Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
Reliability and validity of the Thai self-report version of the Yale–Brown Obsessive–Compulsive Scale-Second Edition
Authors Hiranyatheb T, Saipanish R , Lotrakul M, Prasertchai R, Ketkaew W, Jullagate S, Udomsubpayakul U , Kusalaruk P
Received 10 June 2015
Accepted for publication 8 September 2015
Published 28 October 2015 Volume 2015:11 Pages 2817—2824
DOI https://doi.org/10.2147/NDT.S90276
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Wai Kwong Tang
Thanita Hiranyatheb,1 Ratana Saipanish,1 Manote Lotrakul,1 Rungthip Prasertchai,1 Wanwisa Ketkaew,1 Sudawan Jullagate,1 Umaporn Udomsubpayakul,2 Pichaya Kusalaruk1
1Department of Psychiatry, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand; 2Section for Clinical Epidemiology and Biostatistics, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Purpose: The self-report version of the Yale–Brown Obsessive–Compulsive Scale (Y-BOCS) has been developed to overcome the limitations of the clinician-administered version, which needs to be executed by trained personnel and is time consuming. The second edition of the Y-BOCS (Y-BOCS-II) was developed to address some limitations of the original version. However, there is no self-report version of the Y-BOCS-II at the moment. This study aimed to evaluate the psychometric properties of the developed Thai self-report version of the Yale–Brown Obsessive–Compulsive Scale-Second Edition (Y-BOCS-II-SR-T).
Patients and methods: Y-BOCS-II-SR-T was developed from the Thai version of the Yale–Brown Obsessive–Compulsive Scale-Second Edition (Y-BOCS-II-T). The Y-BOCS-II-SR-T, the Y-BOCS-II-T, the Thai version of the Florida Obsessive–Compulsive Inventory (FOCI-T), the Hamilton Rating Scale for Depression (HAM-D), the nine-item Patient Health Questionnaire (PHQ-9), and the Pictorial Thai Quality of Life (PTQL) instrument were administered to 52 obsessive–compulsive disorder (OCD) patients. Internal consistency for the Y-BOCS-II-SR-T was calculated with Cronbach’s alpha coefficient (α), and the factor analyses were completed. Pearson’s correlation was used in determining convergent and divergent validity among the other measures.
Results: The mean score of the Y-BOCS-II-SR-T total score was 20.71±11.16. The internal consistencies of the Y-BOCS-II-SR-T total scores, the obsession subscale, and the compulsion subscale scores were excellent (α=0.94, α=0.90, and α=0.89, respectively). The correlation between each item and the Y-BOCS-II-SR-T total score showed strong correlation for all items. Confirmatory factor analysis with model modification showed adequate fit for obsession and compulsion factor models. The Y-BOCS-II-SR-T had strong correlation with the YBOCS-II-T and the FOCI-T (rs>0.90) and weaker correlation with the HAM-D, PHQ-9, and PTQL (rs<0.60), which implied good convergent and divergent validity.
Conclusion: The Y-BOCS-II-SR-T is a psychometrically sound and valid measure for assessing obsessive–compulsive symptoms.
Keywords: Thai, obsessive–compulsive disorder, Yale–Brown Obsessive–Compulsive Scale, self-report
Introduction
The Yale–Brown Obsessive–Compulsive Scale (Y-BOCS)1,2 is a semi-structured, interview-based rating scale, which has been used widely by clinicians for assessing the severity of obsessive–compulsive disorder (OCD) symptoms.3 It consists of two main components: 1) the Severity Scale, and 2) the Symptom Checklist. Goodman et al1,2 reported good psychometric properties for Y-BOCS. The alpha coefficient (α) was 0.89 for internal consistency, with high inter-rater reliability (r=0.98). Regarding the convergent and discriminant validity, it moderately to strongly correlated with the Clinical Global Impression (CGI) Scale (r=0.74) but had weaker correlation with the Hamilton Rating Scale for Depression (HAM-D) (r=0.60) and the Hamilton Rating Scale for Anxiety (HAM-A) (r=0.47).1,2 Also, further studies in the past have supported the postulation that Y-BOCS has good psychometric properties.3,4
The clinician-interview format of the Y-BOCS is considered to be the ideal method of OCD symptom assessment; however, the usage of time and resources are extensive.5,6 Therefore, several self-report versions of the Y-BOCS have been developed to overcome these problems.5,7 A study by Steketee et al5 showed that the psychometric properties of the Y-BOCS self-report have excellent internal consistency (α=0.89 for nonclinical samples and α=0.78 for OCD patients) and excellent test–retest reliability in non-clinical groups for self-report over a 1-week period (r=0.88 for the total score). The total scores of the Y-BOCS self-report version were strongly correlated with the clinician-interview version in both non-clinical and OCD groups (r=0.75 and r=0.79, respectively).
The Yale–Brown Obsessive–Compulsive Scale-Second Edition (Y-BOCS-II)8 was developed in 2010 to overcome some limitations to the original Y-BOCS. A few important changes were made in the Y-BOCS-II. Firstly, the “resistance against obsessions” item was replaced with the “obsession-free interval”, because the efforts to resist obsessions are often maladaptive and make OCD patients more impaired, while the “obsession-free interval” item is more neutral. Secondly, the scoring was extended from 5 points (scoring range, 0–4) to 6 points (scoring range, 0–5) in order to increase the sensitivity to changes during treatment. Thirdly, the avoidance items were integrated and modified into the scoring of Severity Scale items because of the lack of clarity on rating the ritualistic avoidance of the original Y-BOCS. Lastly, modifications were made in the content and format of the Symptom Checklist for better clarity and easier understandability of the symptoms. The psychometric study of the Y-BOCS-II Severity Scale showed high internal consistency (Cronbach’s alpha [α] =0.89) with high inter-rater reliability (intraclass correlation [ICC] =0.96). The exploratory factor analysis showed two factors with items associated with the obsession and compulsion factors. The Y-BOCS-II Severity Scale was strongly correlated to the CGI, which indicated good convergent validity, and only moderately correlated to depressive symptoms and general worry, as measured by the Inventory of Depressive Symptomatology Self-Report (IDS-SR) and the Penn State Worry Questionnaire (PSWQ), respectively,5,8 which indicated good divergent validity.
However, there has been no development of a self-report version of the Y-BOCS-II and its psychometric properties published elsewhere, even though it is needed. In Thailand, the assessment tool for OCD is the Thai version of the Yale–Brown Obsessive–Compulsive Scale-Second Edition (Y-BOCS-II-T), but there is no self-report measure of Y-BOCS-II-T, which would be very useful for medical personnel in overcrowded clinical settings. Therefore, the Thai self-report version of the Yale–Brown Obsessive–Compulsive Scale-Second Edition (Y-BOCS-II-SR-T) was developed. This study aimed to assess the psychometric properties of the Y-BOCS-II-SR-T as a measure for OCD symptoms and severity.
Methods
Participants
Participants included 52 OCD patients (55.8% male, mean age 37.00 years; standard deviation [SD] =16.52). All patients were diagnosed as OCD (as determined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision [DSM-IV-TR])9 by trained psychiatrists and were confirmed by the positive result on the obsessive–compulsive module in the Mini International Neuropsychiatric Interview (MINI), Thai version.10 All patients were recruited from the outpatient clinic of the Department of Psychiatry, Ramathibodi Hospital, Bangkok, Thailand by referrals from other doctors or by direct invitation from the researchers. To be included in the study, the participants had to have OCD as the primary diagnosis, be >18 year old, and agree to participate in the study. Exclusion criteria were illiteracy, intellectual disability, severe psychosis, or mental disorder due to medical condition or substances, which were determined from patients’ psychiatric histories and clinical observations during the interviews.
Measures
The Y-BOCS-II-SR-T
The Y-BOCS-II-SR-T is a self-report measure in the paper-and-pencil form. It was developed from the Y-BOCS-II-T.11 Ten OCD patients were invited into the pilot group to complete the Y-BOCS-II-SR-T. The items in the Y-BOCS-II-SR-T were in the exact same order as in the Y-BOCS-II-T, although a few words from the Y-BOCS-II-T were slightly modified for easier understanding. Also, we added some explanation of the Y-BOCS-II-SR-T. For example, we added explanations of the terms “obsession” and “compulsion” into the Y-BOCS-II-SR-T Severity Scale. Regarding each item of the Y-BOCS-II-SR-T Severity Scale, we also selected the most explicit question rather than using many questions. For instance, the second item of the Y-BOCS-II-T queried the obsession-free interval by asking:
On average, what is the longest continuous period (or block) of time in which you are free of obsessive thoughts? (Only consider time while awake. You can also ask:) How frequently do the obsessive thoughts occur?
We adjusted it to read, “‘On average, what is the longest continuous period (or block) of time in which you are free of obsessive thoughts?’ (Only consider time while awake).” Another example, on the third item of Y-BOCS-II-T, which asked about the degree of control over obsessive thoughts was phrased as, “How much control do you have over your obsessive thoughts? How successful are you in stopping or ignoring them? Can you dismiss them?”. We shortened the question to: “How much control do you have over your obsessive thoughts?”11
For the Y-BOCS-II-SR-T-Symptom Checklist, we deleted some content that was aimed at the clinician and that contained difficult-to-understand text or medical terms, such as:
Raters must ascertain whether the reported behaviors are bona fide symptoms of OCD, and not symptoms of another disorder such as specific phobia or trichotillomania.
In addition, these instructions, which were contained in the item 7 instructions of the Y-BOCS-II-T, were deleted:
It is not always clear where to draw the line between somatic obsessions and the somatic preoccupations of *hypochondriasis. Factors that point to OCD are the presence of compulsions not limited to seeking reassurance.
The words, “*Distinguish from anorexia nervosa, in which concern is gaining weight” occurred in item 8 of the original Y-BOCS-II-T; they were also deleted. The Y-BOCS-II-SR-T was pretested, adjusted, and tested again, and the Y-BOCS-II-SR-T was finalized when the OCD patients in the pilot group stated that they could understand the content of questions clearly and when all authors agreed that the Y-BOCS-II-SR-T and the Y-BOCS-II-T were matched for content.11
The Y-BOCS-II-T
The Y-BOCS-II-T in a clinician-rated format consists of ten items in the Severity Scale (Y-BOCS-II-T-SS), which assesses time spent on obsessions and compulsion, obsession-free interval, resistance to compulsion, control over obsessions and compulsions, distress associated with obsessions, distress if compulsions are prevented, and interference from obsessions and compulsions, each of them scored from 0–5.8 The Y-BOCS-II-T also includes the 67 items of The Symptom Checklist (Y-BOCS-II-T-SC), which contains items about obsessions (29 items), compulsions (29 items), and avoidance (nine items).12 The internal consistencies for the total scores of the Y-BOCS-II-T-SS and the Y-BOCS-II-T-SC were 0.94 and 0.90, respectively. The inter-rater reliability, which is described elsewhere,11 demonstrated excellent correlation for both the Y-BOCS-II-T-SS and Y-BOCS-II-T-SC (r=0.99). The total score of the Y-BOCS-II-SS correlated well with the Clinical Global Impression-Severity (CGI-S) scale and the Global Assessment of Functioning (GAF), and lower correlations were obtained with the HAM-D scores, which implied good convergent and divergent validity. However, the Y-BOCS-II-T-SC had moderate correlations with the CGI-S, GAF, and HAM-D, which indicated moderate convergent and divergent validity.11
The Thai version of the Florida Obsessive–Compulsive Inventory
The Florida Obsessive–Compulsive Inventory (FOCI) is a self-report questionnaire for assessing OCD symptoms and severity.13 The Thai version of the Florida Obsessive–Compulsive Inventory (FOCI-T), which was translated from the FOCI-English version, consists of two scales: 1) the Symptom Checklist scale, and 2) the Symptom Severity scale. The Symptom Checklist scale was developed from the Symptom Checklist scale of the Y-BOCS. Total score of the Symptom Checklist scale is calculated by summing the presence of all items (range, 0–20). The Symptom Severity scale consists of five items: 1) time occupied, 2) interference, 3) distress, 4) resistance, and 5) degree of control. The patient rates the severity level of existing symptoms in a 0–4 scoring range, which is calculated by summing the five severity items (range, 0–20). The FOCI-T Symptom Severity had excellent internal consistency (α=0.92) and was highly correlated with the total score of the Y-BOCS-II-T and the CGI-S,14 but was fairly correlated with the scales for severity of depression, quality of life, and functioning impairment, which implied an acceptable concurrent validity of the FOCI-T Severity Scale.15
The Pictorial Thai Quality of Life instrument
The PTQL instrument is a self-report measure for assessing the quality of life of patients both in clinical and community settings. It consists of 25 items, which are divided into six domains: 1) physical, 2) cognitive, 3) affective, 4) social function, 5) economic, and 6) self-esteem domains. It was found to be a good instrument for discriminating between quality of life of people with mental disorders and normal people (P≤0.001). It also demonstrated a high level of concurrent validity associated with the World Health Organization Quality of Life instrument-Short Form (WHOQOL-BREF) (r=0.92). The α for the PTQL was good (α=0.88).16
The HAM-D
The HAM-D17 is the most widely used clinician-administered scale for measuring the severity of depression and response to treatment. The Thai version of the HAM-D was shown to have good internal consistency (α=0.74) and its concurrent validity, as compared with the GAF Scale, was also satisfactory (Spearman’s correlation coefficient [rs], −0.82).18 All interviewers had been trained to administrate the Thai version of the HAM-D, and the inter-rater reliability was excellent (r=0.97).11
Patient Health Questionnaire
The nine-item Patient Health Questionnaire (PHQ-9) is a self-report measure; in our current study, it was used for assessing depressive symptoms patients had during the 2 weeks prior to answering the questionnaire. It consists of nine questions based on the DSM-IV-TR criteria for major depressive episodes.19 The Thai version of the PHQ-9 has been shown to yield satisfactory internal consistency (α=0.79) and moderate convergent validity as compared with the HAM-D (r=0.56; P<0.001).20
Procedure
All patients participated voluntarily in the current study. After receiving an explanation about the purpose and method of the study and after giving informed consent, patients were interviewed by one of four interviewers: two psychiatrists and two psychiatric nurses. The interview process included assessing the OCD symptoms by the Y-BOCS-II-T, and depression by the Thai version of the HAM-D. The self-report measures (the Y-BOCS-II-SR-T, FOCI-T, PHQ-9, and the PTQL) were also completed by the participants. In order to test the order effect of clinician-interview and self-report format, half of the OCD participants were interviewed before completing the self-report measures, and the other half of the patients completed the self-assessment before being interviewed.
The current study was approved by the Ethics Committee of the Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
Data analysis
The collected data were analyzed using SPSS version 20.0 software. Descriptive statistics were used to examine the scoring of the Y-BOCS-II-SR-T, FOCI-T, PTQL, HAM-D, and the PHQ-9, which were reported as mean and SD.
The factor structure of the Y-BOCS-II-SR-T was examined with a confirmatory factor analysis to verify the obsessions and compulsions model by Mplus version 7.1. Several statistical methods were used in confirmatory factor analyses, including chi-square test, the comparative fit index (CFI), and the root mean square error of approximation (RMSEA). It was decided that a non-significant chi-square value would indicate a good fit between a model and the data. The CFI values of >0.97 were considered an indication of an adequate fit, and RMSEA values of <0.08 were accepted for model fit.21
Internal consistency was calculated with Cronbach’s alpha (α). The acceptable α values ranged from 0.70–0.95. Pearson’s correlation was used to determine convergent and divergent validity among the other measures.22 The independent samples t-test was used to examine the order effect of interview and self-report format.
Results
Descriptive statistics
The mean score of the Y-BOCS-II-SR-T total score was 20.71 (SD =11.16). The mean score of the FOCI-T was 9.00 (SD =4.67). The mean and standard deviation scores of the HAM-D and the PHQ-9 were 6.28 (SD =5.97) and 8.44 (SD =6.25), respectively, which implied normal to mild depression in the participants. The mean score of the PTQL was 35.20 (SD =11.81), which demonstrated average status in quality of life.
Reliability
Internal consistency
Cronbach’s α values revealed high internal consistencies for the total (0.94), obsession subscale (0.90), and the compulsion subscale score (0.89) of the Y-BOCS-II-SR-T.
The Cronbach’s α values for the total scores of the Y-BOCS-II-T-SS and Y-BOCS-II-T-SC were 0.94 and 0.90, respectively. The Cronbach’s α values for the FOCI-T Symptom Checklist and Severity Scale were 0.85 and 0.92, respectively. The Cronbach’s α values for the HAM-D and PHQ-9 were 0.83 and 0.89, respectively.
Correlation between Y-BOCS-II-SR-T items
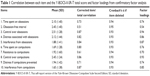
Table 1 shows the correlation between each item and the Y-BOCS-II-SR-T total score. Each item displayed good correlation with the total score. The mean scores for all items and the α values (if item deleted) were also demonstrated.
Factor structure of the Y-BOCS-II-SR-T
Confirmatory factor analysis
The sample was adequate for the factor analytic study (Kaiser–Meyer–Olkin [KMO] measure =0.899; and χ2 of Bartlett’s test of sphericity =419.09 [P<0.001]). We decided to examine the model of obsession (items 1–5) and compulsion (items 6–10) factors for two reasons. Firstly, previous studies have supported this theoretically driven obsession and compulsion model, including the Y-BOCS-II-T, which was the prototype for the Y-BOCS-II-SR-T model.23–26 Secondly, the wordings used in the scale were clearly intended to examine the severity of obsession (items 1–5) and compulsion (items 6–10). However, the results revealed poor-fit to eligible for adequate-fit model with a chi-square value of 79.26 (P=0.00; CFI =0.88; and RMSEA =0.17). Factor loadings for the individual items are presented in Table 1.
Therefore, we examined a confirmatory factor analysis (CFA) model respecification.27 Due to the fact that each item clearly inquired about obsession or compulsion, we decided not to respecify the pattern of relationships between the items and the factors, nor eliminate the factors. We then inspected the modification indices in order to refit the model by adjusting measurement errors. After we considered the modification indices combined with theoretical justifiability, we decided to adjust measurement errors between “time spent on obsessions” and “time spent on compulsions”, together with “interference from obsessions” and “interference from compulsions”.
After modification of the model, the results were an adequate fit for the obsession and compulsion factors model (χ2=36.34; P=0.27; CFI =0.99; and RMSEA =0.05). The diagram illustrating model modifications is presented in Figure 1.
Convergent and divergent validity
The Y-BOCS-II-SR-T had strong correlation with the total severity scale score of the Y-BOCS-II-T and FOCI-T in the OCD sample. In addition, the obsession and compulsion subscales of the Y-BOCS-II-SR-T had strong correlation with the Y-BOCS-II-T obsession and compulsion subscales, respectively. Furthermore, the Y-BOCS-II-SR-T had moderate correlation with the HAM-D, PHQ-9, and the PTQL. All results implied good convergent and divergent validity of the Y-BOCS-II-SR-T (Table 2).
Order effect of interview and self-report format
This study also compared the order effect of the interview and self-report format. By using the independent samples t-test method, the result indicated no difference in the order of the clinician-interview and self-report format (P=0.96).
Discussion
This is the first study to develop and evaluate the psychometric properties of the developed self-report version of the Y-BOCS-II as a measure for OCD symptom severity. Even though it was produced in the Thai language, it might interest all clinicians around the world who have taken care of OCD patients, and it might be useful for other researchers in developing a self-report version of the Y-BOCS-II in their own languages. The mean score for the Y-BOCS-II-SR-T was relatively low (20.71), which might be because all participants in the current study had been receiving treatment. The total score, obsession subscale, and compulsion subscale scores showed excellent internal consistencies. The total score Cronbach’s α value was similar to the clinician-interview Y-BOCS-II-T,11 while the results from the obsession and compulsion subscale scores of the Y-BOCS-II-SR-T were lower. The confirmatory factor analyses, after model modification, found a model that fitted with obsession and compulsion, which was consistent with the original theory-driven factor analysis.1,2,23–26,28 Since this is the first study of a self-report version of Y-BOCS-II, there is no former study of its psychometric properties that we can compare our results with. Comparing our results with a study of self-report version of Y-BOCS from Korea,29 the Cronbach’s α value for total score, and the obsession and compulsion subscale scores of Y-BOCS-II-SR-T in our current study were higher.
The correlation between each item and the Y-BOCS-II-SR-T total score showed strong correlation for all items. The results were quite similar to the original Y-BOCS-II-T.11
Regarding the validity of Y-BOCS-II-SR-T, there was high correlation with the Y-BOCS-II-T in our current analysis, which was similar to Steketee et al’s study on Y-BOCS.5 Moreover, the Y-BOCS-II-SR-T and the FOCI-T were highly correlated in our current study, which implied good convergent validity. Furthermore, the Y-BOCS-II-SR-T had moderate correlation with the HAM-D, PHQ-9, and the PTQL, which demonstrated the good divergent validity and the impact of OCD severity on patients’ depressive symptoms and quality of life. Lastly, the study of the order effect showed no difference in the order of the administration for the Y-BOCS-II-SR-T and the Y-BOCS-II-T, which was consistent with previous findings.5
The present study had some limitations. Firstly, the study was conducted with a small number of OCD participants. However, the total number of participants was adequate for the range of factor loading value found in this study.21 Secondly, the test–retest reliability and treatment sensitivity of the Y-BOCS-II-SR-T were not examined in the current study because of the long follow-up period required for the OCD participants in this study. Test–retest reliability should be assessed at baseline and 1–2 weeks later. However, most of the participants’ follow-up appointments at the hospital occurred after 1 month or more, which was too long to assess test–retest reliability.
Conclusion
Our results indicate that the Y-BOCS-II-SR-T is a psychometrically acceptable and valid measure for assessing obsessive–compulsive symptoms and severity.
Acknowledgments
This study was supported by a grant from the Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand. We would like to thank Assistant Professor Teradech Chai-Aroon, Faculty of Social Sciences and Humanities, Mahidol University, Bangkok, Thailand for his kind help in statistical methodology.
Disclosure
The authors report no conflicts of interest in this work.
References
Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–1011. | ||
Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry. 1989;46:1012–1016. | ||
Frost RO, Steketee G, Krause MS, Trepanier KL. The relationship of the Yale-Brown Obsessive Compulsive Scale (YBOCS) to other measures of obsessive compulsive symptoms in a nonclinical population. J Pers Assess. 1995;65:158–168. | ||
Deacon BJ, Abramowitz JS. The Yale-Brown Obsessive Compulsive Scale: factor analysis, construct validity, and suggestions for refinement. J Anxiety Disord. 2005;19:573–585. | ||
Steketee G, Frost R, Bogart K. The Yale-Brown Obsessive Compulsive Scale: interview versus self-report. Behav Res Ther. 1996;34: 675–684. | ||
Wu KD, Watson D, Clark LA. A self-report version of the Yale-Brown Obsessive-Compulsive Scale Symptom Checklist: psychometric properties of factor-based scales in three samples. J Anxiety Disord. 2007;21:644–661. | ||
Federici A, Summerfeldt LJ, Harrington JL, et al. Consistency between self-report and clinician-administered versions of the Yale-Brown Obsessive-Compulsive Scale. J Anxiety Disord. 2010;24:729–733. | ||
Storch EA, Rasmussen SA, Price LH, Larson MJ, Murphy TK, Goodman WK. Development and psychometric evaluation of the Yale-Brown Obsessive-Compulsive Scale – Second Edition. Psychol Assess. 2010;22:223–232. | ||
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. | ||
Kittirattanapaiboon P, Khamwongpin M. The validity of the Mini International Neuropsychiatric Interview (MINI)-Thai version. Journal of Mental Health of Thailand. 2005;13:126–136. | ||
Hiranyatheb T, Saipanish R, Lotrakul M. Reliability and validity of the Thai version of the Yale-Brown Obsessive Compulsive Scale – Second Edition in clinical samples. Neuropsychiatr Dis Treat. 2014;10:471–477. | ||
Storch EA, Larson MJ, Price LH, Rasmussen SA, Murphy TK, Goodman WK. Psychometric analysis of the Yale-Brown Obsessive-Compulsive Scale Second Edition Symptom Checklist. J Anxiety Disord. 2010;24:650–656. | ||
Storch EA, Kaufman DA, Bagner D, et al. Florida Obsessive-Compulsive Inventory: development, reliability, and validity. J Clin Psychol. 2007;63:851–859. | ||
Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont). 2007;4:28–37. | ||
Saipanish R, Hiranyatheb T, Lotrakul M. Reliability and validity of the Thai version of the Florida Obsessive-Compulsive Inventory. Scientific World Journal. 2015;2015:240787. | ||
Phattharayuttawat S, Ngamthipwatthana T, Pitiyawaranun B. The development of the Pictorial Thai Quality of Life. J Med Assoc Thai. 2005;88:1605–1618. | ||
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. | ||
Lotrakul M, Sukanit P, Sukying C. The validity and reliability of the Hamilton Rating scale for depression, Thai version. J Med Assoc Thai. 1996;41:235–246. | ||
Kroenke K, Spitzer RL, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. | ||
Lotrakul M, Sumrithe S, Saipanish R. Reliability and validity of the Thai version of the PHQ-9. BMC Psychiatry. 2008;8:46. | ||
Hair JF Jr, Black WC, Babin BJ, Anderson RE. Multivariate Data Analysis. 7th ed. Upper Saddle River, NJ: Prentice Hall; 2010. | ||
Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–55. | ||
McKay D, Danyko S, Neziroglu F, Yaryura-Tobias JA. Factor structure of the Yale-Brown Obsessive-Compulsive Scale: a two dimensional measure. Behav Res Ther. 1995;33:865–869. | ||
Amir N, Foa EB, Coles ME. Factor structure of the Yale–Brown Obsessive Compulsive Scale. Psychol Assess. 1997;9:312–316. | ||
Arrindell WA, de Vlaming IH, Eisenhardt BM, van Berkum DE, Kwee MG. Cross-cultural validity of the Yale-Brown Obsessive Compulsive Scale. J Behav Ther Exp Psychiatry. 2002;33:159–176. | ||
Storch EA, Shapira NA, Dimoulas E, Geffken GR, Murphy TK, Goodman WK. Yale-Brown Obsessive Compulsive Scale: the dimensional structure revisited. Depress Anxiety. 2005;22:28–35. | ||
Brown TA, Moore MT. Confirmatory factor analysis. In: Hoyle R, editor. Handbook of Structural Equation Modeling. New York, NY: Guilford Publications, Inc; 2012:361–379. | ||
Anholt GE, van Oppen P, Cath DC, et al. The Yale-Brown Obsessive-Compulsive scale: factor structure of a large sample. Front Psychiatry. 2010;1:18. | ||
Seol SH, Kwon JS, Shin MS. Korean self-report version of the yale-brown obsessive-compulsive scale: factor structure, reliability, and validity. Psychiatry Investig. 2013;10:17–25. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.