Back to Journals » Clinical Interventions in Aging » Volume 13
Relationship between clinical outcomes and Dutch frailty score among elderly patients who underwent surgery for hip fracture
Authors Winters AM , Hartog LC, Roijen HIF, Brohet RM, Kamper AM
Received 26 July 2018
Accepted for publication 15 September 2018
Published 5 December 2018 Volume 2018:13 Pages 2481—2486
DOI https://doi.org/10.2147/CIA.S181497
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
AM Winters,1 LC Hartog,2 HIF Roijen,1 RM Brohet,3 AM Kamper1
1Department of Geriatrics, Isala, 8025 AB, Zwolle, the Netherlands; 2Diabetes Centre, Isala, 8025 AB, Zwolle, the Netherlands; 3Isala Academy, 8025 BP, Zwolle, the Netherlands
Background: Frailty is a geriatric condition that is associated with an increased risk of mortality and functional decline. To date, mainly the Groningen Frailty Indicator (GFI) and Hospital Safety Management (VeiligheidsManagementSysteem [VMS]) frailty score are used to determine frailty in several hospitals in the Netherlands. However, it is yet unknown, which method has the best predictive value on clinical outcomes.
Objective: The aim of this study was to investigate the predictive value of GFI and VMS on clinical outcomes among patients who underwent hip fracture surgery.
Design: This is a prospective observational cohort study.
Methods: We selected all patients aged 70 years or higher, who underwent hip fracture surgery in our general hospital, between November 2014 and November 2015. Among all patients, VMS, GFI and Barthel-20 index (BI) were assessed. McNemar’s paired test and Cohen’s κ were used to examine the difference and the level of agreement between the two scoring methods. Kaplan–Meier and multivariable regression analyses were performed to determine overall survival and mortality, respectively, 3 years and 30 days after surgery.
Results: A total of 280 patients were included in the study. The median follow-up was 25 months. No systematic difference was found between the two methods (P=0.237), while a fair level of agreement could be measured (κ=0.363 [95% CI =0.23–50]). VMS showed a statistically significant difference in overall survival as compared to nonfrail patients (57 vs 80%, respectively [Plogrank <0.001] with an HR of 3.5 [95% CI =2.1–5.7; P<0.001]). Classification according to GFI yielded a lower but still significant HR 2.3 (95% CI =1.2–4.1; P=0.008).
Conclusion: VMS can be used in classifying frailty, whereby VMS frailty score is associated with clinical outcomes as overall survival mortality in older patients with hip fracture and who underwent surgery.
Keywords: orthopedic surgery, frailty assessment, geriatric patients, mortality, functional decline
Introduction
The number of elderly people is rising in the Netherlands, from 2.9 million people aged above 65 years in 2017 to 4.8 million in 2040.1 Hip fractures are a leading cause of morbidity and mortality in elderly, an incidence of 18,000 patients above the age of 50 years in the Netherlands has been described.2 Among others, the overall outcome of hip fracture patients reflects the prefracture condition of the patient and is a summation of many factors. Identification of these factors can be used to identify patients who are frailer and might need a different approach during and after hospital stay. Frailty is a geriatric condition characterized by an increase in vulnerability to external stressors3,4 and has shown to be predictive for adverse postoperative outcomes in patients with hip fracture.5,6
In the Netherlands, a proven feasible, valid, and reliable instrument for measuring frailty is the Groningen Frailty Indicator (GFI).7,8 The internal consistency is 0.68–0.81. The GFI consists of 15 questions to determine the level of frailty; it establishes physical, cognitive, social, and psychological impairments and gives a score at a scale of 0–15. A GFI score of 4 or higher suggests frailty.9 An alternative for scoring frailty in the Netherlands is the Hospital Safety Management (VeiligheidsManagementSysteem [VMS]) frailty score.10 VMS was based on the following three questions: one about cognitive impairment or confusion during earlier admissions, one about falls in the last 6 months, and one question about physical impairments.10 When falling and another question scored yes, frailty was assumed. It is already known that VMS frailty score is correlated with mortality.11 To our knowledge, no previous studies investigated the predictive value of the GFI and VMS frailty scores on 30-day mortality or functional decline in patients with hip fracture. We performed a study in which we aimed to investigate the predictive value on adverse outcome of the GFI and VMS frailty scores in older patients with hip fracture and who underwent surgery.
Methods
Study population
This prospective observational cohort study was performed in a general hospital. All patients at the age of 70 years or older, who were admitted to our hospital with a primary proximal hip fracture and underwent surgery, were recruited. Recruitment and data collection were carried out between November 2014 and December 2015. Exclusion criteria were fractures distal from subtrochanteric fracture, periprosthetic fractures, pathological fractures, and admission to another department than the orthopedics/surgical or internal medicine/geriatric department.
Data collection
Baseline data involved demographic characteristics, multimorbidity, medication use, nutritional status, functional status, surgical treatment, anesthesia technique, delirium during admission, date of admission, and date of surgery. Delirium was considered to be present, when delirium was reported by a member of the geriatric team or when the Delirium Observation Screening (DOS) scores were at least three times above three and were fluctuating during the day.12 Data of mortality were collected from the municipality population register at one point after about 3 years after surgery. Morbidities were classified into the following five categories: diabetes mellitus, cardiovascular disease (heart disease, cerebrovascular accident, transient ischemic attack, renal failure, or hypertension), neurodegenerative disease (dementia and Parkinson’s disease), chronic obstructive pulmonary disease (COPD; asthma, or fibrosis), and cancer. We combined medication with identical ATC3 codes, with polypharmacy defined as the use of five or more prescriptions with different ATC3 codes at admission.
Frailty was determined with two instruments, such as the GFI and the VMS, at admission or within 24 hours after admission.
Nutritional status was determined with the Short Nutritional Assessment Questionnaire (SNAQ). A SNAQ score of two or more is assumed to be related to a moderate-to-severe risk of malnourishment.13 Daily living activities were measured with the Barthel-20 index (BI),14 at the day of admission to evaluate prefracture functional status. Degree of functional status change was based on assessing the difference in BI scores between baseline and 2 months after surgery.
All tests were part of the usual clinical care. Four trained medical staff members performed all tests to reduce interobserver disagreement. It was intended that all tests on a patient were taken by one and the same medical staff member.
Statistical analyses
Descriptive statistics was used to describe the baseline characteristics of the population and the outcome variables. Because of the lack of a golden standard to use as a reference, no sensitivity and specificity analyses were performed. McNemar’s paired test was used to determine whether there was a systematic difference between the two frailty scoring methods. Cohen’s κ was used to measure the level of agreement between the two methods. Univariate analyses were performed with the Pearson chi-squared or Fisher’s exact tests for dichotomous variables and the parametric independent t-test or nonparametric Mann–Whitney U test for continuous variables. Spearman and Pearson correlations were used to determine the correlation between the potential independent variables. In a multivariate logistic regression model, the predictive value of the frailty scoring methods and other patient characteristics on functional decline and mortality was determined. Stepwise regression analyses were performed to determine potential independent predictive variables for mortality and survival. These included logistic regression to examine 30-day mortality and Cox regression to examine overall survival as clinical outcome. Kaplan–Meier analysis was used to examine the difference in overall survival between frail and nonfrail patients classified by VMS and GFI. Potential confounders were age in two groups, smoking, gender, classification of frail by GFI or VMS, malignancy, and multimorbidity at baseline, such as chronic pulmonary diseases, cardiovascular disease, and living in a nursing home. Receiver operating characteristic curve analysis was not performed, since this would only consider the occurrence of events and not time to event. A P-value of <0.05 was considered as statistically significant. SPSS (Version 24) was used for the analysis.
Ethical approval
The study protocol was approved by the local medical ethics committee (Medisch Ethische Toetsingscommissie, Zwolle; study number 14.0110). Written informed consent was obtained from all patients by the participating medical doctor or nurse. All data were analyzed anonymously. The study protocol was registered prior to the start of the study at trailregister.nl (NTR5058). The “Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) statement was used to describe this observational cohort study.15
Results
A total of 286 patients were included in the study. The median follow-up was 25 months. The characteristics are presented in Table 1. The mean age was 83 years, and 75% of the patients were female. Prevalence of delirium during admission was 21%, 9% of the patients died within 30 days after surgery, and 26% of the patients died within 1 year after surgery. Multimorbidity, polypharmacy, and living in a nursing home before admission were associated with an increased 1-year mortality risk.
Frailty
A total of 277 patients completed the VMS, and 189 patients completed the GFI. Both tests were completed by 185 patients. A total of 76 (41%) patients were identified as frail according to both instruments, whereas 51 (28%) patients were identified as nonfrail in both instruments. A total of 24 patients scored frail in the VMS and not in the GFI, and 34 patients scored frail in the GFI and not in the VMS. Paired analysis showed that there was no difference between the two diagnostic tools (P=0.237) in addition to a fair level of agreement (κ=0.363 [95% CI =0.23–50]). In the group patients without GFI scores, fewer patients stayed in a nursing home before admission (9 vs 22%) and fewer patients were known with neurodegenerative disease (17 vs 44%). Other variables were comparable. An increase in positive answers on the VMS questionnaire was associated with an increase in mortality, polypharmacy, malnutrition, and living in a nursing home before admission.
Functional decline
For 62% of all patients, the BI scores were assessed at two moments. In 8% of the patients, functional decline was found (Table 1). The mean age of the patients with functional decline was 86 years, of whom 86% was female. The prevalence of frailty was 68 and 71% according to VMS frailty score and GFI, respectively. Functional decline was significantly associated with VMS (P=0.003) and (hemi)arthroplasty operation technique (P=0.015) (Table 2). Unfortunately, multivariate logistic regression analysis with functional decline as outcome was not possible due to the high number of missing BI scores.
Table 2 includes patients’ characteristics and their possible association or relation with patient outcomes as functional decline, 30-day mortality, and overall mortality.
Mortality
Nine percentage of all patients died within 30 days after surgery (Table 1). The median age was 85 years, and 56% of the patients were female (Table 2). The prevalence of frailty was 91 and 79% according to VMS and GFI, respectively. Of these patients, 84% had polypharmacy and 96% of them suffered from cardiovascular disease. In the univariate analysis, VMS was significantly associated with 30-day mortality and overall mortality. Other factors associated with mortality were being male, delirium during hospitalization, polypharmacy, presence of cardiovascular disease, and malnutrition.
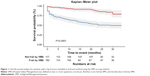
Figure 1 shows the Kaplan–Meier curves of the overall survival among patients with a hip fracture classified as frail (blue line) and not frail (red line) by VMS. Patients who were classified as frail with VMS showed a significantly worse survival than nonfrail patients (overall survival: 57 vs 80%, respectively; Plogrank <0.001). These results were similar when patients were classified according to the GFI method (58 and 81%) (data not shown). The corresponding hazards of death were statistically significant (HRVMS =3.5; 95% CI =2.1–5.7, P<0.001, and HRGFI =2.3; 95% CI =1.2–4.1, P=0.008). Other independent variables of survival in the regression model were age higher than 83 years (HR =2.6; 95% CI =1.5–4.2, P<0.001) and presence of chronic pulmonary disease (HR =0.46; 95% CI =0.2–0.9, P=0.013).
Discussion
In this study, we showed that elderly patients who underwent surgery for hip fracture classification as frail by VMS and GFI are associated with a significantly decreased overall survival. Other independent risk factors for survival were higher age and presence of chronic pulmonary disease. In addition, classification as frail according to VMS was significantly associated with a functional decline after surgery and with 30-day mortality.
VMS
The results of this study are generally consistent with the sparse literature on VMS frailty and outcomes in patients with hip fracture. Patients classified by the VMS as “frail older people” had a higher risk of dying.11 Another study in elderly patients stated that the best predictive power for adverse outcome was found by identifying patients at risk aged 70–80 years and scoring positive on three or four VMS domains or aged >80 years and scoring positive on one or more of the VMS domains.16 The fourth domain in that study was undernutrition. We used three VMS questions about cognitive impairment or confusion during earlier admission periods, activities of daily living (ADL) limitations, and falling. We found that VMS frailty (scoring positive on one of the other questions than falling) was predictable for 30-day mortality, overall mortality, and functional decline. The only study that studied VMS frailty in a population elderly with hip fracture showed that VMS score for delirium risk was predictive for clinical outcome.17
GFI
The existence of higher numbers of missing scores on the GFI frailty score was probably explained by the usability of this questionnaire. The GFI was more difficult to complete than was expected beforehand. During data collection, researchers experienced problems in answering the questions in patients with decline in cognitive functioning and, sometimes, they scored themselves less frail than they actually were.
Another explanation for the missing scores is the inaccurate computer system for selecting eligible patients.
Only one study assessed GFI in patients with hip fractures (N=30). The main study was conducted for vertebral fracture patients. A frailty score of 67% was mentioned only for the total study population.18 Previous studies about the GFI have reported good internal consistency with adequate validity.7,8,11,19 In the present study, GFI was not able to predict 30-day mortality and 1-year mortality. There was an association between GFI and functional decline; however, due to high numbers of missing BI scores, we could not accurately carry out the analyses. Previous studies compared GFI frailty scores only with other frailty measurements, not with patients’ outcomes such as mortality, functional decline, delirium, length of stay, and quality of life.
In this study, chronic pulmonary disease seemed to be protecting with regard to overall mortality. This is inconsistent with earlier studies. Earlier studies in patients with hip fracture showed that patients with chronic pulmonary disease have higher risk of passing away than those without chronic pulmonary disease.20,21 In these studies, patients above the age of 40 or 65 years were included. A similar study, as ours, did not describe pulmonary disease separately but used the Charlson comorbidity index for counting comorbidity.17
Strengths and limitations
The present study has several strengths. It was performed in a general hospital, few exclusion criteria were used, and our study population is a representative group of older patients with hip fracture. To our knowledge, no previous studies investigated the predictive value on adverse outcome of GFI and VMS frailty scores in patients with hip fracture.
There were also limitations in this study. Functional decline by Barthel-20 index is probably not the most relevant outcome of patients after hip fracture. Researchers noticed, during data collection, that in most cases, several months after surgery, the maximum scores on mobility were reached when patients still experienced decline in mobility. Our population was too small for exploring predictive values for 30-day mortality in multivariate analyses. Frailty scoring by VMS and the cutoff point were based on clinical expertise in elderly patients of the geriatric specialists/researchers. The VMS frailty score is based on a commonly accepted guideline in the Netherlands but applied in different ways.
Implications for practice
Frailty should be assessed by VMS in every patient aged 70 years or higher with hip fracture. VMS frailty score is easier to complete than GFI and is also statistically comparable with GFI. When two or more questions are answered with yes, the patient with hip fracture should be documented as frail. For the outcomes assessed in the study, the VMS might be more appropriate than the GFI.
Further research
Further research is necessary to explore which values predict 30-day mortality and to explore the predictive value of frailty on adverse outcome in patients as duration of stay, delirium, functional decline, and quality of life. When knowing these predictive values, it is crucial to explore in what way we can improve adverse outcome in patients with hip fracture in order to realize the main goal of these patients; returning to prefracture functional level.
Furthermore, especially in frail patients, the situation before admission is relevant for decision making, in choosing surgery or not and setting other treatment goals. Therefore, a geriatric comprehensive assessment including GFI probably is relevant for other purposes. Moreover, in this study, frailty was assessed during hospital stay but might also be suitable in the situation before admission. These elements should also be the focus of further research.
Conclusion
VMS frailty scores can be used in establishing frailty and thereby adverse outcome as overall survival and 30-day mortality in older patients with hip fracture.
Disclosure
The authors report no conflicts of interest in this work.
References
van Duin C, Stoeldraijer L. Bevolkingsprognose 2014–2060: groei door migratie. CBS, Bevolkingstrends; 2014. | ||
Lötters FJ, van den Bergh JP, de Vries F, Rutten-van Mölken MP. Current and Future Incidence and Costs of Osteoporosis-Related Fractures in the Netherlands: Combining Claims Data with BMD Measurements. Calcif Tissue Int. 2016;98(3):235–243. | ||
Fried LP, Tangen CM, Walston J, et al; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. | ||
Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–397. | ||
Kistler EA, Nicholas JA, Kates SL, Friedman SM. Frailty and Short-Term Outcomes in Patients With Hip Fracture. Geriatr Orthop Surg Rehabil. 2015;6(3):209–214. | ||
Farhat JS, Velanovich V, Falvo AJ, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg. 2012;72(6):1526–1530; discussion 1530–1531. | ||
Peters LL, Boter H, Buskens E, Slaets JP. Measurement properties of the Groningen Frailty Indicator in home-dwelling and institutionalized elderly people. J Am Med Dir Assoc. 2012;13(6):546–551. | ||
Bielderman A, van der Schans CP, van Lieshout MR, et al. Multidimensional structure of the Groningen Frailty Indicator in community-dwelling older people. BMC Geriatr. 2013;13:86. | ||
Steverink N, Slaets J, Schuurmans H, van Lis M. Measuring frailty: developing and testing of the Groningen frailty indicator (GFI). Gerontologist. 2001;41:236–237. | ||
VMS. Praktijkgids kwetsbare oudere. Available from: http://www.vmszorg.nl/_library/5540/web_2009.0104_praktijkgids_kwetsbare_ouderen.pdf. Accessed April, 2017. | ||
Oud FM, de Rooij SE, Schuurman T, Duijvelaar KM, van Munster BC. Predictive value of the VMS theme ‘Frail elderly’: delirium, falling and mortality in elderly hospital patients. Ned Tijdschr Geneeskd. 2015;159:A8491. Dutch. | ||
Schuurmans MJ, Duursma SA, Shortridge-Baggett LM. Early recognition of delirium: review of the literature. J Clin Nurs. 2001;10(6):721–729. | ||
Kruizenga HM, Seidell JC, de Vet HC, Wierdsma NJ, van Bokhorst-de van der Schueren MA. Development and validation of a hospital screening tool for malnutrition: the short nutritional assessment questionnaire (SNAQ). Clin Nutr. 2005;24(1):75–82. | ||
Wade DT, Hewer RL. Functional abilities after stroke: measurement, natural history and prognosis. J Neurol Neurosurg Psychiatry. 1987;50(2):177–182. | ||
von Elm E, Altman DG, Egger M, et al; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–1499. | ||
Heim N, van Fenema EM, Weverling-Rijnsburger AW, et al. Optimal screening for increased risk for adverse outcomes in hospitalised older adults. Age Ageing. 2015;44(2):239–244. | ||
Folbert EC, Hegeman JH, Gierveld R, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507–515. | ||
Walters S, Chan S, Goh L, Ong T, Sahota O. The Prevalence of Frailty in Patients Admitted to Hospital with Vertebral Fragility Fractures. Curr Rheumatol Rev. 2016;12(3):244–247. | ||
Metzelthin SF, Daniëls R, van Rossum E, de Witte L, van den Heuvel WJA, Kempen GIJM. The psychometric properties of three self-report screening instruments for identifying frail older people in the community. BMC Public Health. 2010;10:176. | ||
Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. | ||
de Luise C, Brimacombe M, Pedersen L, Sørensen HT. Chronic obstructive pulmonary disease and mortality following hip fracture: a population-based cohort study. Eur J Epidemiol. 2008;23(2):115–122. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.