Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Relationship between plasma matrix metalloproteinase levels, pulmonary function, bronchodilator response, and emphysema severity
Authors Koo H, Hong Y, Lim MN, Yim J, Kim WJ
Received 28 December 2015
Accepted for publication 19 February 2016
Published 27 May 2016 Volume 2016:11(1) Pages 1129—1137
DOI https://doi.org/10.2147/COPD.S103281
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Hyeon-Kyoung Koo,1 Yoonki Hong,2 Myoung Nam Lim,2 Jae-Joon Yim,3 Woo Jin Kim2
1Department of Internal Medicine, Division of Pulmonary and Critical Medicine, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, 2Department of Internal Medicine and Environmental Health Center, Kangwon National University, Chuncheon-si, 3Department of Internal Medicine and Lung Institute, Division of Pulmonary and Critical Care Medicine, Seoul National University College of Medicine, Seoul, Republic of Korea
Objective: Chronic obstructive pulmonary disease (COPD) is characterized by chronic inflammation in the airway and lung. A protease–antiprotease imbalance has been suggested as a possible pathogenic mechanism for COPD. We evaluated the relationship between matrix metalloproteinase (MMP) levels and COPD severity.
Methods: Plasma levels of MMP-1, MMP-8, MMP-9, and MMP-12 were measured in 57 COPD patients and 36 normal controls. The relationship between MMP levels and lung function, emphysema index, bronchial wall thickness, pulmonary artery pressure, and quality of life was examined using general linear regression analyses.
Results: There were significant associations of MMP-1 with bronchodilator reversibility and of MMP-8 and MMP-9 with lung function. Also, MMP-1, MMP-8, and MMP-9 levels were correlated with the emphysema index, independent of lung function. However, MMP-12 was not associated with lung function or emphysema severity. Associations between MMP levels and bronchial wall thickness, pulmonary artery pressure, and quality of life were not statistically significant.
Conclusion: Plasma levels of MMP-1, MMP-8, and MMP-9 are associated with COPD severity and can be used as a biomarker to better understand the characteristics of COPD patients.
Keywords: matrix metalloproteinase, pulmonary disease, chronic obstructive, respiratory function test, pulmonary emphysema, bronchodilator response
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by persistent airflow limitation associated with both small airway inflammation (obstructive bronchiolitis) and parenchymal destruction (emphysema).1 One of the proposed hypotheses for COPD pathogenesis is a protease–antiprotease imbalance after observation of emphysema development in alpha-1 antitrypsin deficiency.2 Matrix metalloproteinases (MMPs) are a family of structurally related metalloendopeptidases and are crucial for extracellular matrix remodeling following tissue damage. Both animal and human studies have shown that several MMPs are elevated in sputum, bronchoalveolar lavage (BAL), and lung tissue specimens from animals and patients with COPD.3–9 However, it should be noted that there were some inconsistencies between animal and human data.10–12 It is known that MMPs are activated by various different stimuli, including cigarette smoking and oxidative stress.13–15 The aim of the current study was to determine whether plasma MMP levels, especially MMP-1, MMP-8, MMP-9, and MMP-12, are correlated with COPD disease activity, as measured with pulmonary function, emphysema severity, pulmonary artery (PA) pressure, and quality of life using data of Chronic Obstructive Pulmonary Disease in Dusty Areas Near Cement Plants (CODA) cohort.
Methods
Study design and participants
The CODA cohort was initially started from a health survey to identify the health effects associated with cement dust and has been supported by the National Institute of Environment Research of the Ministry since 2007. The CODA cohort is made up of both normal controls and subjects who have airflow limitation, as confirmed with a spirometer. Airflow limitation is defined as the post-bronchodilator forced expiratory volume in 1 second (FEV1) over forced vital capacity (FVC) value (FEV1/FVC) of <0.7.1 Recruitment into the CODA cohort is ongoing and subjects will be followed for more than 10 years. The design of the CODA study had been previously described in detail.16 Briefly, the CODA study is an observational, longitudinal study in which subjects undergo medical interviews, physical examinations, spirometer with bronchodilator reversibility testing, laboratory testing, and computed tomography (CT) scanning. All CODA study conduct adheres to Good Clinical Practice Guidelines and the tenets of the Declaration of Helsinki. It has been approved by the ethics institutional review boards of participating centers (Institutional Review Board of Kangwon National University Hospital (KNUH) 2012-06-007). The current study has also been approved by the ethics institutional review boards (KNUH-KBB-2013-005). All participants provided written informed consent.
Clinical, laboratory, and quality of life measures
The methods used in the CODA study have been described in detail elsewhere.16 Initial questionnaire data included demographic characteristics and respiratory symptoms. Dyspnea was evaluated using the modified Medical Research Council dyspnea scale. Health-related quality of life was evaluated by calculating the total score of the patient-reported COPD assessment test (CAT). Volumetric CT scan measurements were based on the protocol used in the Korean Obstructive Lung Disease study and were obtained from 16-multidetector CT scanner (Somatom Sensation 16; Siemens Medical Systems, Bonn, Germany).17 The emphysema index, defined as the percentage of low attenuation area ≤950 Hounsfield units (HU, %LAA-950HU), and airway thickening (mean wall area [MWA] percentage of two segmental bronchi) were measured using an in-house software from the Korean Obstructive Lung Disease study group to assess COPD quantitatively.17–19 Airway dimensions were measured near the origin of the right apical and left apico-posterior segmental bronchi that were selected by a consensus reading of two radiologists. PA pressure was represented by the PA/ascending aorta (A) diameter ratio.20 Spirometry was performed using an EasyOne Kit (NDD, Zurich, Switzerland). Bronchodilator reversibility was evaluated by assessing the change in FVC or FEV1 (in liters) following bronchodilator administration. All pulmonary function tests were performed following the recommendations of the American Thoracic Society and the European Respiratory Society.21 Serum, plasma, and urine samples were collected for biomarker and genetic/proteomic analyses. Concentrations of plasma MMP-1, MMP-8, MMP-9, and MMP-12 were measured using commercially available enzyme-linked immunosorbent assay kits (R&D Systems, Inc., Minneapolis, MN, USA) according to manufacturer’s instructions. The detection limits of MMP-1, MMP-8, MMP-9, and MMP-12 were 0.063 ng/mL, 0.0125 ng/mL, 0.011 ng/mL, and 0.0019 pg/mL, respectively.
Statistical analyses
Data are expressed as mean ± standard deviation, median values (interquartile range), and frequency distribution (%), as appropriate. For between-group comparisons, Student’s t-tests or analyses of variance were used to compare continuous variables and chi-square tests were used to compare categorical variables. Associations between variables were examined using Pearson’s correlation coefficient (r). Multivariate analyses were performed using general linear regression. Data were analyzed using Statistical Analysis Software (Version 9.3; SAS Institute Inc., Cary, NC, USA) for Windows. Statistical significance was defined as P<0.05 (two-sided P-values examined).
Results
Subject characteristics
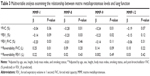
A total of 93 subjects were included in our analyses, with 57 and 36 subjects in the COPD and healthy control groups, respectively. Nine subjects (25%) in the control group and 19 subjects (33.3%) in the COPD group were current smokers. Clinical and laboratory characteristics of our study population are summarized in Table 1. Plasma levels of MMP-1, MMP-8, MMP-9, and MMP-12 were not significantly different between the control and COPD groups. Because smoking is known to affect both COPD and MMP levels, the relationship between smoking status and MMP levels was evaluated. Smoking led to a significant increase in MMP-12 levels (P=0.045), but not in MMP-1 (P=0.43), MMP-8 (P=0.29), or MMP-9 (P=0.35) levels. Table 2 shows how the study population was stratified based upon smoking status. In the control group, MMP-12 levels were significantly higher in current smokers (P=0.01) than in subjects who had never smoked (P for trend =0.01). Also, MMP-8 increased with smoking status (P for trend =0.02). In the COPD group, MMP-8 and MMP-9 levels were higher in former smokers than in subjects who had never smoked, but no significant difference was identified in current smokers. Significant correlations were found between plasma MMP-8 and MMP-9 levels (r=0.76, P<0.001), MMP-8 and MMP-12 levels (r=0.53, P<0.001), and MMP-9 and MMP-12 levels (r=0.71, P<0.001) (Figure S1). The MMP-8, MMP-9, and MMP-12 levels were also positively correlated with peripheral white blood cell (WBC) count (Figure 1).
  | Figure 1 Correlation between MMP levels and WBC count as determined by linear regression analyses. |
MMP levels, lung function, and quality of life
The relationships between MMP levels and lung function were evaluated. Levels of MMP-1 were not significantly associated with FVC (P=0.72), FEV1 (P=0.18), or FEV1/FVC (P=0.06). Similarly, MMP-12 had no relationship with FVC (P=0.14), FEV1 (P=0.22), and FEV1/FVC (P=0.62). However, levels of MMP-8 (r=−0.28, P=0.01) and MMP-9 (r=−0.23, P=0.03) were negatively correlated with FVC, and levels of MMP-9 were inversely correlated with FEV1 (r=−0.24, P=0.03). The relationships between MMP levels and bronchodilator reversibility were also evaluated. Levels of MMP-1 were positively correlated with FVC (L) reversibility (r=0.25, P=0.02) (Figure 2). However, CAT score for quality of life was not correlated with any MMP level examined (MMP-1: P=0.13, MMP-8: P=0.58, MMP-9: P=0.73, and MMP-12: P=0.20).
Correlations between MMP levels and lung function were adjusted for age, sex, height, body mass index (BMI), and smoking status for the multivariate analysis. Both FVC and FEV1 were negatively correlated with MMP-8 and MMP-9 levels, but not with MMP-1 and MMP-12 levels (Table 3). A separate multivariate analysis was performed, in which FVC and FEV1 reversibility were adjusted for age, sex, height, BMI, smoking status, and post-bronchodilator FVC or FEV1, respectively. Both FVC reversibility (β=0.25, P=0.01) and FEV1 reversibility (β=0.22, P=0.02) were independently associated with MMP-1 levels, but not with MMP-8, MMP-9, or MMP-12 levels (Table 3). Another multivariate analysis was performed to examine the association between CAT score and MMP levels after adjusting the CAT score for age, sex, BMI, smoking status, and COPD stage. This revealed that none of the MMP levels examined were significantly correlated with the CAT score (MMP-1, P=0.06; MMP-8, P=0.29; MMP-9, P=0.37; and MMP-12, P=0.10).
Emphysema index, percent MWA, and pulmonary hypertension
The emphysema index (%LAA-950HU) was 3.19±3.91 in the control group and 9.23±8.07 in the COPD group (P<0.001). The relationships between the emphysema index and MMP levels were preliminarily evaluated with univariate analyses. The emphysema index was positively correlated with both MMP-8 and MMP-9 levels in COPD patients (Figure 3). Multivariate analysis examining the relationships between the emphysema index and MMP levels was performed after adjusting for age, sex, height, BMI, smoking status, FVC (% predicted), and FEV1 (% predicted). Only MMP-1 was independently associated with the emphysema index (model 1 in Table 4). Because WBC count and MMP levels were correlated with each other (Figure 1), the WBC count was added to a previous model. After additional adjustment (model 2 in Table 4), the emphysema index was independently associated with MMP-1 (β=0.18, P=0.048), MMP-8 (β=0.19, P=0.045), and MMP-9 (β=0.21, P=0.03), but not with MMP-12 (P=0.39).
The percent MWA was 69.8%±0.5% in the control group and 70.4%±4.3% in the COPD group (P=0.55). The PA/A ratio, as measured by CT scan, was 0.59±0.09 in the control group and 0.79±0.11 in the COPD group (P=0.92). Univariate analyses showed that the percent MWA was not associated with MMP-1 (P=0.88), MMP-8 (P=0.60), MMP-9 (P=0.60), or MMP-12 (P=0.62). The PA/A ratio was also not significantly associated with any MMP level examined (MMP-1, P=0.40; MMP-8, P=0.30; MMP-9, P=0.46; and MMP-12, P=0.83). Multivariate analyses were performed for both percent MWA and PA/A ratio, but neither parameter was significantly correlated with any MMP level examined (Table 4).
Airflow limitation and emphysema status
Small airway inflammation and parenchymal destruction characterize COPD.1 Therefore, we stratified COPD patients into the following four groups depending upon the presence of airflow limitation (FEV1 ≤80%) and emphysema (%LAA-950HU ≥5): absence of airflow limitation and emphysema (O-E-), absence of airflow limitation and presence of emphysema (O-E+), presence of airflow limitation and absence of emphysema (O+E-), and presence of airflow limitation and emphysema (O+E+). The clinical characteristics of each of the four subgroups are summarized in Table 5. Interestingly, MMP levels were not significantly different between the four subgroups.
Discussion
In this study, plasma levels of MMP-8 and MMP-9 were associated with FVC and FEV1. Values of MMP-1 were correlated with bronchodilator reversibility. Furthermore, MMP-1, MMP-8, and MMP-9 levels were related to emphysema index, independent of pulmonary function. However, MMP-12 was not associated with lung function or the emphysema index.
The MMPs are proteolytic enzymes that degrade matrix components and are known to play roles in initiating and maintaining inflammation after cigarette smoke exposure. Earlier studies have extensively investigated MMP-12. In an animal study, cigarette smoke exposure upregulated MMP-12 production and MMP-12 knockout mice were protected against smoke-induced emphysema.6 Unfortunately, the results of human studies varied and how smoking affects MMP-12 levels remains controversial. Ilumets et al9 found that MMP-12 levels were higher in the sputum of stage 0 smokers than in nonsmokers. Also, Montaño et al22 reported that MMP-12 activity is increased in macrophages from BAL fluid of COPD patients. However, Finlay et al10 found that MMP-12 mRNA levels were not significantly different in alveolar macrophages of emphysematous and healthy lungs. In addition, Lee et al12 found that single-nucleotide polymorphisms in MMP-12 are not associated with COPD frequency in the Korean population. Studies on MMP-9 have shown that this MMP is elevated in the sputum8 and serum of patients with COPD. Also, MMP-9 levels and lung function were found to be correlated in both COPD patients23 and the general population.24 Associations between MMP-9 and both lung function decline25 and COPD exacerbation26 have also been reported. However, D’Armiento et al27 did not find a significant correlation between MMP-9 and emphysema severity. The literature on MMP-1 and MMP-8 levels is sparse, but elevated MMP-1 levels have been reported in COPD patients and were recently shown to be correlated with lung function.23 Although an MMP-8 elevation has been observed in BAL fluid from patients with subclinical emphysema,28 correlations between MMP-8 and CT lung density and between MMP-8 levels and pulmonary function have not been found.27
Our findings suggest a role of several MMPs in COPD pathogenesis. Our most striking findings were the correlations between MMP-1, MMP-8, and MMP-9 with the emphysema index and between MMP-1 and bronchodilator reversibility. Several MMPs have been previously shown to be elevated in COPD patients and related to poor lung function. However, this study is the first to find independent correlations between MMP-1, MMP-8, and MMP-9 and emphysema severity. Furthermore, the association of MMP-1 with bronchodilator reversibility has not been previously reported. Therefore, MMP-1 might be important in understanding frequent exacerbation with airway hyperresponsiveness. The role of MMP-8 in the pathogenesis of idiopathic pulmonary fibrosis has been studied more than that in COPD.29–31 However, we found that MMP-8 levels were significantly correlated with both lung function and emphysema severity. Further studies are needed to verify and clarify the role of MMP-8 in COPD pathogenesis. We found an association between MMP-9 levels and lung function, as previously shown by others,23,24 but also found a significant correlation between MMP-9 levels and emphysema severity. In agreement with earlier studies, we did not observe a significant relationship between MMP-12 levels and pulmonary function or emphysema severity.
Differences in plasma MMP levels between patients with and without COPD were not observed in the present study. This suggests that MMP levels may be elevated in patients with conditions other than COPD. Though MMPs would not be suitable biomarkers for diagnosing COPD, they may be useful for predicting COPD activity and patient prognosis.
This study had several limitations. First, we could not control the influence of cement dust on subjects because we used data obtained from the CODA cohort. The influence of cement dust on MMPs has not been documented, but we could not control the exact amount of dust that each patient was exposed to. Therefore, differences in dust exposure may have confounded our results. Second, only baseline blood samples were analyzed and we were not able to evaluate changes in MMP levels during the follow-up period. Third, we could not control the effects of medications such as statins or anti-inflammatory drugs. Fourth, PA pressure can be measured more accurately by cross-sectional area <5 mm2 (%CSA<5),32 which might reveal greater relevance to the association between level of MMP and severity of PA pressure. Fifth, we were unable to obtain appropriate data to make an association between MMP levels and COPD exacerbation because only a small number of patients had worsening disease during the relatively short follow-up period. Further studies evaluating the association between the annual lung function decline rate, COPD exacerbation, functional capacity, and mortality are needed to confirm our findings.
In conclusion, elevated MMP-8 and MMP-9 levels were associated with poor pulmonary function, and MMP-1 was correlated with the bronchodilator response. Furthermore, emphysema severity was correlated with MMP-1, MMP-8, and MMP-9 (not MMP-12), independent of lung function. Therefore, MMP-1, MMP-8, and MMP-9 may be powerful biomarkers in COPD patients. The roles of MMPs should be further studied to improve our understanding of COPD pathogenesis and progression.
Disclosure
This study was supported by grants from the Environmental Health Center funded by the Ministry of Environment, Republic of Korea. The authors report no other conflicts of interest in this work.
References
Roisin RR (2011) Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease; 2015. Available from: http://www.goldcopd.org. Accessed December, 2014. | ||
Laurell CB, Erickson S. The electrophoretic alpha-1 globulin pattern of serum in alpha-1 antitrypsin deficiency. Scand J Clin Lab Invest. 1963;15:132–140. | ||
Hautamaki R, Kobayashi DK, Senior RM, Shapiro S. Requirement for macrophage elastase for cigarette smoke-induced emphysema in mice. Science. 1997;277:2002–2004. | ||
Lanone S, Zheng T, Zhu Z, et al. Overlapping and enzyme specific contributions of matrix metalloproteinases-9 and -12 in IL-13-induced inflammation and remodelling. J Clin Invest. 2002;110:463–474. | ||
Prause O, Bozinovski S, Anderson GP, Lindén A. Increased matrix metalloproteinase-9 concentration and activity after stimulation with interleukin-17 in mouse airways. Thorax. 2004;59:313–317. | ||
Vlahos R, Bozinovski S, Chan SP, et al. Neutralizing granulocyte/macrophage colony-stimulating factor inhibits cigarette smoke-induced lung inflammation. Am J Respir Crit Care Med. 2010;182:34–40. | ||
Imai K, Dalal SS, Chen ES, et al. Human collagenase (matrix metalloproteinase-1) expression in the lungs of patients with emphysema. Am J Respir Crit Care Med. 2001;163:786–791. | ||
Beeh KM, Beier J, Kornmann O, Buhl R. Sputum matrix metalloproteinase-9, tissue inhibitor of metalloprotinease-1, and their molar ratio in patients with chronic obstructive pulmonary disease, idiopathic pulmonary fibrosis and healthy subjects. Respir Med. 2003;97:634–639. | ||
Ilumets H, Rytila P, Demedts L, et al. Matrix metalloproteinases-8, -9, and -12 in smokers and patients with stage 0 COPD. Int J Chron Obstruct Pulmon Dis. 2007;2:369–379. | ||
Finlay G, Russell KJ, McMahon KJ. Elevated levels of MMPs in BAL fluid of emphysematous patients. Thorax. 1997;52:502–506. | ||
Gosselink JV, Hayashi S, Elliott WM, et al. Differential expression of tissue repair genes in the pathogenesis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;181:1329–1335. | ||
Lee SY, Kim MJ, Kang HG, et al. Polymorphisms in matrix metalloproteinase-1, -9 and -12 genes and the risk of chronic obstructive pulmonary disease in a Korean population. Respiration. 2010;80:133–138. | ||
Nelson KK, Melendez JA. Mitochondrial redox control of matrix metalloproteinases. Free Radic Biol Med. 2004;37:768–784. | ||
Kinnula VL. Focus on antioxidant enzymes and antioxidant strategies in smoking related airway diseases. Thorax. 2005;60:693–700. | ||
Kinnula VL, Fattman CL, Tan RJ, Oury TD. Oxidative stress in pulmonary fibrosis: a possible role for redox modulatory therapy. Am J Respir Crit Care Med. 2005;172:417–422. | ||
Hong Y, Kwon JW, Lee SA, et al. Methodology of an observational cohort study for subjects with chronic obstructive pulmonary disease in dusty areas near cement plants. J Pulm Respir Med. 2014;4(1):169. | ||
Lee YK, Oh YM, Lee JH, et al. Quantitative assessment of emphysema, air trapping, and airway thickening on computed tomography. Lung. 2008;186:157–165. | ||
Gevenois PA, De Vuyst P, de Maertelaer V, et al. Comparison of computed density and microscopic morphometry in pulmonary emphysema. Am J Respir Crit Care Med. 1996;154:187–192. | ||
Wang Z, Gu S, Leader JK, et al. Optimal threshold in CT quantification of emphysema. Eur Radiol. 2013;23:975–984. | ||
Iyer AS, Wells JM, Vishin S, Bhatt SP, Wille KM, Dransfield MT. CT scan-measured pulmonary artery to aorta ratio and echocardiography for detecting pulmonary hypertension in severe COPD. Chest. 2014;145(4):824–832. | ||
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. | ||
Montaño M, Beccerril C, Ruiz V, Ramos C, Sansores RH, González-Avila G. Matrix metalloproteinases activity in COPD associated with wood smoke. Chest. 2004;125(2):466–472. | ||
Montaño M, Sansores RH, Becerril C, et al. FEV1 inversely correlates with metalloproteinases 1, 7, 9 and CRP in COPD by biomass smoke exposure. Respir Res. 2014;15:74. | ||
Olafsdóttir IS, Janson C, Lind L, Hulthe J, Gunnbjörnsdóttir M, Sundström J. Serum levels of matrix metalloproteinase-9, tissue inhibitors of metalloproteinase-1 and their ratio are associated with impaired lung function in the elderly: a population-based study. Respirology. 2010;15(3):530–535. | ||
Higashimoto Y, Iwata T, Okada M, Satoh H, Fukuda K, Tohda Y. Serum biomarkers as predictors of lung function decline in chronic obstructive pulmonary disease. Respir Med. 2009;103(8):1231–1238. | ||
Omachi TA, Eisner MD, Rames A, Markovtsova L, Blanc PD. Matrix metalloproteinase-9 predicts pulmonary status declines in a1-antitrypsin deficiency. Respir Res. 2011;12:35. | ||
D’Armiento JM, Goldklang MP, Hardigan AA, et al. Increased matrix metalloproteinase (MMPs) levels do not predict disease severity or progression in emphysema. PLoS One. 2013;8(2):e56352. | ||
Betsuyaku T, Nishimura M, Takeyabu K, et al. Neutrophil granule proteins in bronchoalveolar lavage fluid from subjects with subclinical emphysema. Am J Respir Crit Care Med. 1999;159(6):1985–1991. | ||
Craig VJ, Zhang L, Hagood JS, Owen CA. Matrix metalloproteinases as therapeutic targets for idiopathic pulmonary fibrosis. Am J Respir Cell Mol Biol. 2015;53(5):585–600. | ||
Craig VJ, Quintero PA, Fyfe SE, et al. Profibrotic activities for matrix metalloproteinase-8 during bleomycin-mediated lung injury. J Immunol. 2013;190(8):4283–4296. | ||
Dancer RC, Wood AM, Thickett DR. Metalloproteinases in idiopathic pulmonary fibrosis. Eur Respir J. 2011;38(6):1461–1467. | ||
Matsuoka S, Washko GR, Yamashiro T, et al. Pulmonary hypertension and computed tomography measurement of small pulmonary vessels in severe emphysema. Am J Respir Crit Care Med. 2010;181(3):218–225. |
Supplementary material
  | Figure S1 Correlations between the various MMP levels examined as determined by linear regression analyses. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.