Back to Journals » Neuropsychiatric Disease and Treatment » Volume 13
Relapse and hospitalization in patients with schizophrenia and bipolar disorder at the St Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia: a comparative quantitative cross-sectional study
Received 7 April 2017
Accepted for publication 18 May 2017
Published 15 June 2017 Volume 2017:13 Pages 1527—1531
DOI https://doi.org/10.2147/NDT.S139075
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Getnet Ayano,1 Bereket Duko2
1Research and Training Department, St Amanuel Mental Specialized Hospital, Addis Ababa, 2School of Nursing and Midwifery, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
Background: Relapse and hospital admission are common among, and carry a heavy burden in, patients with schizophrenia and bipolar disorder. The aim of this study was to assess the risk of relapse and hospitalizations in patients with schizophrenia and bipolar disorder at the St Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia.
Patients and methods: A hospital-based comparative cross-sectional study was conducted in June 2016. Systematic random sampling technique was used to recruit 521 (260 schizophrenia cases and 261 bipolar disorder cases) study participants. Face-to-face interviews were conducted by trained psychiatry professionals. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) criteria and Structured Clinical Interview of DSM-IV (SCID) were used.
Results: The risk of relapse and hospitalizations was slightly higher in patients with bipolar disorder than in patients with schizophrenia. A majority of schizophrenic (213 [81.92%]) and bipolar (215 [82.37%]) patients had a history of hospital admission, and 228 (87.69%) schizophrenic and 230 (88.12%) bipolar patients had a history of relapse. Patients who had a history of hospitalizations also had co-occurring substance use disorders compared to those who had no history of hospitalizations for schizophrenia (81.5% vs 37.9%) and bipolar disorder (82.56% vs 38.2%), respectively. Similarly, those patients who had a history of relapse had high comorbid substance use disorders than those who had no history of relapse for both schizophrenia (87.88% vs 47.37%) and bipolar disorder (88.37% vs 47.19%), respectively.
Conclusion: It is vital that, in the local context, mental health professionals strengthen their therapeutic relationships with patients and their caregivers. This might enable patients and their caregivers to express their needs and concerns to them, as well as help to plan proper interventions for patients. Attention needs to be given to screening for comorbid substance use disorders in patients with schizophrenia and bipolar disorder, especially in those who have had a history of relapse and hospitalizations.
Keywords: relapse, hospitalization, schizophrenia, bipolar disorder
Background
Severe mental disorders (SMDs), including schizophrenia, bipolar disorder, schizoaffective disorder and depressive psychosis, have a relatively low prevalence (1%–2%), and they are associated with increased risk of relapse and hospitalizations.1,2 Relapse is common and carries a heavy burden in patients with schizophrenia. The course of illness in schizophrenia is characterized by frequent relapses with exacerbations of psychosis, often resulting in the need for hospitalization. The risk of relapse for a patient with schizophrenia has been estimated to be 3.5% per month, and ~40% of patients experience a relapse within a year following hospital admission.1,3 Risk factors include poor adherence, severe residual psychopathology, poor insight, substance misuse and poor interpersonal relationships.1 It is estimated that 40% of relapses are caused by poor treatment adherence, which is a major problem in many service users.4,5 As relapse in schizophrenia is associated with a heavy human and financial burden, its prevention has become an important goal.
Evidences indicate that up to 90% of patients with bipolar disorder have at least one relapse in their lifetime, with an average of 0.6 relapses per year. After recovery from a mood episode, nearly 50% subsequently have a relapse within 2 years.6 Relapse of mood episodes, delay remission and residual symptoms usually lead to hospitalization, increased suicide risk and/or delay in psychosocial recovery. Poor interepisodic functioning is therefore a common problem in bipolar patients. Frequent bipolar relapses or being hospitalized for bipolar episodes can be very disruptive to patients’ ability to continue their commitments and can consequently reduce patients’ social functioning. Low social functioning can act as a vulnerability factor for more frequent relapses.6
Evidence shows that patients with schizophrenia and bipolar disorder are at higher risk of relapse and hospitalizations. However, in low- and middle-income countries, such as Ethiopia, there is limited research concerning relapse and hospitalizations in patients with schizophrenia and bipolar disorder.
Patients and methods
Study setting and design
A hospital-based comparative cross-sectional study was conducted in June 2016 at the St Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia. The St Amanuel Mental Specialized Hospital is the only mental health hospital in Ethiopia providing services for mental health problems for a long time.
Study population
A total of 521 patients, 260 patients with schizophrenia and 261 patients with bipolar disorder, were included in the study. All the 521 patients were enrolled in the study as prevalent cases. Systematic sampling technique was used to recruit the study participants. Sampling interval was determined by dividing the total study population who had follow-up during the 6-week data collection period by total sample size; then, the starting point was randomly selected.
Inclusion and exclusion criteria
All patients with established Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnoses of schizophrenia/bipolar disorder who underwent treatment follow-up assessment were included in this study. Suicidal gesture or attempt was defined as a self-inflicted act associated with intent to die or use of a method with potential for lethality.
Data collection instruments
Demographic variables were collected using a semistructured questionnaire. Data were collected by trained psychiatry professionals. Relapse and hospital admission was assessed according to DSM-IV-TR . The Structured Clinical Interview of DSM-IV (SCID) was used to identify patients with substance use disorder.
Data processing and analyses
The Statistical Program for Social Science (SPSS version 20; IBM Corporation, Armonk, NY, USA) was used for data analyses. Sociodemographic (age, sex, marital status, areas of residence, religion and education) and clinical (diagnosis, history of alcohol, cannabis, nicotine and khat abuse or dependence) factors were analyzed and reported by using words, tables and charts.
Ethical consideration
The institutional review board of the St Amanuel Mental Specialized Hospital gave ethical clearance for this study. We introduced our study participants to the purpose of the study and informed them about their rights to discontinue the interview at any time; we also received written informed consent from each study participant. Confidentiality was maintained at all levels of the study.
Results
Sociodemographic characteristics of study participants
A total of 260 patients with the diagnosis of schizophrenia and 261 patients with bipolar disorder, with mean age of 31.21 (±SD =6.36) years and 29.87 (±SD =7.33) years for bipolar and schizophrenic patients, respectively, were recruited. Considering bipolar disorder and schizophrenia, there were, respectively, more male respondents (187 [71.6%] and 181 [69.6%]) than female respondents (74 [28.4%] and 79 [30.4%]). More than half the patients with bipolar disorder and schizophrenia were single (157 [60.2] and 151 [58.1%], respectively), and about one-third of them were married (270 [32.5%] and 79 [30.4%], respectively). In terms of occupation, 193 (23.2%) and 87 (33.5%) were private employees, and 59 (22.7%) and 54 (20.7%) were students for participants with schizophrenia and bipolar disorder, respectively (Table 1).
Relapse and hospitalizations in patients with schizophrenia and bipolar disorder
Both relapse and hospitalizations were slightly higher in patients with bipolar disorder than in patients with schizophrenia. A majority of schizophrenic (213 [81.92%]) and bipolar (215 [82.37%]) patients had a history of hospital admission, and 228 (87.69%) of the schizophrenic patients and 230 (88.12%) bipolar patients had a history of relapse (Table 2).
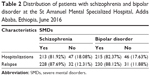  | Table 2 Distribution of patients with schizophrenia and bipolar disorder at the St Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia, June 2016 |
Substance use disorders in patients with schizophrenia and bipolar disorder
A total of 172 (65.9%) schizophrenic and 167 (64%) bipolar patients had substance use disorders, of whom 132 (50.6%) bipolar and 94 (36.2%) schizophrenic patients had khat use disorders, and 102 (39.1%) bipolar and 94 (36.2%) schizophrenic patients had alcohol use disorders in their lifetimes. Moreover, 125 (48.1%) patients with schizophrenia and 81 (31%) patients with bipolar disorder had polysubstance use disorders (Table 3).
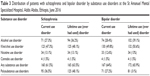  | Table 3 Distribution of patients with schizophrenia and bipolar disorder by substance use disorders at the St Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia, June 2016 |
Relapse, hospitalizations and comorbid substance use disorders in patients with schizophrenia and bipolar disorder
The magnitude of comorbid substance use disorders was higher among patients with a history of relapse and hospitalizations compared to their counterparts in the schizophrenia and bipolar patient groups. Patients who had a history of hospitalizations had co-occurring substance use disorders (schizophrenia 81.5% and bipolar disorder 82.56%). Similarly, those patients who had a history of relapse had high comorbid substance use disorders than those who had no history of relapse for schizophrenia (87.88% vs 47.37%) and bipolar disorder (88.37% vs 47.19%; Table 4).
Discussion
This study revealed that the magnitude of relapse and hospitalizations was very high among patients with SMD in Ethiopia, and it was comparable to that seen among patients with SMD in high-income country settings.2,7–9 In the current study, a majority of schizophrenic (213 [81.92%]) and bipolar (215 [82.37%]) patients had a history of hospital admission, and 228 (87.69%) schizophrenic patients and 230 (88.12%) bipolar patients had a history of relapse. This finding is in agreement with the findings of studies conducted in Norway (96%),7 theUSA8,9 and other countries.2 However, the results from the current study were slightly lower compared to the findings of studies conducted in India (70%), Spain (68%), Iran (56.6%), Ethiopia (Butajira: 65.9%) and other countries.4–6,10–12 The possible reasons might be study design, sociocultural setting, methodology and sample size of the studies.
In this study, both relapse and hospitalizations were slightly higher among patients with bipolar disorder than among those with schizophrenia. This finding is in agreement with other studies that reported significantly higher rates of relapse and hospitalizations among patients with bipolar disorder than among those with schizophrenia.2,7,10,11
In our study, relapse and hospitalizations were common among patients with SMDs, such as schizophrenia and bipolar disorder, compared to relapse and hospitalizations due to other disorders, such as depression and substance use disorders. This finding is in accordance with other studies that revealed significantly higher rates of relapse and hospitalizations among patients with SMDs than among those with other disorders, such as depression and substance use disorders.8,9,13 In this study, about two-thirds of the schizophrenic (172 [65.9%]) and bipolar (167 [64%]) patients had substance use disorders, of whom 132 (50.6%) and 94 (36.2%) bipolar disorder and schizophrenic patients, respectively, had khat use disorder in their lifetime, and 102 (39.1%) and 94 (36.2%), respectively, had alcohol use disorder in their lifetime. The results of our study are similar to those from some previous studies14–16 but different from the studies conducted by Regier et al (higher),17 Ashton and Streem18 and Cassidy et al (both lower).19 This might be due to the differences in data collection instrument, sociodemographics and culture.
Comorbid substance use disorder was more frequent among patients who had a history of relapse and hospitalizations than among those who had no history of relapse and hospitalizations, and it was identified in the current study that patients who had a history of hospitalizations (majority) had co-occurring substance use disorders, compared to those who had no history of hospitalizations for both schizophrenia (81.5% vs 37.9%) and bipolar disorder (82.56% vs 38.2%). Similarly, those patients who had a history of relapse had high comorbid substance use disorders than those who had no history of relapse for both schizophrenia (87.88% vs 47.37%) and bipolar disorder (88.37% vs 47.19%).20–22
Conclusion
Relapse and hospitalizations are observed to be common problems among patients with SMDs. Both relapse and hospitalizations were slightly higher in patients with bipolar disorder compared to those with schizophrenia. Comorbid substance use disorder was a more frequent phenomenon among patients who had a history of relapse and hospitalizations than among those who had no history of relapse and hospitalizations, and it was identified in the current study that the majority of patients who had a history of relapse and hospitalizations had comorbid substance use disorders. Our study findings indicate that much attention needs to be given to the screening and assessment of comorbid substance use disorders among patients with schizophrenia and bipolar disorder, especially among those who have a history of relapse and hospitalizations. Finding comorbid substance use disorders to be common among patients who have a history of suicidal relapse and hospitalizations indicates that further screening for and attention to comorbidity are needed in the case of patients who have a history of relapse and hospitalizations. Further studies are recommended to identify factors associated with relapse and hospitalization.
Acknowledgments
The authors acknowledge the St Amanuel Mental Specialized Hospital, Ethiopia, for funding the study. They appreciate the study participants for their cooperation in providing the necessary information. Because of the sensitivity of the data, the data will not be shared publicly, but we can make available the necessary data for interested persons upon request.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Csernansky JG, Schuchart EK. Relapse and rehospitalisation rates in patients with schizophrenia: effects of second generation antipsychotics. CNS Drugs. 2002;16(7):473–484. | ||
Perlis RH, Ostacher MJ, Patel JK, et al. Predictors of recurrence in bipolar disorder: primary outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatry. 2006;163(2):217–224. | ||
Hogarty GE, Ulrich RF. The limitations of antipsychotic medication on schizophrenia relapse and adjustment and the contributions of psychosocial treatment. J Psychiatr Res. 1998;32:243–250. | ||
Weiden P, Mott T, Curcio N. Recognition and management of neuroleptic noncompliance in schizophrenia. In: Shriqui CL, Nasrallah HA, editors. Contemporary Issues in the Treatment of Schizophrenia. American Psychiatric Publishing, Arlington, VA; 1995:411–434. | ||
Weiden PJ, Zygmunt A. Medication noncompliance in schizophrenia. Part I: assessment. J Prac Psych Behav Health. 1997;3:106–110. | ||
Lam DH, Watkins ER, Hayward P, et al. A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: outcome of the first year. Arch Gen Psychiatry. 2003;60(2):145–152. | ||
Finseth PI, Morken G, Malt UF, Andreassen OA, Vaaler AE. Risk factors of cycle acceleration in acutely admitted patients with bipolar disorder. Acta Psychiatr Scand. 2014;130(5):388–396. | ||
SAMHSA [webpage on the Internet]. Mental and Substance Use Disorders. [updated October 9, 2014]. Available from: http://www.samhsa.gov/disorders. Accessed March 13, 2015. | ||
Weiss AJ, Barrett ML, Steiner C. Trends and Projections in Inpatient Hospital Costs and Utilization, 2003–2013. HCUP Statistical Brief #175. Rockville, MD: Agency for Healthcare Research and Quality; 2014. Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb175-Hospital-Cost-Utilization-Projections-2013.pdf. Accessed March 13, 2015. | ||
Schooler NR. Relapse and rehospitalization: comparing oral and depot antipsychotics. J Clin Psychiatry. 2003;64(suppl 16):14–17. | ||
Simhandl C, König B, Amann BL. A prospective 4-year naturalistic follow-up of treatment and outcome of 300 bipolar I and II patients. J Clin Psychiatry. 2014;75(3):254–263. | ||
Fekadu A, Kebede D, Alem A, et al. Clinical outcome in bipolar disorder in a community-based follow-up study in Butajira, Ethiopia. Acta Psychiatr Scand. 2006;114(6):426–434. | ||
Fekadu A, Desta M, Alem A, Prince M. A descriptive analysis of admissions to Amanuel Psychiatric Hospital in Ethiopia. Ethiop J Health Dev. 2007;21(2):173–178. | ||
Tohen M, Greenfield SF, Weiss RD, Zarate CA Jr, Vagge LM. The effect of comorbid substance use disorders on the course of bipolar disorder: a review. Harv Rev Psychiatry. 1998;6:133–141. | ||
Dalton EJ, Cate-Carter TD, Mundo E, Parikh SV, Kennedy JL. Suicide risk in bipolar patients: the role of co-morbid substance use disorders. Bipolar Disord. 2003;5:58–61. | ||
Tolliver BK. Bipolar disorder and substance abuse: overcome the challenges of “dual diagnosis” patients. Curr Psychiatr. 2010;9(8):33–B. | ||
Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511–2518. | ||
Ashton K, Streem D. Nicotine Dependence: Disease Management Project. entre for Continuing Education, Cleveland Clinic, 2009. | ||
Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disord. 2001;3:e120–e188. | ||
Sanguineti VR, Samuel SE, Schwartz SL, Robeson MR. Retrospective study of 2,200 involuntary psychiatric admissions and readmissions. Am J Psychiatry. 1996;153(3):392–396. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Press; 1994. | ||
Center for Substance Abuse Treatment. Substance Abuse Treatment for Persons with Co-occurring Disorders. Treatment Improvement Protocol (TIP) Ser., No. 42. DHHS Publ. No. (SMA) 05–3992. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


