Back to Journals » Nature and Science of Sleep » Volume 14
Relationships Among Trajectories of Sleep Disturbance, Depression, and Antiretroviral Therapy in Persons Newly Diagnosed with HIV: A One-and-a-Half-Year Observational Longitudinal Study
Authors Chen CC , Liu HY, Chen YC , Ko NY
Received 19 June 2022
Accepted for publication 14 November 2022
Published 2 December 2022 Volume 2022:14 Pages 2133—2142
DOI https://doi.org/10.2147/NSS.S377464
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ahmed BaHammam
Chang-Chun Chen,1 Hsiao-Ying Liu,2 Yen-Chin Chen,1– 3 Nai-Ying Ko1– 3
1Department of Nursing, College of Medicine, National Cheng Kung University, Tainan, Taiwan; 2Department of Nursing, National Cheng Kung University Hospital, Tainan, Taiwan; 3Research and Development Committee, Taiwan AIDS Nurse Association, Taipei, Taiwan
Correspondence: Yen-Chin Chen; Nai-Ying Ko, No.138, Sheng Li Road, Tainan, Taiwan, Tel +886 2353535 2019, Fax +886 2377550, Email [email protected]; [email protected]
Purpose: Sleep disturbance is one of the most prevalent symptoms among persons living with HIV (PLWH). However, the trajectory of sleep patterns in persons newly diagnosed with HIV remains underrecognized. The current study aimed to estimate the trajectory of sleep quality and its associated factors among newly diagnosed PLWH.
Patients and Methods: A prospective study was conducted in the outpatient clinic of a medical center in southern Taiwan from January 2015 to December 2017. Our primary outcome was sleep quality using the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI). Participants completed the questionnaire at baseline and at four follow-up interval visits: at 3– 6, 6– 9, 9– 12 and 12– 15 months. A generalized equation estimation (GEE) model was applied to analyze the relationships among poor sleep quality, depression and antiretroviral therapy among persons newly diagnosed with HIV.
Results: A total of 217 PLWH were included. The mean age of the sample was 29.3 years, and males (98.6%) were predominant. A total of 56.2% of HIV-infected persons were considered to have poor sleep quality at baseline. After controlling for the confounding effects of demographic characteristics, the following factors increased the risk of poor sleep quality: older age (ß= 0.07, CI: 0.03– 0.11, p=0.001), level of depression (ß= 0.32, CI: 0.27– 0.37, p< 0.001) and detectable viral load (ß= 0.61, CI: 0.04 – 1.18, p= 0.037). However, there was no significant difference in BMI, CD4 counts, HIV viral load, disclosure status, or highly active antiretroviral therapy (HAART) regimen.
Conclusion: Our results demonstrate that one in two persons with newly diagnosed HIV had poor sleep quality. Being older, having higher levels of depression, and having detectable HIV viral loads were identified as risk factors for developing poor sleep quality in persons living with HIV.
Keywords: HIV, sleep disturbance, depression, highly active antiretroviral therapy, HAART
Introduction
Human immunodeficiency virus (HIV) infection is a manageable chronic disease with antiviral drug therapy. In Taiwan, the HIV mortality rate has been reduced since the introduction of highly active antiretroviral therapy (HAART) in 1997.1 The overall survival time increased by an average of 13 years compared to the non-HAART era.2 With the increase in life expectancy, the quality of life of people living with HIV (PLWH) is an issue to be considered.
Sleep disturbance is the most common symptom that interferes with the quality of life of PLWH. HIV-infected people have a higher prevalence rate of sleep disturbance, ranging from 30% to 70%, than those without HIV.3–5 HIV patients have sleep-related problems, including obstructive sleep apnea syndrome (OSAS), insomnia, and daytime sleepiness.6–8 In Taiwan, a population-based study revealed that HIV patients had a 3.7 times higher risk of sleep disturbances than the general population, and even compared to cancer patients, PLWH were still at increased risk for sleep disturbances.7 However, the cause of sleep disturbances remains controversial. Prior literature indicated that the onset of sleep disturbances may result from immune deficiency, depression, social support, medication prescriptions, and sleep disorders.9,10
The impacts of HIV infection on psychological status and prejudice and social stigma may put PLWH at higher risk of depression, which induces sleep disturbances. Previous studies support that depressive symptoms are a crucial factor related to sleep disturbances, for which the risk ratio is 3–16 times that of those without depression.4,8 In addition to psychological factors, health-related problems (eg, opportunistic infections) caused by immune deficiency and side effects of HAART are also common effects on sleep quality among PLWH.9 Consecutive care with rolling adjustments based on the patients’ health status and good compliance with ART for PLWH might improve their mental health and sleep quality.11 However, a recent study observed that after 9 months of follow-up, the sleep quality of most men who have sex with men (MSM) and bisexual men who live with HIV did not change. Only 17% of them improved, and 10% of the subjects have lower sleep quality.12 Moreover, a 6-year follow-up study show PLWH with undetectable viral load are more likely to be in the recovery pattern than those with higher viral load, but CD4 count and use of HAART were not associated with certain trajectories.13 Although most of the prior cross-sectional investigations that applied questionnaires indicated that sleep and emotional disturbances are common problems among PLWH,14–18 prospective follow-up of sleep patterns among HIV-infected persons receiving antiviral drug treatment is still rare.19
To our knowledge, two prospective studies investigated sleep changes over time in PLWH. Rogers et al19 recruited 240 PLWH and found that the more sleep problems they experienced resulted in worse cognitive functions and low energy/vitality. However, the study observed sleep quality changes did not significantly correlate to depression. The other study conducted by Downing et al12 who found that 50.1% (505) gay and bisexual reported having stable good sleep quality during one-year observation period. Sleep quality decline in PLWH was significantly associated with greater depression and anxiety, as well as lower HAART adherence. However, the study focused on a sample of gay and bisexual men living with HIV, and inconsistent results on the sleep changes and the relationships between sleep quality and depression over time. Therefore, we still need prospective longitudinal studies to describe patterns of sleep quality and depression among newly diagnosed HIV patients receiving antiretroviral therapy for the first time and to identify associated factors of the changes in the trajectory of sleep quality.
Materials and Methods
The data were collected as part of a prospective longitudinal HIV case management model intervention service project (ER-98-090). This research was performed in accordance with relevant regulations. We assessed patients’ physio-psychological status at different time points (from T0 to T4) at each clinic visit. The interval of each time point was 3–6 months. T0 is the first clinic visit; T1 is the time within 3–6 months after initial diagnosis; T2 is the time within 6–9 months after initial diagnosis; T3 is the time within 9 months to 1 year after initial diagnosis; and T4 is the time within 1 –1.5 years after initial diagnosis after obtaining informed consent from the participants.
Participants
A convenience sample of 217 adults with a new HIV diagnosis was enrolled in this study over a 2-year period (January 2015–December 2017). The newly diagnosed HIV was defined as individual has been reported to Centers for Disease Control and Prevention (CDC), completed the registration process and has been provided with a CDC registration number and clinic card. The sample size was calculated using G-power software with a CI of 95% and power of 95%, using repeated measures method with effect size 0.20, five-time measurement. The estimated sample size was 168; we adjusted this sample size to account for possible dropouts and non-responders (20%) resulting in a total estimated sample size of 202 participants.
This study was conducted in the outpatient clinic of a medical center in southern Taiwan. Eligible participants were Chinese- or Taiwanese-speaking, at least 20 years old and newly diagnosed with HIV before enrollment. Individuals were excluded if they had been pregnant, reported acute psychological disorders, or had unstable conditions.
Measurements
The physio-psychological survey included demographic information on age, sex, level of education, job type, BMI, disclosure status, psychiatric history, length of time since HIV diagnosis, CD4 counts, HIV viral load, and HAART regimen. Two randomized controlled trials (The TEMPRANO and SRART) have provided evidence that early initiation of HAART is associated with a more favorable treatment.20,21 World Health Organization (WHO) recommended treatment as prevention in 2015 that all patients be treated at any CD4 count with HAART once HIV infection is diagnosed.22 Subsequently, the Taiwan HIV/AIDS treatment guideline in 2016 recommended for initiation of HAART is a CD4 count at any level in persons diagnosed HIV positive. The physician would follow Taiwan CDC recommendation, in the initiation of HAART would be tried the first-line treatment, which includes Atripla (EFV/FTC/TDF), Odefsey (RPV/FTC/TAF), Triumeq (ABC/3TC/DTG), Biktarvy (TAF/FTC/BIC) and Delstrigo (DOR/3TC/TDF). In case of failure on first-line regimen, physician needed to apply second-line ART such as dolutegravir (ETR), dolutegravir (DTG).23
The HAART regimen was classified into three groups according to each individual’s pharmacy refill records: nonnucleoside reverse transcriptase inhibitors (NNRTIs), integrase strand transfer inhibitors (INSTIs), and protease inhibitors (PIs). Viral load undetectable was defined as being less than 20 copies/mL.
Sleep quality was evaluated by the Chinese version of the Pittsburgh Sleep Quality Index (C-PSQI). The C-PSQI is widely performed to evaluate subjective sleep quality and consists of 24 items and 7 dimensions with a total score ranging from 0 to 21 points (Cronbach’s α = 0.83). Subjects with a score higher than 5 points were defined as having poor sleep quality.24
Depressive symptoms were evaluated by the short form of the Center for Epidemiologic Studies Depression (CES-D) scale, which consists of 10 items with a total score ranging from 0 to 30 points (Cronbach’s α = 0.88).25 Subjects with a score of 10 to 19 points were defined as having mild depressive symptoms, and 20 to 30 points were defined as having severe depressive symptoms.25
Data Analysis
The data analyses were conducted using R software version 4.0.3.26,27 Descriptive statistics were used to summarize the mean PSQI and depression scores across the 5 time point assessments for newly diagnosed people with HIV. A mixed model analysis of variance (ANOVA) was used to verify the differences in the PSQI score among different levels of depression and HAART regimens at each time point. The generalized estimating equation (GEE) was used to investigate the associated factors of the changes in the trajectory of sleep quality among newly diagnosed people with HIV infection. This study was approved by the Human Research Committee at National Cheng Kung University Hospital (B-ER-109-352). All participants provided written consent and written authorization for their health care providers to release their medical records for research purposes.
Results
Distribution of Participants’ Characteristics Across Time
A total of 217 HIV-infected patients (mean age=29.4 years, SD=7.5 years) participated. The attrition rate at the 5-time point assessment was 29.5%. Of these patients at baseline (T0), 122 (56.2%) were categorized as having poor sleep quality, and 82 (37.8%) were categorized as having mild or severe depression. The distribution curve of CD4 counts at baseline showed that approximately 74.7% of the patients’ CD4 counts were lower than 500 cells/mm3 (Supplementary Figure 1), and mean viral load of the patients was 2.94 log.10 Among these patients, NNRTIs were the most common HAART regimen (83.5%). The trajectories of the participants’ characteristics indicated an increased percentage of full-time jobs (p=0.002) and length of time since HIV diagnosis (p<0.001), higher BMIs (p=0.003) and CD4 counts (p<0.001), and decreased viral loads (p<0.001) (Table 1).
 |
Table 1 The Trajectories of Participants’ Characteristics According to Different Time Measurements (N = 217) |
Mean Change in Sleep Quality and Depression Levels
As shown in Figure 1, the trajectory for sleep quality from baseline to the T4 time point between 1 and 1.5 years showed a U shape, which means that patients’ self-reported sleep quality decreased first and then increased on T3. In addition, the trajectory of depression score results was similar to the sleep quality trajectory. The linear regression line showed a slightly falling trend of sleep quality (p=0.08) and depressive (p=0.10) conditions among people with new HIV diagnosed during the 5-time point assessment. However, the multiple comparison test (Kruskal–Wallis test) showed no difference between each time point.
Association of Sleep Quality at Different Depression Levels Across Time
As shown in Figure 2, poor sleep quality was borderline significantly associated with a higher level of depression over time (p = 0.06). The sleep quality trajectory of persons newly diagnosed with HIV with normal depression levels remained stable and significantly better than that of the mild and severe groups. However, the sleep quality of people with severe depression improved from T0 to T2 (p=0.19) and then worsened from T2 to T4 (p=0.37).
Association of Sleep Quality with Different ART Regimens Across Time
As shown in Figure 3, we found that sleep quality in the INSTIs group was not significantly poorer than that in patients in the other ART regimen groups during the T1 to T4 time points (p=0.24).
Factors Associated with Sleep Quality Trajectory
In the GEE model, we found that increasing age (ß= 0.07, p=0.001), higher depression scores (ß= 0.32, p<0.001), and detectable viral load (ß=0.61, p=0.04) were associated with poor sleep quality when controlling for other factors (Table 2).
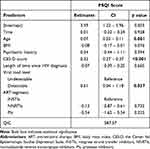 |
Table 2 Factors Associated with Poor Sleep Quality |
Discussion
This study is one of few prospective studies to evaluate changes in sleep quality and level of depression trajectory among PLWH who have recently started ART.12,19 Our findings indicated that the prevalence of poor sleep quality and moderate/severe depression among PLWH with newly diagnosed HIV ranged from 56.2% to 47.7% and 37.7% to 28.1%, respectively. To our knowledge, few studies have investigated the trajectory of sleep quality and level of depression among PLWH with new HIV diagnoses. Our study result is somewhat in agreement with previous studies that included HIV patients with HAART.12,14–18 In addition, the findings in the current study were similar to the results reported in China, which showed that the level of depression decreased from 23.0% at baseline to 14.0% at month 12 post-treatment.11 Also consistent with a prospective observational study conducted by Downing et al,12 the result showed that two sleep quality trajectory groups (bad sleep quality maintained and sleep quality negative change) were highly associated with depression. This suggests that screening for sleep quality and mental health problems is greatly warranted for PLWH who have new HIV diagnoses.
Prior studies indicated that uncontrolled HIV infection is associated with increased systemic levels of proinflammatory cytokines leading to the development of sleep disturbances.28 Our study also showed that undetectable HIV viral load increases the possibility of experiencing poor sleep quality. This is consistent with previous studies, which found that increased CD4 counts were associated with sleep quality improvements due to patients’ overall health improving after HAART.29,30 However, another study conducted in South Africa showed that both the overall CD4 count rebound and higher current CD4 counts were negative associated with sleep quality.31 The differences in findings may be due to the differences in ethnicity and gender composition, as well as the fact that patients in South Africa seem to have delayed access to HIV treatment. Especially, when PLWH have delayed start with HAART, which has been associated with CD4 effector T cells being more spontaneously activated and leads to AIDS.32 Our findings demonstrate that PLWH receiving ART have viral suppression, which contributes to improved sleep quality.
Factors associated with poor sleep quality in PLWH, such as getting older and a higher intensity of depression, were also found in our study.4,16,17 The relationship between getting older and poor sleep quality might be related to various factors, such as age-related sleep architecture and growth hormone changes.33 Given the association between poor sleep and emotional disorders, there might be linkages between sleep, emotional regulation and alteration in the hypothalamic–pituitary–adrenal axis implication of psychopathology and sleep–wake cycle. Given the bidirectional association between sleep and depression, targeted management of one may improve the other. The implication would be that treating depression might help to improve sleep quality, and addressing sleep difficulties early may relieve psychological morbidity.
Regarding HIV treatment, we found that patients who had initiated an INSTI-based regimen did not have a higher rate of sleep disturbances over time compared to the NNRTI- and PI-based groups during the observation period of 1.5 years. Similar to the findings of a multicenter observational study in China, there were no significant associations between efavirenz-containing regimens and sleep disturbances.4,34 However, our finding was contrary to previous studies, which have largely focused on the impact of specific antiretroviral agents on poor sleep quality due to the neuropsychiatric adverse effects frequently occurring in efavirenz- or INSTI-based regimen users.35,36 The reasons for the conflicting results between these trials and our data might be the different study purposes. These trials aimed to examine the effects of delayed switch and dolutegravir discontinuation on neuropsychiatric adverse effects. Further study exploring the relationship between INSTI-based regimens and sleep is warranted.
However, our study has some limitations. First, each participant was selected by convenience sampling, and the findings may not be generalizable to all PLWH in Taiwan. Second, the effect of ART on sleep quality at months 12 and 15 may be under-evaluated due to a 30% attrition rate. Third, sleep quality and emotional problems in this study were measured by questionnaires. Further studies are encouraged to measure objective biomarkers such as sleep efficiency and total sleep time; it would be helpful to better understand the nature of sleep disturbances in PLWH. Finally, this study lacks long-term taking HAART-related symptoms, such as electrolyte imbalance, that might compromise our findings.
Conclusion
The trajectory of sleep quality among newly diagnosed HIV patients presents a linear decline regression line during the 5-time point assessment. Depression evaluations and daily regular antiretroviral treatment may prevent sleep disturbances among people newly diagnosed with HIV. The objective measurements for investigating the trajectory of sleep quality in newly diagnosed HIV infection are warranted to need.
Acknowledgments
The authors would like to thank the HIV case managers at National Cheng Kung University Hospital who participated in the study. This research was supported by National Cheng Kung University Hospital (NCKUH-11107017), and National Science and Technology Council (NSTC 111-2314-B-006-027).
Disclosure
The authors report no conflicts of interest in this work. We confirm that our study complies with the Declaration of Helsinki.
References
1. Yang CH, Huang YF, Hsiao CF, et al. Trends of mortality and causes of death among HIV‐infected patients in Taiwan, 1984–2005. HIV Med. 2008;9(7):535–543. doi:10.1111/j.1468-1293.2008.00600.x
2. Wing EJ. HIV and aging. Int J Infect Dis. 2016;53:61–68. doi:10.1016/j.ijid.2016.10.004
3. Allavena C, Guimard T, Billaud E, et al. Prevalence and risk factors of sleep disturbance in a large HIV-infected adult population. AIDS Behav. 2016;20(2):339–344. doi:10.1007/s10461-015-1160-5
4. Huang X, Li H, Meyers K, et al. Burden of sleep disturbances and associated risk factors: a cross-sectional survey among HIV-infected persons on antiretroviral therapy across China. Sci Rep. 2017;7(1):1–8. doi:10.1038/s41598-016-0028-x
5. Reid S, Dwyer J. Insomnia in HIV infection: a systematic review of prevalence, correlates, and management. Psychosom Med. 2005;67(2):260–269. doi:10.1097/01.psy.0000151771.46127.df
6. Chen YC, Lin CY, Li CY, Zhang Y, Ko WC, Ko NY. Obstructive sleep apnea among HIV-infected men in the highly active antiretroviral therapy era: a nation-wide longitudinal cohort study in Taiwan, 2000–2011. Sleep Med. 2020;65:89–95. doi:10.1016/j.sleep.2019.07.011
7. Chen YC, Lin CY, Strong C, et al. Sleep disturbances at the time of a new diagnosis: a comparative study of human immunodeficiency virus patients, cancer patients, and general population controls. Sleep Med. 2017;36:38–43. doi:10.1016/j.sleep.2017.04.005
8. Crum-Cianflone NF, Roediger MP, Moore DJ, et al. Prevalence and factors associated with sleep disturbances among early-treated HIV-infected persons. Clin Infect Dis. 2012;54(10):1485–1494. doi:10.1093/cid/cis192
9. Wibbeler T, Reichelt D, Husstedt I-W, Evers S. Sleepiness and sleep quality in patients with HIV infection. J Psychosom Res. 2012;72(6):439–442. doi:10.1016/j.jpsychores.2012.03.003
10. Fekete EM, Williams SL, Skinta MD. Internalised HIV-stigma, loneliness, depressive symptoms and sleep quality in people living with HIV. Psychol Health. 2018;33(3):398–415. doi:10.1080/08870446.2017.1357816
11. Xie J, Wang Z, Li Q, et al. Associations between antiretroviral therapy-related experiences and mental health status among people living with HIV in China: a prospective observational cohort study. AIDS Res Ther. 2021;18(1):60. doi:10.1186/s12981-021-00370-y
12. Downing MJ, Millar BM, Hirshfield S. Changes in sleep quality and associated health outcomes among gay and bisexual men living with HIV. Behav Sleep Med. 2020;18(3):406–419. doi:10.1080/15402002.2019.1604344
13. Womack JA, Murphy TE, Bathulapalli H, et al. Trajectories of sleep disturbance severity in HIV-infected and uninfected veterans. J Assoc Nurses AIDS Care. 2017;28(3):431–437. doi:10.1016/j.jana.2017.02.006
14. Oshinaike OO, Akinbami AA, Ojo OO, Ojini IF, Okubadejo UN, Danesi AM. Comparison of the minimental state examination scale and the international HIV dementia scale in assessing cognitive function in Nigerian HIV patients on antiretroviral therapy. AIDS Res Treat. 2012;2012:581531. doi:10.1155/2012/581531
15. Gutierrez J, Tedaldi EM, Armon C, Patel V, Hart R, Buchacz K. Sleep disturbances in HIV-infected patients associated with depression and high risk of obstructive sleep apnea. SAGE Open Med. 2019;7:2050312119842268. doi:10.1177/2050312119842268
16. Bedaso A, Abraham Y, Temesgen A, Mekonnen N. Quality of sleep and associated factors among people living with HIV/AIDS attending ART clinic at Hawassa University comprehensive specialized Hospital, Hawassa, SNNPR, Ethiopia. PLoS One. 2020;15(6):e0233849. doi:10.1371/journal.pone.0233849
17. Mengistu N, Azale T, Yimer S, Fikreyesus M, Melaku E, Shumye S. Quality of sleep and associated factors among people living with HIV/AIDS on follow up at Ethiopian Zewditu Memorial Hospital, 2018. Sleep Sci Pract. 2021;5(1):2. doi:10.1186/s41606-020-00056-w
18. Wu J, Wu H, Lu C, Guo L, Li P. Self-reported sleep disturbances in HIV-infected people: a meta-analysis of prevalence and moderators. Sleep Med. 2015;16(8):901–907. doi:10.1016/j.sleep.2015.03.027
19. Rogers BG, Lee JS, Bainter SA, Bedoya CA, Pinkston M, Safren SA. A multilevel examination of sleep, depression, and quality of life in people living with HIV/AIDS. J Health Psychol. 2020;25(10–11):1556–1566. doi:10.1177/1359105318765632
20. Lundgren JD, Babiker AG, Gordin F, et al. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795–807. doi:10.1056/NEJMoa1506816
21. Danel C, Moh R. A trial of early antiretrovirals and isoniazid preventive therapy in Africa. N Engl J Med. 2015;373(9):808–822. doi:10.1056/NEJMoa1507198
22. World Health Organization. Guideline on When to Start Antiretroviral Therapy and on Pre-Exposure Prophylaxis for HIV. World Health Organization; 2015.
23. Taiwan AIDS Society. Guidelines for diagnosis and treatment of HIV/AIDS. Taiwan; 2020. Available from: http://www.aids-care.org.tw/journal/treatment.php.
24. Tsai PS, Wang SY, Wang MY, et al. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res. 2005;14(8):1943–1952. doi:10.1007/s11136-005-4346-x
25. Zhang W, O’Brien N, Forrest JI, et al. Validating a Shortened Depression Scale (10 Item CES-D) among HIV-Positive People in British Columbia, Canada. PLoS One. 2012;7(7):e40793. doi:10.1371/journal.pone.0040793
26. R Core Team.R: A Language and Environment for Statistical Computing [Computer Program]. Vienna, Austria: R Foundation for Statistical Computing; 2020.
27. Højsgaard S, Halekoh U, Yan J. The R package geepack for generalized estimating equations. J Stat Softw. 2006;15:1–11.
28. O’Brien K, Riddell N, Gómez-Olivé F, Rae D, Scheuermaier K, von Schantz M. Sleep Disturbances in HIV Infection and their biological basis. Sleep Med Rev. 2021;65:101571. doi:10.1016/j.smrv.2021.101571
29. Seay JS, McIntosh R, Fekete EM, et al. Self-reported sleep disturbance is associated with lower CD4 count and 24-h urinary dopamine levels in ethnic minority women living with HIV. Psychoneuroendocrinology. 2013;38(11):2647–2653. doi:10.1016/j.psyneuen.2013.06.022
30. Oshinaike O, Akinbami A, Ojelabi O, Dada A, Dosunmu A, John Olabode S. Quality of sleep in an HIV population on antiretroviral therapy at an Urban Tertiary Centre in Lagos, Nigeria. Neurol Res Int. 2014;2014:298703. doi:10.1155/2014/298703
31. Redman KN, Karstaedt AS, Scheuermaier K. Increased CD4 counts, pain and depression are correlates of lower sleep quality in treated HIV positive patients with low baseline CD4 counts. Brain Behav Immun. 2018;69:548–555. doi:10.1016/j.bbi.2018.02.002
32. Paiardini M, Muller-Trutwin M. HIV-associated chronic immune activation. Immunol Rev. 2013;254(1):78–101. doi:10.1111/imr.12079
33. Nicolaides NC. HPA Axis and Sleep. NCBI Bookshelf; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279071/.
34. Nguyen A, Calmy A, Delhumeau C, et al. A randomized crossover study to compare efavirenz and etravirine treatment. AIDS. 2011;25(1):57–63. doi:10.1097/QAD.0b013e32833f9f63
35. Waters L, Fisher M, Winston A, et al. A Phase IV, double-blind, multicentre, randomized, placebo-controlled, pilot study to assess the feasibility of switching individuals receiving efavirenz with continuing central nervous system adverse events to etravirine. AIDS. 2011;25(1):65–71. doi:10.1097/QAD.0b013e328341685b
36. Hoffmann C, Welz T, Sabranski M, et al. Higher rates of neuropsychiatric adverse events leading to dolutegravir discontinuation in women and older patients. HIV Med. 2017;18(1):56–63. doi:10.1111/hiv.12468
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.