Back to Journals » Clinical Ophthalmology » Volume 16
Refractive and Visual Outcomes of a Monofocal Non-Constant Aberration Aspheric Intraocular Lens
Authors Hernández-Martínez A, Díaz-del-Rio MA, Ruiz-Santos M, Ruiz-Mesa R , Tañá-Rivero P
Received 11 May 2022
Accepted for publication 20 July 2022
Published 10 August 2022 Volume 2022:16 Pages 2521—2530
DOI https://doi.org/10.2147/OPTH.S373587
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Adrián Hernández-Martínez, Miguel A Díaz-del-Rio, María Ruiz-Santos, Ramón Ruiz-Mesa, Pedro Tañá-Rivero
Ophthalmology Department, Oftalvist Huelva, Huelva, Spain
Correspondence: Adrián Hernández-Martínez, Oftalvist Huelva, Pl. Ivonne Cazenave, 1, Huelva, 21004, Spain, Email [email protected]
Purpose: To evaluate the refractive and visual outcomes following cataract surgery and implantation of a new monofocal non-constant aberration aspheric intraocular lens (IOL).
Methods: Ninety eyes of 86 patients who underwent implantation the CT LUCIA 621P IOL (Carl Zeiss Meditec AG) were retrospectively analyzed in this study. Main outcome measures were refractive error and monocular corrected distance visual acuity (CDVA) and monocular uncorrected distance visual acuity (UDVA) values. Patients were evaluated at 1-month post-surgery and intra- and post-operative complications were recorded.
Results: Eighty percent of the eyes showed a CDVA of 20/25 or better before surgery. The postoperative mean values of monocular distance Snellen decimal UDVA and CDVA were 0.64± 0.22 and 0.89± 0.13, respectively. All eyes showed the same or better difference between UDVA and CDVA. In relation to the postoperative spherical equivalent, the highest percentage of eyes, 31.11%, was for the range between − 0.50 and − 0.14D followed by 22.22% for the ± 0.13D range. Ninety percent of the eyes were within ± 1.00 D and 73.33% of eyes within ± 0.50 D. The mean postoperative spherical equivalent was − 0.18± 0.55D. 37.78% and 76.67% of the eyes showed a value ≤ 0.50 D and ≤ 1.00D, respectively, being the mean postoperative refractive cylinder − 0.81± 0.50D. No adverse events were reported in whole sample intra and postoperatively.
Conclusion: The present study shows that cataract surgery with an monofocal non-constant aberration aspheric IOL implantation resulted in good visual performance and refractive outcomes. This lens may be considered as a valid choice for patients in a standard-routine cataract surgery practice.
Keywords: intraocular lens, phacoemulsification, cataract, aspheric design, aberrations
Introduction
Today, one of the main purposes of cataract surgery is not only to restore visual acuity in our patients but also to provide the best possible visual acuity. One advance was the introduction of aspheric intraocular lenses (IOLs) in the market to correct the spherical aberration of the cornea and hence increase contrast sensitivity improving visual quality.1,2 Despite published studies showing discrepancies about whether these IOLs improve visual performance over that with spherical IOLs (mainly due to inter-eye corneal spherical aberration variability, centration, tilt and asphericity of the IOL),3 recent systematic reviews with meta-analysis concluded that aspheric monofocal IOL implantation resulted in less ocular spherical aberration and fewer ocular higher-order aberration than spherical IOLs. This might explain the better contrast sensitivity in patients with aspheric IOLs, especially under dim light.4,5
It has been published that higher order aberrations can be induced with significant decentration or tilt of IOL with a negative aspheric optic due to the large difference in optical power between the intermediate and peripheral regions of the lens.6,7 IOL with aberration neutral design are less impacted by misalignment.8,9 A new design, called non-constant aberration aspheric, was proposed where the optical power is higher in the center and varies towards the periphery. It shows negative spherical aberration in the central region of the lens being reduced to zero near the periphery. Two models of this design have been evaluated reporting different outcomes for patients and surgeon satisfaction, optical and surface properties, visual performance, stability and Nd:YAG laser capsulotomy rates: the CT LUCIA 601P10–15 and the 611P16–21 IOLs (Carl Zeiss Meditec AG, Jena, Germany). The two main differences between these models are that the C-loop haptic design is angulated (5 degrees) for the 601P and step vaulted (no angulation) for the 611P model. Both show an aspheric Zeiss optic (ZO) design. The design of the 611P model, theoretically, offers more robustness to decentration and tilt, and taking into account that the profile of the optic-haptic junction is thicker and more expanded, there should be more stiffness to the IOL, which would result in better centering and alignment, improving refractive predictability and stability.16 The new model, the CT LUCIA 621P IOL (Carl Zeiss Meditec AG, Jena, Germany) shows the same C-loop haptic design than the 611P model but with an optimized ZO optical aspheric profile. To our knowledge, no study has analyzed the visual and refractive outcomes of the CT LUCIA 621P IOL in order to properly observe the clinical outcomes of this lens in a standard-routine cataract surgery practice. Only one in vitro study with computed tomography has been done to assess the geometry of the lens.22
Then, the aim of the present clinical study is to assess the refractive and visual outcomes in a series of eyes that undergone the CT LUCIA 621P IOL implantation after cataract surgery.
Methods
This single-center retrospective study was approved by the Ethics Committee of the Hospital Clínico San Carlos (Madrid, Spain) and was conducted in accordance with the tenets of the Declaration of Helsinki. Exemption for patient consent was obtained from the Ethics Committee since the study was retrospective and we used a pre-existing database from our center for patients undergoing standard usual cataract surgery. In all cases, privacy and confidentially of patients’ data were ensured throughout the study. The study was registered at the DRKS German Clinical Trials Register (clinical registration number DRKS00028270).
Patients
In this study, we have retrospectively examined data from 90 eyes of 86 patients at the Oftalvist Clinic in Huelva, Spain, between February 2022 and April 2022. Inclusion criteria were patients 50 years of age or older undergone age-related cataract removal (phacoemulsification), clear intraocular media except for cataracts and IOL power ranging from 0.00 to +34.00 D. Exclusion criteria were eyes with irregular cornea (ie, keratoconus), previous corneal refractive surgery, and ocular anomalies or pathologies that could reduce visual function or postoperative IOL stability (ie, severe amblyopia, macular degeneration).
Intraocular Lens
All eyes were implanted with the monofocal CT LUCIA 621P IOL. This hydrophobic acrylic lens has a design with a C-loop platform with an optimized ZO non-constant aberration aspheric design. The IOL is fully preloaded and has a heparin-coated surface for smoother injection and unfolding process. The IOL has step-vaulted haptics to translate the optic posteriorly for better contact with the posterior capsule and shows a 360° square edge design. The overall diameter of the lens is 13.0 mm with an optical zone of 6.0 mm. The diopter range varied from 0.00 to +34.00 D in 0.50-D steps. The Abbe number was 51 and the refractive index 1.49. The IOL comes preloaded in the Zeiss Bluesert injector with different tip sizes that need the following incision sizes: 2.2 for lenses between 0.00 and +24.0D, 2.4 for lenses between +24.50 and +30.00 D and 2.6 for lenses between +30.50 and +34.00D.
Surgical Procedure
All cataract surgical procedures were performed under topical anaesthesia using the Centurion Silver (Alcon, Fort Worth, TX, USA) through a 2.2-mm temporally located clear corneal incision. After cataract removal and posterior capsule polishing, the capsular bag was filled with sodium hyaluronate 1.0% (Ocu+, CIMA, Pittsburgh, PA, USA). The IOL was implanted using a preloaded injector through the 2.2-mm corneal incision expanding it for IOL higher than 24D. After centering the IOL and complete removal of the viscoelastic, the surgery ended sealing the incisions by means of hydration (without sutures in all cases) and administration of 1 mg of cefuroxime (Prokam, Laboratories Théa, Clermont-Ferrand, France) in the anterior chamber.
Preoperative and Postoperative Assessment
Preoperative examination was performed in all patients measuring Snellen decimal monocular best-corrected distance visual acuity (CDVA), slit-lamp biomicroscopy, intraocular pressure tonometry and funduscopy through dilated pupils. Cataracts were graded according to Lens Opacities Classification System (LOCS) III classification. Ocular biometry was performed with the Allegro Biograph (Wavelight AG, Germany) optical biometer, and IOL power calculation was based on this measurement considering the SRK/T (n=83) and Hoffer-Q (n=7) formula, and a historical level of surgically induced astigmatism by the incision of 0.25 D. In those cases when the measurement of optical biometry failed an ultrasound biometer (Tomey AL-4000, Tomey Corporation, Nagoya, Japan) was used (n=20). The targeted refraction in all cases was emmetropia. Post-operative assessments were performed at 1 month after implantation and considered: uncorrected distance visual acuity (UDVA), CDVA, refraction, and slit-lamp biomicroscopy. Adverse events were also recorded.
Statistical Analysis and Sample Size
Statistical analysis was carried out using SPSS software (22.0 version, IBM Corp., Armonk, New York, USA). All the measurements are shown as the mean ± standard deviation (SD). Assuming a sample size of 90 patients, a 95% confidence interval, a standard deviation of 0.12 logMAR (based on a previous similar published paper14) the precision for the primary estimate will be 0.0335 logMAR. This was considered appropriate for the purpose of this study.
Results
In this retrospective study, we have examined 90 eyes of 86 patients. In four patients, cataract surgery was performed bilaterally and in 82 patients, surgery with implantation of the CT LUCIA 621P IOL was performed unilaterally. Table 1 shows the preoperative patients’ demographics. Mean patient age was 72.53±7.40 years (ranging from 57 to 88 years) and 44 were female (51.16%) and 42 were male (48.83%). Cataracts were graded using the LOCS III classification in 57 nuclear (2 × NC2, 3 × NC3, 10 × NC4, 21 × NC5 and 21 × NC6), 10 cortical (1 × C2 and 9 × C3), and 23 subcapsular posterior (3 × P2, 14 × P3, and 6 × P4) lens opacities. Phacoemulsification was uneventful in all cases, and no problems or complications were found in any of the cases at the 1 month of follow-up.
 |
Table 1 Preoperative Demographic Characteristics of Participants Implanted with the CT LUCIA 621P IOL Shown as Means, Standard Deviations (SD) and Ranges |
Standard graphs for reporting refractive and visual acuity outcomes were constructed. For the efficacy of the procedure, Figures 1 and 2 were plotted. Figure 1 provides the cumulative postoperative Snellen UDVA and CDVA, and Figure 2 shows the change in lines of visual acuity between the postoperative UDVA and CDVA. Eighty percent of the eyes showed a CDVA of 20/25 or better and all eyes showed the same or better difference between UDVA and CDVA. The postoperative mean values of monocular distance Snellen decimal UDVA and CDVA were 0.64±0.22 (range from 0.10 to 1.0) and 0.89±0.13 (range from 0.60 to 1.0), respectively. For predictability, Figure 3 shows the histogram of postoperative spherical equivalent refraction relative to the intended target refraction. The highest percentage of eyes, 31.11%, was for the range between −0.50 and −0.14D followed by 22.22% for the ±0.13D range. Ninety percent of the eyes were within ±1.00 D and 73.33% of the eyes within ±0.50 D. The mean postoperative spherical equivalent was −0.18±0.55D. Figure 4 shows the histogram of postoperative refractive cylinder. Specifically, 37.78% and 76.67% of the eyes showed a value ≤0.50 D and ≤1.00D, respectively, being the mean postoperative refractive cylinder −0.81±0.50 D.
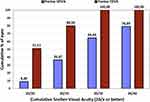 |
Figure 1 Cumulative proportion of eyes having a given uncorrected distance visual acuity (UDVA) and best-corrected distance visual acuity (CDVA) values at 1 month after surgery (efficacy). |
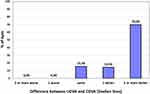 |
Figure 2 Change in lines of visual acuity between the postoperative uncorrected distance visual acuity (UDVA) and best-corrected distance visual acuity (CDVA) at 1 month after surgery (efficacy). |
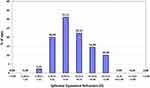 |
Figure 3 Histogram of postoperative spherical equivalent refraction (D) at 1 month after surgery (predictability). |
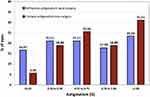 |
Figure 4 Histogram of preoperative corneal astigmatism (D) and postoperative refractive astigmatism (D) at 1 month after surgery (predictability). |
Discussion
Previous clinical and in vitro studies have analyzed some different metrics of previous models of the LUCIA IOL (601P10–15 and 611P16–21), but only one with the new 621P model.22 Then, our purpose in the present study was to provide refractive and visual outcomes in a series of eyes that underwent this implantation after cataract surgery in order to fully describe the clinical outcomes of this new model. Table 2 shows the main characteristics of the different CT LUCIA models.
 |
Table 2 Main Characteristics of the Different CT LUCIA Models |
As we have previously introduced, in addition to the cornea, the visual outcomes of those patients submitted to cataract surgery depend on several factors such as the optical quality of the IOL (spherical and aspherical design) and its position in the capsular bag (effective lens position and postoperative shift). A recent in vitro bench study using computed tomography to assess the geometry of different monofocal C-loop haptic design with identical overall length and optic diameter revealed clear differences between IOLs.22 One of the IOLs analyzed in this study was the CT LUCIA 621PY. These authors found variability in analyses of haptic angle of contact and capsular bag contact between the lenses assessed at all well sizes, but both values were consistently greatest for the CT LUCIA 621PY, which had the lowest percentage change in these values between the smallest and largest diameter wells. These authors pointed out that an IOL with a design that maintains a consistent relationship and contact with the capsular bag independent of native size would be expected to confer intraocular positional stability, limit posterior capsule opacification development, and provide predictable visual outcomes after cataract surgery. These should be assessed in clinical studies.
In this sense, in the current study, we have found good visual acuity outcomes with 80% of eyes with a CDVA of 20/25 or better after the surgery (see Figure 1), being the monocular mean postoperative CDVA 0.89±0.13 (ranging from 0.60 to 1.0). Note that all eyes showed the same or better difference between UDVA and CDVA post-surgery (Figure 2). In relation to predictability (related to the positional stability of the lens in the capsular bag), we found excellent refractive outcomes with 90% of eyes with a spherical equivalent within ±1.00 D (Figure 3) and a mean value less than a quarter of diopter (−0.18±0.55D). For the astigmatism, the mean postoperative refractive cylinder was similar than corneal astigmatism reported before the surgery (−0.81±0.50 D versus 0.81±0.40 D) with 76.67% of eyes with a value ≤1.00 D (Figure 4). Our results support the conclusion of the in vitro bench study previously indicated showing the good visual acuity outcomes.
It has been reported that the 611P model is equipped with the ZO asphericity concept, which means that the power of the IOL is higher in the center and then varies toward the periphery (flatter lens surface at intermediate distance from the lens axis and a steepening at the peripheral region of the lens).16 As introduced, this design may offer more robustness to decentration and tilt, and with the thicker optic-haptic junction, it is expected to provide a better centering and alignment, improving refractive predictability and stability.16 The possible reduction of incidence of higher-order aberrations due to the variability of corneal shapes may benefit patients implanted with this lens. Our results, with the 621P model, with the same C-loop haptic design than the 611P (see Table 2), support this suggestion taking into account the good predictability outcomes: mean spherical equivalent value was <0.25D (−0.18±0.55D). According to the manufacturer, the optic was engineered based on the realistic Liou–Brennan eye model, which is optimized for a pupil size typically found in cataract patients. The central zone induces negative spherical aberration to balance corneal aberration for an improved image quality, and the peripheral zone induces positive spherical aberration to increase decentration tolerance. Thus creates an ideal balance between aberration correction and neutral effects. Unfortunately, as introduced, there are no peer review clinical publications showing visual and refractive outcomes of the CT LUCIA 621P IOL to compare with the present research. However, we consider it interesting to discuss the clinical outcomes reported in publications using previous models.
Borkenstein and Borkenstein10 prospectively analyzed 42 eyes implanted with the CT LUCIA 601P in 28 pseudoexfoliation syndrome patients. They found a CDVA of −0.05±0.13 logMAR after the surgery. The target refraction using the Haigis formula within ±0.5D was reached by 92.9% and by 100% within ±1.0D of all cases, respectively and patient satisfaction was very high, and no halos or glare were reported in any case. Our results showed 90% eyes within ±1.00D. Authors concluded that the implantation of this lens was safe in complicated cases as pseudoexfoliation. Nguyen et al11 in an in vitro study evaluated the power, modulation transfer function, light transmission and light scattering of the CT LUCIA 601PY before and after power adjustment by a femtosecond laser. They found that the power adjustment in this lens produced an accurate change in dioptric power while not significantly affecting the quality of the lens. Labuz et al12 analyzed glistening formation and light scattering in different hydrophobic-acrylic IOLs, obtaining mean values of 85±86 microvacuole (MV)/mm2 and 8.4±0.4 μm for glistening number and size, respectively, and 1.09±0.99 deg2/sr for straylight, for the CT LUCIA 601P model. They found that the density of microvacuoles decreased from the center to the periphery in this model. De Giacinto et al13 analyzed the surface properties of the CT LUCIA 601P and other hydrophobic acrylic lenses using atomic force microscopy and surface contact angle measurements with the sessile drop method was performed to assess lens wettability. They found that the CT LUCIA 601P lens had the lowest contact angle (48.75±4.91 degrees) of all IOL models evaluated. Tandogan et al14 used an accelerated laboratory method to develop glistenings in several IOLs and measure MV density and size (Miyata grading) using an image analysis program. The found a mean glistening density [MV/mm2] and a mean Miyata grading (in brackets) of 11.6±5.7 (0) for the Vivinex XY1, 264.4±110.3 (2.6) for the SN60WF, 6.0±2.8 (0) for the Tecnis ZCB00, 2.2±0.7 (0) for the Avansee PN6A, 851.4±59.4 (3+) for the Aktis SP NS-60YG and 71.0±71.6 (1) for the CT LUCIA 601P. They concluded that while all tested lenses showed glistening with this method, the Aktis and SN60WF showed the highest MV density, followed by the CT LUCIA 601P. In comparison, the Vivinex, Tecnis, and Avansee lenses showed far fewer number of glistening. Liu et al15 compared the visual performance after the implantation of three aberration-correcting aspherical intraocular lenses: LUCIA 601P, CT ASPHINA 509M and the AMO Tecnis ZCB00. 26 eyes were implanted with the LUCIA 601P model and found at 3 months post-surgery mean UDVA of 0.11±0.12 LogMAR and CDVA 0.03±0.06 LogMAR. Mean spherical equivalent and cylinder were −0.02±0.66 D and −0.30±0.61D, respectively. Note that out mean spherical equivalent was −0.18±0.55D. These authors compared three groups of eyes implanted with the three lenses considering that the LUCIA lens shows a non-constant aberration, the ASPHINA lens a spherical aberration of −0.18 μm, and the Tecnis lens a spherical aberration of −0.27 μm. They found no statistically significant differences in UDVA and CDVA between groups (p≥0.83). Wavefront aberrations and contrast sensitivity were also reported and the root-mean-square for total ocular coma was statistically significantly lower in the LUCIA group (p=0.03) and spherical aberration was statistically significantly lower in the Tecnis group (p<0.01). Comparing higher order aberration values among the three groups no statistically significant differences were found (p=0.85) and, neither for contrast sensitivity under both photopic and mesopic lighting conditions (p≥0.05). In this study authors carried out an analysis of intraocular stray light with better values in the LUCIA group (p=0.04). Authors argued that the lower intraocular stray light may be related with that this lens does not produce glistenings of any grade16 compared to the other models.2 These authors concluded that the implant of a non-constant aberration IOL in cataract surgery patients provided lower coma and better intraocular straylight than with the spherical aberration −0.18μm and −0.27μm IOLs despite equivalent postoperative levels of visual acuity and contrast sensitivity.
Borkenstein and Borkenstein16 reported clinical outcomes of 96 eyes of 54 patients who underwent implantation of the CT LUCIA 611P model at 1-year post-surgery. In this model the optic–haptic junction was completely redesigned and changed (wider and stiffer) in comparison to the predecessor CT LUCIA 601 lens (see Table 2). According to the manufacturer, the CT LUCIA 601P was the first generation with a different haptic design, angulated by 5° and with Accuject injector. The CT LUCIA 611P platform shows different changes where the angulation was removed and the haptic design as the injector were changed. Borkenstein and Borkenstein16 indicated that in theory, the optic design should make the IOL more insensitive to decentration and tilt, and given that the profile of the optic–haptic junction is thicker and more expanded, there should be more stiffness to the IOL, which would result in better centering and alignment properties in the capsular bag, thus improving refractive predictability and long-term results regarding refractive stability. They found a mean 0.02 logMAR CDVA (range from 0.14 to −0.10 logMAR) with 94.8% of all subject eyes with 0.10 logMAR or better. In our case 80% of eyes showed an CDVA of 20/25 or better. The spherical equivalent within ±0.50 D was reported in 88 of 96 patients (91.7%) and within ±0.75 D in 96.9%. The percentages in our study were 90% within ±1.00 D and 73.33% within ±0.50 D. The target refraction ±1.00 D was achieved in 100% of subject eyes and no glistenings were reported in any case. In addition, no intraoperative or postoperative adverse events were observed. They concluded that these results demonstrate the safety and efficacy of the lens. In addition, authors pointed out that because of the new designed thicker and stiffer optic–haptic junction regarding improved characteristics of the lens (stability in the capsular bag), some special attention has to be addressed to the slightly different behavior of the lens during implantation and unfolding process. Same authors analyzed this model in 15 eyes of 15 patients with severe cases of pseudoexfoliation syndrome, phacodonesis and small pupils.17 Both 601P and 611P models have the same optical design but in the latter model, as we have indicated previously, the haptics are wider and stiffer, and then this model may be considered a better choice in patients where stability of the capsular bag is compromised. 3 months postoperatively, the mean manifest spherical equivalent was −0.35 D (from 0.00 to −1.00 D) and all eyes were within ±0.50D of their preoperative target. Mean CDVA was 0.02 logMAR at the 3 months postoperative visit. Authors found that in 6 cases (40%) decentration or tilt was detected but these patients did not complain of any subjective visual symptoms or discomfort at any time of the follow-up. No significant refractive shift or refractive surprise occurred during the follow-up of 10 months, and no intraoperative adverse events were noted. These authors concluded that this model provided good surgical performance, excellent refractive stability, and predictable outcomes in challenging cases. Our results, using the 621P model, which has the same haptics design of the 611P, also support this conclusion. According to the manufacturer, the CT LUCIA 621P changed the injector, further optimized the asphericity of the optic to be more forgiving with decentration and increase diopter range. Ling et al18 published a study about the evaluation of Nd:YAG capsulotomy rates carried out for posterior capsule opacification (PCO) in 200 eyes implanted with the CT LUCIA 611P IOL. They reported 3.5% and 8.5% at 1 and 2 years, respectively. In this sense, Wormstone et al19 assessed the CT LUCIA 611PY/capsular bag biomechanical interactions following cataract surgery in a human in vitro graded culture capsular bag model. These authors concluded that throughout culture the lens appeared stable in its position and capsular bag modifications did not change this. They proposed that the lens optic edge shows an enhanced barrier function, which is likely to provide better PCO management in patients. Yildirim et al,20 in a laboratory study, assessed the resistance to MV (glistening) formation analyzing the number of microvacuoles per square mm in the central part of different lenses. Results revealed mean glistening numbers with the highest in the SN60WF lens (66.0±45.5 MVs/mm2), followed by the CT LUCIA 611P (30.7±8.4 MVs/mm2), 800C (2.0±3.6 MVs/mm2), Vivinex XY1 (2.7±2.4 MVs/mm2) and the Tecnics ZCB00 (0.9±0.6 MVs/mm2). This study shows that the resistance to glistening formation differs depending on the hydrophobic acrylic copolymer composition of the IOL material. These authors indicated that there were differences with the values obtained previously in another study (85±86 MVs/mm2)12 and to explain this difference considered that there was an improvement in the manufacturing process between the 601P and the 611P models, which lead to a higher resistance to glistening formation. And, finally, Hienert et al21 carried out a study to compare the dynamics of axial IOL position and stability in the capsular bag after fellow-eye implantation of the CT LUCIA 611P and the CT ASPHINA 409MP IOLs. 100 eyes of 50 patients were analyzed up to 6 months post-surgery using the IOLMaster 700 biometer. They found statistically significant differences in postoperative anterior chamber depth with an overall IOL shift of 0.25±0.16 mm for the ASPHINA lens and 0.14±0.09 mm for the LUCIA 611P IOL (p<0.001). Notwithstanding, no significant differences were found in refraction or visual acuity between groups, reporting a mean UDVA of 0.06±0.14 logMAR and a mean spherical equivalent of −0.32±0.48D for the LUCIA 611P model. In our results, with the 621P model, these values were 0.64±0.22 for UDVA (Snellen decimal) and −0.18±0.55D for the spherical equivalent.
We have to consider that our study has two main limitations. First, there was no clinical direct comparison with other available aspheric IOLs in the market, but previously published literature was used to compare outcomes reported. And, second, despite of previous models of this lens have been assessed with long follow-ups showing good safety outcomes, the follow-up time in our study was short- and long-term effect of this specific IOL model should be further studied. Then, future prospective studies should include other models of lenses and longer follow-up where wavefront aberrations and contrast sensitivity should be measured.
Conclusion
Our study shows that the CT LUCIA 621P IOL provides satisfactory visual acuity and good accuracy in the postoperative refractive error. This lens with a non-constant aberration aspheric design may be considered as a valid choice for patients in a standard-routine cataract surgery practice. Future studies should include the analysis of wavefront aberrations and contrast sensitivity under different lighting conditions, and a comparison with other aspheric IOL models available in the market.
Data Sharing Statement
Data are not available for sharing.
Funding
This study has been funded by an investigator-sponsored study from Carl Zeiss Meditec, Inc. Carl Zeiss did not have any role in study design, data collection and analysis, decision to publish, and preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Packer M, Fine IH, Hoffman RS. Aspheric intraocular lens selection: the evolution of refractive cataract surgery. Curr Opin Ophthalmol. 2008;19(1):1–4. doi:10.1097/ICU.0b013e3282f2d791
2. Dick HB. Recent developments in aspheric intraocular lenses. Curr Opin Ophthalmol. 2009;20(1):25–32. doi:10.1097/ICU.0b013e32831b8bb3
3. Montés-Micó R, Ferrer-Blasco T, Cerviño A. Analysis of the possible benefits of aspheric intraocular lenses: review of the literature. J Cataract Refract Surg. 2009;35(1):172–181. doi:10.1016/j.jcrs.2008.09.017
4. Schuster AK, Tesarz J, Vossmerbaeumer U. The impact on vision of aspheric to spherical monofocal intraocular lenses in cataract surgery: a systematic review with meta-analysis. Ophthalmology. 2013;120(11):2166–2175. doi:10.1016/j.ophtha.2013.04.011
5. Schuster AK, Tesarz J, Vossmerbaeumer U. Ocular wavefront analysis of aspheric compared with spherical monofocal intraocular lenses in cataract surgery: systematic review with metaanalysis. J Cataract Refract Surg. 2015;41(5):1088–1097. doi:10.1016/j.jcrs.2015.04.005
6. Lawu T, Mukai K, Matsushima H, Senoo T. Effects of decentration and tilt on the optical performance of 6 aspheric intraocular lens designs in a model eye. J Cataract Refract Surg. 2019;45(5):662–668. doi:10.1016/j.jcrs.2018.10.049
7. Barbero S, Marcos S, Jiménez-Alfaro I. Optical aberrations of intraocular lenses measured in vivo and in vitro. J Opt Soc Am a Opt Image Sci Vis. 2003;20(10):1841–1851. doi:10.1364/JOSAA.20.001841
8. Shentu XC, Tang XJ, Yao K. Spherical aberration, visual performance and pseudoaccommodation of eyes implanted with different aspheric intraocular lens. Clin Exp Ophthalmol. 2008;36(7):620–624. doi:10.1111/j.1442-9071.2008.01856.x
9. Pieh S, Fiala W, Malz A, Stork W. In vitro strehl ratios with spherical, aberration-free, average, and customized spherical aberration-correcting intraocular lenses. Invest Ophthalmol Vis Sci. 2009;50(3):1264–1270. doi:10.1167/iovs.08-2187
10. Borkenstein AF, Borkenstein EM. Patient and surgeon satisfaction levels after using an acrylic, hydrophobic, monofocal IOL and the malyugin ring in pseudoexfoliation syndrome patients. J Ophthalmol. 2018;2018:3843098. doi:10.1155/2018/3843098
11. Nguyen J, Werner L, Ludlow J, et al. Intraocular lens power adjustment by a femtosecond laser: in vitro evaluation of power change, modulation transfer function, light transmission, and light scattering in a blue light-filtering lens. J Cataract Refract Surg. 2018;44(2):226–230. doi:10.1016/j.jcrs.2017.09.036
12. Labuz G, Knebel D, Auffarth GU, et al. Glistening formation and light scattering in six hydrophobic-acrylic intraocular lenses. Am J Ophthalmol. 2018;196:112–120. doi:10.1016/j.ajo.2018.08.032
13. De Giacinto C, Porrelli D, Turco G, Pastore MR, D’Aloisio R, Tognetto D. Surface properties of commercially available hydrophobic acrylic intraocular lenses: comparative study. J Cataract Refract Surg. 2019;45(9):1330–1334. doi:10.1016/j.jcrs.2019.04.011
14. Tandogan T, Auffarth GU, Son HS, Merz P, Choi CY, Khoramnia R. In-vitro glistening formation in six different foldable hydrophobic intraocular lenses. BMC Ophthalmol. 2021;21(1):126. doi:10.1186/s12886-021-01879-6
15. Liu Y, Zhao J, Hu Y, Li B, Wang J, Zhang J. Comparison of the visual performance after implantation of three aberration-correcting aspherical intraocular lens. Curr Eye Res. 2021;46(3):333–340. doi:10.1080/02713683.2020.1798467
16. Borkenstein AF, Borkenstein EM. Long-term clinical results and scanning electron microscopic analysis of the aspheric, hydrophobic, acrylic intraocular lens CT LUCIA 611P(Y). Clin Ophthalmol. 2018;12:1219–1227. doi:10.2147/OPTH.S167895
17. Borkenstein AF, Borkenstein EM. Surgical experience with a redesigned, fully preloaded, hydrophobic acrylic intraocular lens in challenging cases of pseudoexfoliation syndrome, phacodonesis, and small pupils. Clin Ophthalmol. 2019;13:199–206. doi:10.2147/OPTH.S194420
18. Ling R, Borkenstein EM, Borkenstein AF. Evaluation of Nd: yAGLaser capsulotomy rates in a real-life population. Clin Ophthalmol. 2020;14:3249–3257. doi:10.2147/OPTH.S276329
19. Wormstone IM, Damm NB, Kelp M, Eldred JA. Assessment of intraocular lens/capsular bag biomechanical interactions following cataract surgery in a human in vitro graded culture capsular bag model. Exp Eye Res. 2021;205:108487. doi:10.1016/j.exer.2021.108487
20. Yildirim TM, Schickhardt SK, Wang Q, Friedmann E, Khoramnia R, Auffarth GU. Quantitative evaluation of microvacuole formation in five intraocular lens models made of different hydrophobic materials. PLoS One. 2021;16(4):e0250860. doi:10.1371/journal.pone.0250860
21. Hienert J, Hirnschall N, Ruiss M, Ullrich M, Zwickl H, Findl O. Prospective study to compare axial position stability after fellow-eye implantation of 2 distinct intraocular lens designs. J Cataract Refract Surg. 2021;47(8):999–1005. doi:10.1097/j.jcrs.0000000000000557
22. Borkenstein AF, Borkenstein EM. Geometry of acrylic, hydrophobic IOLs and changes in haptic-capsular bag relationship according to compression and different well diameters: a bench study using computed tomography. Ophthalmol Ther. 2022. doi:10.1007/s40123-022-00469-z
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
