Back to Journals » Risk Management and Healthcare Policy » Volume 14
Relationship Between Risk Perception, Social Support, and Mental Health Among General Chinese Population During the COVID-19 Pandemic
Authors Liu C, Huang N, Fu M , Zhang H, Feng XL , Guo J
Received 19 January 2021
Accepted for publication 14 April 2021
Published 7 May 2021 Volume 2021:14 Pages 1843—1853
DOI https://doi.org/10.2147/RMHP.S302521
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Chengbin Liu,1 Ning Huang,1 Mingqi Fu,2 Hui Zhang,1 Xing Lin Feng,3 Jing Guo3
1School of Sociology, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 2Center for Social Security Studies, Wuhan University, Wuhan, People’s Republic of China; 3Department of Health Policy and Management, School of Public Health, Peking University, Beijing, People’s Republic of China
Correspondence: Jing Guo
Department of Health Policy and Management, School of Public Health, Peking University, 38 Xueyuan Road, Beijing, 100191, People’s Republic of China
Tel +86-18086471505
Email [email protected]
Background: The Coronavirus Diseases (COVID-19) pandemic is a global public health challenge and provides an opportunity to investigate the unclear relationship between risk perception, social support, and mental health. This study aims to examine the association between risk perception and mental health while taking social support as a moderator.
Methods: An online cross-sectional study recruiting 2993 participants was conducted in China, from 1st to 10th, February 2020. The relationship between risk perception, social support, and mental health was examined using multivariate linear regression analyses.
Results: This study indicated that risk perception was associated with a higher level of mental health symptoms. The subscale “Perceived uncontrollability” seemed to present a stronger correlation with depressive symptoms (Beta=0.306) and post-traumatic stress disorder (PTSD) symptoms (Beta=0.318) than the subscale “Perceived Severity” did. Moreover, social support moderated the relationship between perceived uncontrollability and mental health symptoms.
Conclusion: In the context of the COVID-19 pandemic, it is necessary to design mental health strategies and programs from a risk perception perspective (more mental health strategies should be delivered to build reasonable risk perception), while social support from family and friends may be protective to against depressive symptoms and PTSD symptoms. There is a demand for mental health intervention from a risk perception perspective.
Keywords: risk perception, social support, depressive symptoms, PTSD symptoms, SARS-CoV-2
Introduction
The novel coronavirus disease (COVID-19) has evolved into a global crisis since its onset at the end of 2019. The highly infectious COVID-19 affects not only physical health but also mental health among general populations.1,2 Among which, PTSD and depressive symptoms were recognized as the most prevalent ones.3 These emerging mental health symptoms related to the COVID-19 could hinder the prevention and control of the epidemic and may evolve into long-term health problems.4 Thus, it is critical to examine the mental health status in the general population during the COVID-19 outbreak.5
Risk Perception and Mental Health
Based on the cognitive appraisal theory,6 perceived risks of COVID-19 can be regarded as one form of threat appraisal and thus a determinant of psychological health responses. However, the relationship between risk perception and mental health has only been examined in few studies and remains unclear.7 For example, while some studies suggesting a negative correlation of risk perception with mental health,8 another study claimed that this association was insignificant.9 Different conclusions could be attributed to the variance in sample selection, methodologies, and social settings between studies. Moreover, given the high infection risk and the acute threat of this pandemic, risk perception towards COVID-19, a negative event with a higher likelihood, is somewhat different from that towards risks of rare events like nuclear leaks, other life-threatening diseases, and even SARS.10,11 Thus, an empirical study is required to further elucidate the relationship between risk perception and mental health during the COVID-19 crisis.
Moreover, risk perception is a subjective-construction process consisting of multiple dimensions, such as judgments on the severity and controllability of risks.12 According to the cognitive appraisal theory, when people encounter a threat/risk, they will evaluate the characteristics of threat/risk through two stages. In the first stage, people assess the consequences of the threat, reflecting individuals’ perceived severity of COVID-19 risk. After people assess the severity of a negative event, they consider how they could control or avoid it in the second stage. It involves assessment of controllability and knowledge of the threat, mainly reflecting peoples’ perceived controllability of COVID-19 risk.6 Thus, risk perception towards COVID-19 concerns not only the potential or actual consequences of this pandemic (namely Perceived Severity later) but also the controllability over these threats (namely Perceived Controllability later). Often, these two domains of risk perception relate to different psychological patterns and mental health responses.6 Recently, a study found that the perceived controllability was associated with mental health stronger than perceived severity.13 However, results from this study require further examination, as its coefficients were not standardized and the crucial direct exposure variable was not controlled. Thus, to better understand the relationship between risk perception and mental health in the COVID-19 pandemic context, this study tries to discuss risk perception on controllability and severity, respectively.
Social Support as a Moderating Variable
More importantly, social support has the potential to moderate the association between risk perception and mental health, yet was relatively less considered by existing studies.14 Social support means both psychological and material resources to individuals,15 and was believed to be essential for mental health protection.15 According to the stress-buffering model,16 social support may reduce adverse psychological effects of negative life events on individuals’ mental health.17 Yet, the buffering effect from social support to post-traumatic stress disorder (PTSD) symptoms was doubted by some researchers.18 Interestingly, there was another study found that shows excessive social support even detrimental to mental health, as individuals with much external support are easier to lose their ability to self-adjusting.19 Thus, whether and how social support moderates the relationship between risk perception and mental health remained unclear, and more evidence should be provided.
Objectives and Hypothesis
To sum up, this study tries to examine the relationship between risk perception and mental health symptoms while taking social support as a moderator. Based on a broad literature review, three hypotheses and one explorative question were proposed in this study. First, we posited a hypothesis that higher risk perception (perceived uncontrollability and perceived severity) was associated with higher levels of depressive symptoms and PTSD symptoms during the COVID-19 pandemic. Second, taking the adverse outcomes of the pandemic on individuals into consideration, we raised an explorative question to explore whether a stronger association was found between perceived uncontrollability with mental disorders than perceived severity with mental disorders. It should be noted that we did aim to get descriptive results of this question rather than its statistical significance, because of its explorative nature. Lastly, we proposed two competing hypotheses on the role of social support in the relationship between risk perception and mental health. Social support could buffer or enhance the association from risk perception to mental health.
Materials and Methods
Study Design
This cross-sectional online questionnaire survey was conducted during the early period of the COVID-19 outbreak in China (Between February 1st– and February 10th, 2020). To avoid the spread of COVID-19 through respiratory droplets and direct contact, we collected data through the professional online survey platform “Survey Star” (Changsha Ranxing Science and Technology, Shanghai, China), and utilized the convenience and quota sampling method that focused on recruiting the general population living in mainland China. Due to the online survey that we conducted in the COVID-19 pandemic, participants with higher risk perception and limited time to access the internet may be under-represented. Thus, in order to enhance the sample’s representativeness, recruitment was targeted to seven groups, namely medical workers, service staff, social service workers, teachers and operators, students, workers and farmers, and unemployed, and others. Among these occupational groups, medical workers and relevant fields with higher infection risks and work burden, who might have more risk perception and less time to surf the internet in the public health emergency; While workers, farmers, and unemployed individuals with lower social economic status, may also perceive higher risk towards COVID-19 and have less access to the internet during the COVID-19 crisis.
Our sample size was calculated using the following formula:20 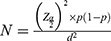 . In the sample size calculation,
. In the sample size calculation,  = the standard normal deviation at type 1 error of 5% (
= the standard normal deviation at type 1 error of 5% ( is usually set at 1.96),
is usually set at 1.96),  = the expected prevalence rate of PTSD in China based on previous research (
= the expected prevalence rate of PTSD in China based on previous research ( is set at 0.5, to make the value of
is set at 0.5, to make the value of  and sample size largest),
and sample size largest),  = absolute error or precision (
= absolute error or precision ( is recommended to set at 0.05 when 10%< p <90%).21 Therefore, the sample size calculated for the study is 384. But since there may be a refusal or non-response to participate in our study, and unusable data caused by an extremely short answer time and/or inconsistent answer patterns, we decided to collect over 384 samples from 1st to 10th February 2020, as a result, 2993 eligible samples were entered the survey.
is recommended to set at 0.05 when 10%< p <90%).21 Therefore, the sample size calculated for the study is 384. But since there may be a refusal or non-response to participate in our study, and unusable data caused by an extremely short answer time and/or inconsistent answer patterns, we decided to collect over 384 samples from 1st to 10th February 2020, as a result, 2993 eligible samples were entered the survey.
Measurements
Mental Health Status
Depressive symptoms were measured by the Center for Epidemiologic Studies Depression Scale (CESD), which is an extensively used and validated self-report inventory.22 This scale has 20 items rating symptom frequency on a 4-point scale: from 0 (less than one day) to 3 (5–7 days). The total score ranges from 0 to 60, with a higher score indicating the more severe depressive symptoms. The Cronbach’s alpha in this study was 0.93.
PTSD symptoms were assessed using a 20-item self-report PCL-5 scale, which estimates the severity of DSM-5-related PTSD symptoms during the past month.23 Respondents answered the 20 items on a 4-point rating scale from 0 (not at all) to 4 (extremely). The summation of the score ranges from 0 to 80. The higher the score indicates the higher level of PTSD symptoms. The Cronbach’s alpha was 0.97 in this study.
Social Support
Social support was assessed by the multi-dimensional scale of perceived social support (MSPSS).24 It includes 12 items, rating levels of social support from three source types: family, friends, and others (colleagues or classmates). And each item along a 7-point Likert scale, with (1) representing strongly disagree and (7) representing strongly agree. Four items in each of the subscales are summed to obtain scores for family support, friend support, and other social support, respectively. Its Cronbach’s Alpha reliability of three types of social support was 0.918, 0.932, and 0.935, respectively.
Risk Perception
Risk perception was assessed and revised from a self-report questionnaire designed by a previous researcher.25 This scale has seven items include the degree of worrying about COVID-19 (not worried at all to very worried), the impact of COVID-19 on individuals and society (very small to very large), the consequences of COVID-19 (slowly appear to immediately emerge), controllability of COVID-19 (uncontrollable to controllable), knowledge about COVID-19 (unfamiliar to familiar) et al. Factor analysis was used to get two dimensions: perceived severity and perceived uncontrollability and the KMO value of ≥0.70 indicated better justifiability of factor analysis. More details can be seen in Table 1.
 |
Table 1 Factor Analysis of Risk Perception Scale |
Confounding Variables
Socio-demographic background characteristics included gender (male, female), age (below 18, 18–25, 26–30, 31–40, 41–50, over 50), ethnicity (Han, else), religion (yes, no), marriage (yes, no), the party (political status: whether a member of the Communist Party of China or not (yes, no)), education (Junior high school and below, High school/Technical school, Junior College, Undergraduate, Postgraduate and above), job (medical workers, service staffs, social service workers, teachers and operators, students, workers and farmers, unemployed and others), and income (poor, not poor). Exposure variables included direct exposure, Wuhan exposure (yes, no), and media exposure (very frequent, often, some, almost none). Health status contained the recent state of physical health (two-week illness: whether suffered headaches or fever in the past two weeks (yes, no)) and previous state of mental health (Previous trauma: an experience of a traumatic event in the last year (yes, no)). These variables were concluded according to previous related studies.3,26,27
Statistical Analysis
Several linear regression models were used to examine the relationship between risk perception and mental health status. Besides, we also tested how three sources of social support associate with mental health, respectively. Finally, we separately added interactive variables of risk perception and social support to estimate the moderating effects of each source of social support. Each model controlled the same confounding variables: gender, age, ethnicity, marital status, party, religion, education, job, income, prior, various exposure, previous trauma, two-week illness. All analyses were carried out using Stata version 16.0 (release 16MP, Stata Corporation, College Station, TX, USA).
Results
Table 2 shows the description of the sample. Approximately 47% of the sample were male, and almost 8% of the subjects were over 50 years old. Most of the subjects belonged to the Han ethnicity (95.9%) and over 90% did not have a religion or a belief. About 42.5% of the respondents were not married, and more than 57% of subjects had a bachelor degree or above, with only 24.4% of them belonging to Party groups. In addition, workers and farmers accounted for 13.0% of the sample, while the proportion of unemployed and other occupations is 16.5%. And only 11.5% of subjects identified themselves as poor (low-income). More details of subjects can be seen in Table 2.
 |
Table 2 Descriptive Analysis of Samples Characteristics |
Table 3 displays the results of the linear regression analysis for mental health symptoms. Model 1 indicated that family and friend support strongly were associated with a lower level of depressive symptoms, but significant other support had a positive association with depressive symptoms (B= 1.637, 95% CI: 0.683, 2.592). In Model 2, risk perception strongly correlated with the high level of depressive symptoms, and the perceived uncontrollability (Beta= 0.306) seemed to have a higher correlation with depressive symptoms than perceived severity (Beta=0.049). Model 3 indicated that social support was significantly associated with PTSD symptoms. However, the degree and direction of correlations with PTSD symptoms differed, family support seemed to have a higher negative correlation with PTSD symptoms than friend support, and other support was positively associated with the level of PTSD symptoms (B=3.434 95% CI: 1.970,4.898). Model 4 showed that risk perception had significant and positive correlations with PTSD symptoms, but the strength of the association varied. Perceived uncontrollability appeared to be stronger correlated with PTSD symptoms (Beta=0.318) than perceived severity (Beta=0.092).
 |
Table 3 Multiple Linear Regression for the Relationship Between Risk Perceptions, Social Support, and Mental Health Symptoms |
Table 4 shows the results of the interaction of social support with risk perception on depressive symptoms. In Model 1, family support (B=0.517, 95% CI: 0.172, 0.862), friend support (B=0.509, 95% CI: 0.171, 0.847), and other social support (B=0.553, 95% CI: 0.216, 0.891) had a significant interaction effect on the association between perceived uncontrollability and depressive symptoms, indicating a high level of social support would enhance the effects of perceived perception on the depressive symptoms (Figure 1). But we found no significant moderation effect of each source of social support on the association between perceived severity and depressive symptoms.
 |
Table 4 Multiple Linear Regression for the Relationship Between Interactions (Risk Perception × Social Support) and Mental Health |
 |
Figure 1 The moderating effect of family support (A), friend support (B), and other social support (C) on the relationship between perceived uncontrollability and depressive symptoms. |
Model 2 in Table 4 indicated that the relationship between perceived uncontrollability and PTSD symptoms were significantly moderated by family support (B=0.634, 95% CI 0.109, 1.158), friend support (B=0.543, 95% CI: 0.029, 1.057), and other social support (B=0.692, 95% CI: 0.178, 1.206), respectively. As shown in Figure 2, individuals who reported higher levels of perceived uncontrollability and social support from three sources would have a higher level of PTSD symptoms. Again, there was no moderating effect of social support and perceived severity on PTSD symptoms.
 |
Figure 2 The moderating effect of family support (A), friend support (B), and other social support (C) on the relationship between perceived uncontrollability and PTSS symptoms. |
Discussion
Our study set out to assess the relationship between risk perception and mental health symptoms, and further examine the moderating effect of social support over this relationship. Results indicate that risk perception, especially perceived uncontrollability, significantly associates with greater depressive symptoms among Chinese populations during the COVID-19 outbreak. Besides, we find that three types of social support have different moderating effects on the association between perceived risk and mental health symptoms, which shed light on mental health protection in the future.
Our results of this study support the first hypothesis that risk perception associates with greater depressive symptoms and PTSD symptoms. As explained by the previous study, risk perception could induce greater mental health symptoms through the mediating effect of coronavirus fear.28 The more anxious people being towards the virus, the greater the psychological burden they would bear throughout the pandemic. Furthermore, the descriptive results of our exploratory question indicate that risk perception on uncontrollability seems to present a stronger association with depressive symptoms than risk perception on severity. This is because there would not be many behavioral or psychological responses if people thought the risk has no chance to occur, no matter how severe the consequences might be.29,30 Second, it could be explained that individuals had a high level of intolerance of uncertainty in the context of the COVID-19 pandemic with high infectivity and uncertainty, and then they might tend to attach more importance to the control of the unknowing risk.31 Third, the incidence and uncontrollability of COVID-19 with a higher infection force are more likely to cause people’s fear than its consequences.32 Thus, it is reasonable for this study to say that mental health protection during the COVID-19 could be considered from a risk perception perspective, risk perception on uncontrollability in particular.
In addition, we find that associations between social support and mental health vary between different social support types. Following existing studies, this study suggests that support from family and friend are helpful in against depressive symptoms and PTSD symptoms,33,34 family support in particular.35 However, this study observes that greater social support from other sources correlates with greater mental health symptoms. Reasons for these varied relationships go to the different roles each support has. According to the weak tie and strong tie theory,36,37 intimate friends and family members usually are regarded as the strong ties and generally provide practical and emotional support when people got exhausted,38 whereas other people like colleagues are often considered as weak ties and could provide more information support that would always turn into rumors spreading and negative emotions in pandemic context, which further arouse excessive pressure.39 Furthermore, since people were recommended to stay at home during the COVID-19 pandemic, they might have more time to stay with their intimate family members or friends living with or near them and receive more practical support from family and friends. However, they only can contact weak tie network members through the online social software, and then the probability to receive rumors about COVID-19 might increase through online communication with weak tie relationship members.40 Besides, the hierarchical compensation model suggests that family members and friends are the preferred sources of support for old adults in the order, with formal network least preferred and least probably to be asked support,41 and young people in China also primarily seek support from family and friend, which is correspondent with the Chinese traditional Confucian culture.42 Also, our result showed that perceived support from family and friends is much higher than that from others. Therefore, support from family and friends are potential resources for general populations to against mental disorders during the pandemic.
More importantly, our results indicate that social support moderates the relationship between perceived risk controllability and mental health symptoms. Association between risk uncontrollability perception and mental health symptoms would be enhanced if family and friend support is strong. The interaction pattern is in accordance with the “reverse buffering effect”, social support strengthens rather than weakens the positive association between stressors and negative outcomes.43 Firstly, it could be explained by the over-reciprocating supportive exchanges (high level of support received may exceed support given), it may be harmful to self-image (resulting from a state of dependency and incompetence) and sense of control over the risk.44 Secondly, excessive social support strengthened the sense of loss of control over COVID-19 risk, since individuals with high social support may have more friends or family members to worry about. Thirdly, excessive social support may reduce self-efficacy in coping with trauma and increase the sense of powerlessness,45 leading to more negative emotions. Another possible explanation may be that the poorer mental health is, the lower is the “buffer effect” of family and friend support. Thus, excessive social support from family and friends could enhance the positive correlation between perceived uncontrollability and mental health symptoms. Also, individuals could perceive greater uncontrollability with worse mental health when they perceived more support from others like colleagues. This is because other people as a kind of weak tie often convey negative information support that may not be obtained from the strong tie, and it may elevate the risk perception, based on the weak tie theory.37 And this explanation may be consistent with the previous study suggested that advice from weak ties could be more likely to make people perceived potential risks of an event, which could result in more mental health symptoms,34 rather than potential benefits.46 Also, the reverse direction of associations from risk perception and social support to mental health is possible. Specifically, more depressive and PTSD symptoms could be the reason (instead of the result) for seeking more support or for having a higher perceived uncontrollability. Therefore, high support from others (the weak tie network members such as classmates or colleagues) that comes with more negative informational support may enhance the negative association between risk perception and psychological health.
Limitations and Implications
Some limitations should be discussed. First, this study is a cross-sectional data study design. More strong evidence from the longitudinal or experimental study should be employed further. Second, data were collected by a web-based survey, causing the sampling of our study was voluntary. Thus, there could be a selection bias. Third, convenience and quota sampling used in this study is a non-probability sampling technique, which could lead to selective biases. For example, the targeted recruitment of medical workers and relevant fields in the non-probability sampling process might make the current study biased. Therefore, we should be cautious to generalize the study findings to the overall population of China. Fourth, since our data was collected at the early phases of the COVID-19 outbreak, the findings could exit time-sensitive. Future studies can continue to monitor whether the moderating effects of social support have a long-term effect after the pandemic. Besides, due to the lack of data before the pandemic, it is difficult to judge whether the mental health symptoms estimated in this study, are a “reaction” to the pandemic or a pre-existing condition. Lastly, due to the geographic constraints, our results may be only applicable to the Chinese population. A recent study found that risk perception differed across countries due to socio-cultural differences across nations, so future research can focus on different countries’ risk perception and its relation with mental health.47
Despite its limitations, this study tells us some significant implications. On one hand, the perceived uncontrollability of risk seems to have a stronger correlation with depressive symptoms and PTSD symptoms than perceived severity. Therefore, politicians must adopt effective risk communication and mental health interventions. For example, the government could establish an emergency risk communication management system to help people to avoid or mitigate the negative impact of COVID-19 on their mental health by controlling risk perception levels, especially perceived controllability of risk.48 As to building reasonable risk perception, it is important to provide the public with authentic and accurate information and control the contagious disease outbreaks as soon as possible.49,50 On the other hand, social support should be paid more attention to when conducting psychological interventions. Providing appropriate social support from family and friends will help improve their mental health. It may provide individuals with a supportive environment, wherein individuals could alleviate or avoid mental health symptoms by sharing their feelings and emotions.51 Besides, the negative role of other support may suggest that the support from colleges or classmates could be negative informational support. Therefore, policy efforts could provide the public with more valid information support about COVID-19. Furthermore, according to the moderation effect of social support, although family and friend support is beneficial to mental health, excessive social support from family and friends may not buffer the adverse effect of risk perception on mental health symptoms. It could be accompanied by a sense of powerlessness.45 Based on this finding, it is imperative to control the quality and quantity of family and friend support in mental health intervention.52 Lastly, since people with higher support from weak tie relationship may receive more negative information about COVID-19, especially rumors, that could increase the risk perception and mental health symptoms, it is necessary for governments to notice the interpersonal communication in networks with a lot of weak ties, to enhance the public’s ability to identify the authenticity of crisis information and to provide real information to mitigate rumors that disseminate through the weak ties in particular.39
Conclusions
This study shows that perceived uncontrollability of COVID-19 risk appears to be more strongly associated with mental health symptoms, followed by perceived severity. Family and friends’ support negatively associates with the degree of depressive symptoms and PTSD symptoms, whereas other social support not. Moreover, high family and other social support could enhance the effects of perceived uncontrollability on mental health symptoms. These findings may have implications for risk communication and mental health promotion programs in future potential pandemics.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval
The study was approved by the Ethics Committee of Peking University Medical Center. Also, we confirm that this study was conducted in accordance with the Declaration of Helsinki.
Consent to Participate
All participants provided their online informed consent before proceeding with the questions. The informed consent documents, which contained the study’s purpose, anonymity, confidentiality, and participants’ right to withdraw at any time, were presented on the front page of the online questionnaire. Only after potential participants completely read the documents, and then click on a response button “Yes, I consent”, they could continue to fill in the questionnaire online. For subjects under 18 years old, parental informed consent has been obtained from the process that their parents shared the questionnaire link with them.
Acknowledgments
The authors wish to thank Farooq Ahmed and Muhammad Shahid for their work on careful edit and revision of this paper, and thanks to all those who helped to collect the data and those who kindly volunteered to participate in the study.
Funding
This study was supported by China National Social Science Foundation (20VYJ042).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi:10.1016/j.psychres.2020.112954
2. Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi:10.1016/j.psychres.2020.112921
3. Guo J, Feng XL, Wang XH, van IJzendoorn MH. Coping with COVID-19: exposure to covid-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int J Environ Res Public Health. 2020;17(11):1–18. doi:10.3390/ijerph17113857
4. Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–320. doi:10.1177/0020764020915212
5. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi:10.3390/ijerph17051729
6. Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. Dynamics of a stressful encounter. cognitive appraisal, coping, and encounter outcomes. J Pers Soc Psychol. 1986;50(5):992–1003. doi:10.1037/0022-3514.50.5.992
7. Imai H, Furukawa TA, Hayashi SU, et al. Risk perception, self-efficacy, trust for physician, depression, and behavior modification in diabetic patients. J Health Psychol. 2020;25(3):350–360. doi:10.1177/1359105317718057
8. Takebayashi Y, Lyamzina Y, Suzuki Y, Murakami M. Risk perception and anxiety regarding radiation after the 2011 Fukushima nuclear power plant accident: a systematic qualitative review. Int J Environ Res Public Health. 2017;14(11):1306. doi:10.3390/ijerph14111306
9. Imai H, Okumiya K, Fukutomi E, et al. Association between risk perception, subjective knowledge, and depression in community-dwelling elderly people in Japan. Psychiatry Res. 2015;227(1):27–31. doi:10.1016/j.psychres.2015.03.002
10. González-Sanguino C, Ausín B, Castellanos MÁ, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172–176. doi:10.1016/j.bbi.2020.05.040
11. Liu M, Zhang H, Huang H. Media exposure to COVID-19 information, risk perception, social and geographical proximity, and self-rated anxiety in China. BMC Public Health. 2020;20(1):1–8. doi:10.1186/s12889-020-09761-8
12. Suzuki Y, Yabe H, Yasumura S, et al. Détresse psychologique et perception des risques liés aux rayonnements: L’enquête de surveillance sanitaire Fukushima Health Management Survey. Bull World Health Organ. 2015;93(9):598–605. doi:10.2471/BLT.14.146498
13. Li J-B, Yang A, Dou K, Wang L-X, Zhang M-C, Lin X-Q. Chinese public’s knowledge, perceived severity, and perceived controllability of COVID-19 and their associations with emotional and behavioural reactions, social participation, and precautionary behaviour: a national survey; 2020. doi:10.21203/rs.3.rs-16572/v1
14. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi:10.1016/j.ajp.2020.102066
15. Hou T, Zhang T, Cai W, et al. Social support and mental health among health care workers during coronavirus disease 2019 outbreak: a moderated mediation model. PLoS One. 2020;15(5):e0233831. doi:10.1371/journal.pone.0233831
16. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. doi:10.1037/0033-2909.98.2.310
17. Schwarzer R, Knoll N. Functional roles of social support within the stress and coping process: a theoretical and empirical overview. Int J Psychiol. 2007;42(4):243–252. doi:10.1080/00207590701396641
18. Wu X, Zhou X, Wu M, Chen J, Zhao X. A longitudinal study on the effects of the level of trauma exposure and subjective fear on post-traumatic stress disorder (PTSD): the moderating effect of social support. Psychol Dev Educ. 2016;32(5):595–603. doi:10.16187/j.cnki.issn1001-4918.2016.05.10
19. Yeh YC, Ko HC, Wu JYW, Cheng CP. Gender differences in relationships of actual and virtual social support to internet addiction mediated through depressive symptoms among college students in Taiwan. Cyberpsychol Behav. 2008;11(4):485–487. doi:10.1089/cpb.2007.0134
20. Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013;35(2):121–126. doi:10.4103/0253-7176.116232
21. Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6(1):14–17. doi:10.29252/hrjbaq.5.1.49
22. Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi:10.1177/014662167700100306
23. Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. 2013;5(August):2002. doi:10.1037/t02622-000
24. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52(1):30–41. doi:10.1207/s15327752jpa5201_2
25. Xie X, Zheng R, Xie D, Wang H. Analysis on psychological panic phenomenon of SARS. Beijing Da Xue Xue Bao Yi Xue Ban. 2005;41(4):628–639.
26. Guo J, Fu M, Liu D, Zhang B, Wang X, van IJzendoorn MH. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110:104667. doi:10.1016/j.chiabu.2020.104667
27. Sun Q, Lu N. Social Capital and mental health among older adults living in urban China in the context of COVID-19 pandemic. Int J Environ Res Public Health. 2020;17(21):7947. doi:10.3390/ijerph17217947
28. Yildirim M, Arslan G, Özaslan A. Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: exploring the mediating effects of resilience and coronavirus fear; 2020. doi:10.31234/osf.io/84xju
29. Rundmo T, Nordfjærn T. Does risk perception really exist? Saf Sci. 2017;93:230–240. doi:10.1016/j.ssci.2016.12.014
30. Weinstein ND. Perceived probability, perceived severity, and health-protective behavior. Health Psychol. 2000;19(1):65–74. doi:10.1037/0278-6133.19.1.65
31. Satici B, Saricali M, Satici SA, Griffiths MD. Intolerance of Uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Int J Ment Health Addict. 2020. doi:10.1007/s11469-020-00305-0
32. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. doi:10.1016/j.ijantimicag.2020.105924
33. Bostean G, Andrade FCD, Viruell‐Fuentes EA. Neighborhood stressors and psychological distress among U.S. Latinos: measuring the protective effects of social support from family and friends. Stress Health. 2019;35(2):115–126. doi:10.1002/smi.2843
34. Liu X, Shao L, Zhang R, et al. Perceived social support and its impact on psychological status and quality of life of medical staffs after outbreak of SARS-CoV-2 Pneumonia: a Cross-Sectional Study. SSRN Electron J. 2020. doi:10.2139/ssrn.3541127
35. Mohd TAMT, Yunus RM, Hairi F, Hairi NN, Choo WY. Social support and depression among community dwelling older adults in Asia: a systematic review. BMJ Open. 2019;9(7):e026667. doi:10.1136/bmjopen-2018-026667
36. Katz JP. Networks in the Knowledge Economy. Oxford University Press; Vol. 17. 2011. doi:10.5465/ame.2003.11854693
37. Granovetter M. The strength of weak ties: a network theory revisited. Sociol Theory. 1983;1:201–233. doi:10.2307/202051
38. Griffiths KM, Crisp DA, Barney L, Reid R. Seeking help for depression from family and friends: a qualitative analysis of perceived advantages and disadvantages. BMC Psychiatry. 2011;11(1). doi:10.1186/1471-244X-11-196
39. Wei J, Bu B, Guo X, Gollagher M. The process of crisis information dissemination: impacts of the strength of ties in social networks. Kybernetes. 2014;43(2):178–191. doi:10.1108/K-03-2013-0043
40. Liu T, Zhang H, Zhang H. The impact of social media on risk communication of disasters — a comparative study based on Sina Weibo blogs related to Tianjin Explosion and Typhoon Pigeon. Int J Environ Res Public Health. 2020;17(3):883. doi:10.3390/ijerph17030883
41. Okabayashi H, Krause N, Akiyama H. Mental health among older adults in Japan: do sources of social support and negative interaction make a difference? Social Science & Medicine (1982). 2004;59(11):2259–2270. doi:10.1016/j.socscimed.2004.02.024
42. Lee RPL, Ruan D, Lai G. Social structure and support networks in Beijing and Hong Kong. Soc Netw. 2005;27(April 2001):249–274. doi:10.1016/j.socnet.2005.04.001
43. Hobman EV, Restubog SLD, Bordia P, Tang RL. Abusive supervision in advising relationships: investigating the role of social support. Appl Psychol. 2009;58(2):233–256. doi:10.1111/j.1464-0597.2008.00330.x
44. Nahum-Shani I, Bamberger PA. Explaining the variable effects of social support on work-based stressor-strain relations: the role of perceived pattern of support exchange. Organ Behav Hum Decis Process. 2011;114(1):49–63. doi:10.1016/j.obhdp.2010.09.002
45. Bolger N, Amarel D. Effects of social support visibility on adjustment to stress: experimental evidence. J Pers Soc Psychol. 2007;92(3):458–475. doi:10.1037/0022-3514.92.3.458
46. Weenig MWH, Midden CJH. Communication network influences on information diffusion and persuasion. J Pers Soc Psychol. 1991;61(5):734–742. doi:10.1037/0022-3514.61.5.734
47. Dryhurst S, Schneider CR, Kerr J, et al. Risk perceptions of COVID-19 around the world. J Risk Res. 2020;23(7–8):994–1006. doi:10.1080/13669877.2020.1758193
48. Xu J, Dai J, Rao R, Xie H. The association between exposure and psychological health in earthquake survivors from the Longmen Shan Fault area: the mediating effect of risk perception. BMC Public Health. 2016;16(1). doi:10.1186/s12889-016-2999-8
49. Qian M, Wu Q, Wu P, et al. Psychological responses, behavioral changes and public perceptions during the early phase of the COVID-19 outbreak in China: a population based cross-sectional survey. MedRxiv. 2020. doi:10.1101/2020.02.18.20024448
50. Zhang L, Li H, Chen K. Effective risk communication for public health emergency: reflection on the COVID-19 (2019-nCoV) outbreak in Wuhan, China. Healthcare. 2020;Vol 8(1):64. doi:10.3390/healthcare8010064
51. Zhou X, Wu X, Zhen R. Understanding the relationship between social support and posttraumatic stress disorder/posttraumatic growth among adolescents after Ya’an earthquake: the role of emotion regulation. Psychol Trauma. 2017;9(2):214–221. doi:10.1037/tra0000213
52. Shang F, Kaniasty K, Cowlishaw S, Wade D, Ma H, Forbes D. The impact of received social support on posttraumatic growth after disaster: the importance of both support quantity and quality. Psychol Trauma. 2020. doi:10.1037/tra0000541
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
