for spinal deformity in Chinese adolescents (No. 2159000033).They play no roles in investigation.
Disclosure
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
References
1. Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine. 2005;30(9):1082–1085. doi:10.1097/01.brs.0000160842.43482.cd
2. Hamdy RC, Petak SM, Lenchik L. Which central dual X-ray absorptiometry skeletal sites and regions of interest should be used to determine the diagnosis of osteoporosis? J Clin Densitom. 2002;5(Suppl):S11–S18. doi:10.1385/JCD:5:3S:S11
3. Zou D, Jiang S, Zhou S, et al. Prevalence of osteoporosis in patients undergoing lumbar fusion for lumbar degenerative diseases: a combination of DXA and Hounsfield units. Spine. 2020;45(7):E406–E410. doi:10.1097/BRS.0000000000003284
4. Stokes IA. Mechanical modulation of spinal growth and progression of adolescent scoliosis. Stud Health Technol Inform. 2008;135:75–83.
5. Li XF, Li H, Liu ZD, Dai LY. Low bone mineral status in adolescent idiopathic scoliosis. Eur Spine J. 2008;17(11):1431–1440. doi:10.1007/s00586-008-0757-z
6. Shea KG, Ford T, Bloebaum RD, D’Astous J, King H. A comparison of the microarchitectural bone adaptations of the concave and convex thoracic spinal facets in idiopathic scoliosis. J Bone Joint Surg Am. 2004;86(5):1000–1006. doi:10.2106/00004623-200405000-00017
7. Yu WS, Chan KY, Yu FW, et al. Bone structural and mechanical indices in Adolescent Idiopathic Scoliosis evaluated by high-resolution peripheral quantitative computed tomography (HR-pQCT). Bone. 2014;61:109–115. doi:10.1016/j.bone.2013.12.033
8. Muraki S, Yamamoto S, Ishibashi H, et al. Impact of degenerative spinal diseases on bone mineral density of the lumbar spine in elderly women. Osteoporos Int. 2004;15(9):724–728. doi:10.1007/s00198-004-1600-y
9. Kanis JA, Burlet N, Cooper C, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2008;19(4):399–428. doi:10.1007/s00198-008-0560-z
10. Pickhardt PJ, Pooler BD, Lauder T, Del Rio AM, Bruce RJ, Binkley N. Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med. 2013;158(8):588–595. doi:10.7326/0003-4819-158-8-201304160-00003
11. Zou D, Li W, Deng C, Du G, Xu N. The use of CT Hounsfield unit values to identify the undiagnosed spinal osteoporosis in patients with lumbar degenerative diseases. Eur Spine J. 2019;28(8):1758–1766. doi:10.1007/s00586-018-5776-9
12. Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 2011;93(11):1057–1063. doi:10.2106/JBJS.J.00160
13. Wang H, Zou D, Sun Z, Wang L, Ding W, Li W. Hounsfield unit for assessing vertebral bone quality and asymmetrical vertebral degeneration in degenerative lumbar scoliosis. Spine. 2020;45(22):1559–1566. doi:10.1097/BRS.0000000000003639
14. Aebi M. The adult scoliosis. Eur Spine J. 2005;14(10):925–948. doi:10.1007/s00586-005-1053-9
15. Wong E, Altaf F, Oh LJ, Gray RJ. Adult Degenerative Lumbar Scoliosis. Orthopedics. 2017;40(6):e930–e939. doi:10.3928/01477447-20170606-02
16. Hendrickson NR, Pickhardt PJ, Del Rio AM, Rosas HG, Anderson PA. Bone mineral density T-scores derived from CT attenuation numbers (Hounsfield units): clinical utility and correlation with dual-energy X-ray absorptiometry. Iowa Orthop J. 2018;38:25–31.
17. Lee SJ, Binkley N, Lubner MG, Bruce RJ, Ziemlewicz TJ, Pickhardt PJ. Opportunistic screening for osteoporosis using the sagittal reconstruction from routine abdominal CT for combined assessment of vertebral fractures and density. Osteoporos Int. 2016;27(3):1131–1136. doi:10.1007/s00198-015-3318-4
18. Takatalo J, Ylinen J, Pienimäki T, Häkkinen A. Intra- and inter-rater reliability of thoracic spine mobility and posture assessments in subjects with thoracic spine pain. BMC Musculoskelet Disord. 2020;21(1):529. doi:10.1186/s12891-020-03551-4
19. DenOtter TD, Schubert J. Hounsfield unit. In: StatPearls. Treasure Island (FL): StatPearls PublishingCopyright © 2022, StatPearls Publishing LLC.; 2022.
20. Pickhardt PJ, Lauder T, Pooler BD, et al. Effect of IV contrast on lumbar trabecular attenuation at routine abdominal CT: correlation with DXA and implications for opportunistic osteoporosis screening. Osteoporos Int. 2016;27(1):147–152. doi:10.1007/s00198-015-3224-9
21. Zaidi Q, Danisa OA, Cheng W. Measurement techniques and utility of Hounsfield unit values for assessment of bone quality prior to spinal instrumentation: a review of current literature. Spine. 2019;44(4):E239–E244. doi:10.1097/BRS.0000000000002813
22. Chen P, Li Z, Hu Y. Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health. 2016;16(1):1039. doi:10.1186/s12889-016-3712-7
23. Yu F, Xia W. The epidemiology of osteoporosis, associated fragility fractures, and management gap in China. Arch Osteoporos. 2019;14(1):32. doi:10.1007/s11657-018-0549-y
24. Pappou IP, Girardi FP, Sandhu HS, et al. Discordantly high spinal bone mineral density values in patients with adult lumbar scoliosis. Spine. 2006;31(14):1614–1620. doi:10.1097/01.brs.0000222030.32171.5f
25. Rowe P, Koller A, Sharma S. Physiology, bone remodeling. In: StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2020, StatPearls Publishing LLC.; 2020.
26. Lanyon LE, Armstrong VJ, Saxon L, et al. Estrogen receptors critically regulate bones’ adaptive responses to loading. Clin Rev Bone Miner Metab. 2007;5(4):234–248. doi:10.1007/s12018-008-9011-9
27. Seeman E. Bone modeling and remodeling. Crit Rev Eukaryot Gene Expr. 2009;19(3):219–233. doi:10.1615/CritRevEukarGeneExpr.v19.i3.40
28. Prisby RD, Lafage-Proust MH, Malaval L, Belli A, Vico L. Effects of whole body vibration on the skeleton and other organ systems in man and animal models: what we know and what we need to know. Ageing Res Rev. 2008;7(4):319–329. doi:10.1016/j.arr.2008.07.004
29. Javaheri B, Pitsillides AA. Aging and mechanoadaptive responsiveness of bone. Curr Osteoporos Rep. 2019;17(6):560–569. doi:10.1007/s11914-019-00553-7
30. Song XX, Jin LY, Li XF, et al. Effects of low bone mineral status on biomechanical characteristics in idiopathic scoliotic spinal deformity. World Neurosurg. 2018;110:e321–e329. doi:10.1016/j.wneu.2017.10.177
31. Ducher G, Prouteau S, Courteix D, Benhamou CL. Cortical and trabecular bone at the forearm show different adaptation patterns in response to tennis playing. J Clin Densitom. 2004;7(4):399–405. doi:10.1385/JCD:7:4:399
32. Spector ER, Smith SM, Sibonga JD. Skeletal effects of long-duration head-down bed rest. Aviat Space Environ Med. 2009;80(5 Suppl):A23–A28. doi:10.3357/ASEM.BR02.2009
33. Krølner B, Toft B, Pors Nielsen S, Tøndevold E. Physical exercise as prophylaxis against involutional vertebral bone loss: a controlled trial. Clin Sci. 1983;64(5):541–546. doi:10.1042/cs0640541
34. Bassey EJ, Ramsdale SJ. Increase in femoral bone density in young women following high-impact exercise. Osteoporos Int. 1994;4(2):72–75. doi:10.1007/BF01623226
35. Boos N, Webb JK. Pedicle screw fixation in spinal disorders: a European view. Eur Spine J. 1997;6(1):2–18. doi:10.1007/BF01676569
36. Galbusera F, Volkheimer D, Reitmaier S, Berger-Roscher N, Kienle A, Wilke HJ. Pedicle screw loosening: a clinically relevant complication? Eur Spine J. 2015;24(5):1005–1016. doi:10.1007/s00586-015-3768-6
37. Zindrick MR, Wiltse LL, Widell EH, et al. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop Relat Res. 1986;203(203):99–112.
38. Seller K, Wahl D, Wild A, Krauspe R, Schneider E, Linke B. Pullout strength of anterior spinal instrumentation: a product comparison of seven screws in calf vertebral bodies. Eur Spine J. 2007;16(7):1047–1054. doi:10.1007/s00586-007-0307-0
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


