Back to Journals » Clinical Ophthalmology » Volume 9
Reassessment of pneumatic retinopexy for primary treatment of rhegmatogenous retinal detachment
Authors Cohen E , Zerach A, Mimouni M, Barak A
Received 30 June 2015
Accepted for publication 25 July 2015
Published 2 November 2015 Volume 2015:9 Pages 2033—2037
DOI https://doi.org/10.2147/OPTH.S91486
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Eyal Cohen,1,* Amir Zerach,1,* Michael Mimouni,2 Adiel Barak1
1Department of Ophthalmology, Tel Aviv Sourasky Medical Center, Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, 2Department of Ophthalmology, Rambam Health Care Campus, Haifa, Israel
*These authors contributed equally to this work
Background: Pneumatic retinopexy (PR) remains a popular technique for the treatment of rhegmatogenous retinal detachment (RRD).
Objective: To evaluate the single operation and final success rate of PR for primary treatment of RRD and to determine factors associated with anatomical and visual outcomes.
Methods: This retrospective case review study analyzed the data of patients who underwent PR for primary treatment of RRD. Patients with a follow-up period of <2 months were excluded. Single operation success was defined as successful retinal reattachment following a single PR throughout 2 months of follow-up.
Results: Eighty-four eyes met the inclusion criteria. Single operation success was achieved in 50 eyes (59.5%), while 82 obtained anatomical success at the final follow-up visit (97.6%). An average of 0.702±1.095 additional retinal detachment operations was necessary to achieve final anatomical success in the entire cohort (n=84) and 1.4±1.3 in the single operation failure group (n=34). Both groups (single operation success vs failure) did not differ significantly in any of the preoperative variables. Multivariate analysis of pseudophakic patients (n=22) revealed that 52.65% of the variation in single operation outcome was explained by the number of clock-hours detached (partial R2=43.76%, P=0.001). The final best-corrected visual acuity was significantly better in the single operation success group (logarithm of minimum angle [logMAR] 0.229±0.249 vs logMAR 0.747±0.567, P<0.001).
Conclusion: Careful patient selection is warranted before performing PR in RRD, particularly in pseudophakic patients with large detachments. Ultimately 60% of the cases will attach after the procedure with the rest requiring on average 1.4 additional procedures to achieve final anatomical success.
Keywords: pneumatic retinopexy, rhegmatogenous retinal detachment
Introduction
Retinal detachment is the separation of multilayer neurosensory retina from the underlying retinal pigment epithelium. The incidence of rhegmatogenous retinal detachment (RRD) has significant geographic variations ranging between 6.3 and 17.9 per 100,000 people per year.1 In current clinical practice, scleral buckling, pars plana vitrectomy (PPV), and pneumatic retinopexy (PR) are used to treat RRD2 with reported primary success rates of 95%, 71%–92%, and 64%, respectively.3 PR is both safe4 and cost-effective.5 It is used in 14%–17% of cases of RRD making it the second most popular primary modality after PPV.6 The classic indications for PR are retinal breaks confined to the superior clock-hours, retinal break or breaks within 1–2 clock-hours, absence of proliferative retinopathy grade C or D, a cooperative patient who can be positioned, and clear media.7 In addition, in cases with other relative indications, PR was shown to have satisfactory results.7 In spite of the fact that the immediate anatomical success rate of PR has been reported to be lower than that of other techniques, the final best-corrected visual acuity (BCVA) has been shown to be similar.8–10 It seems that though the success rate reported by studies investigating PR in the past 3 decades is declining,10–12 it remains a popular technique.6 Two recent large retrospective studies that investigated the risk factors for failure of PR reported an initial anatomical success rate of 61%–63.3% with a final rate of 96.1%–99.2%.13,14
The aim of this article was to 1) evaluate the initial and final success rate (both anatomically and functionally) of PR surgery for primary treatment of RRD; 2) characterize the complications directly related to this procedure; and 3) identify the subset of patients who are most likely to benefit from this procedure as a primary modality.
Methods
All necessary authorizations were obtained from the Institutional Review Board of the Tel Aviv Medical Center.
Subjects
The medical records of patients who underwent PR between the years 2009 and 2012 at the Department of Ophthalmology of the Tel Aviv Medical Center, a tertiary care hospital in Tel Aviv, Israel, were reviewed.
In our department, PR is used to repair RRD with retinal breaks located between 8 o’clock and 4 o’clock. The procedure is not performed in cases with inferior breaks or lattice between the 4 o’clock and 8 o’clock positions, retinal break >1 hour, inability to detect retinal breaks in detached retina, clinically significant media opacity preventing identification of breaks, proliferative vitreoretinopathy grade C, previous retinal surgery, or poor patient compliance.
Inclusion criteria were a minimum follow-up period of 2 months. Patients who underwent ocular surgery (except cataract surgery) in the same eye prior to PR were excluded from this study. The demographic and preoperative characteristics extracted from each patient’s medical record are depicted in Table 1.
Surgical technique
All patients were treated with a similar PR technique, adapted from Hilton et al by one of the three surgeons (LA, BA, or SS).15 After attempting to identify all the retinal breaks via fundal examination, the necessity, alternatives, and potential complications of the procedure were explained to the patient by the physician before obtaining consent. The PR was performed under retrobulbar or subconjunctival combined with topical anesthesia. In the first stage, transconjunctival cryopexy was applied around each of the retinal breaks. Afterward, 0.5 mL of SF6 or 0.3 mL of C3F8 was injected into the vitreous. Paracentesis was performed in selected patients who required lowering of intraocular pressure. All patients were postoperatively positioned in order to correctly apply pressure to the area of detached retina. When necessary, patients underwent additional laser retinopexy.
Definitions
Single operation success: successful retinal reattachment following a single PR throughout 2 months of follow-up.13 This group included patients who received additional laser or cryotherapy in the postoperative period. Additional retinal detachment repair procedures performed in this group were the result of re-detachment occurring after a period of 2 months.
Final anatomical success: eyes in which the retina remained attached throughout the follow-up period.
Statistical analysis
Statistical analyses were performed using SPSS 21.0 (IBM Corporation, Armonk, NY, USA). We compared both baseline and follow-up characteristics of primary success patients and failure patients by using, whenever appropriate, Student’s t-test for normally distributed variables or Kruskal–Wallis for nonparametric variables. We used χ2 or Fisher’s exact test as indicated for the analysis of categorical variables. We then performed stepwise backward multivariate logistic regression analysis that attempted to determine the baseline variables that enabled to predict success or failure introducing as independent variables those that reached a significant level of <0.3 in univariate analysis. Snellen BCVA values were converted to logMAR units. A P-value of <0.05 was considered significant.
Results
Out of a total of 102 eyes of 102 patients that underwent PR between the years 2009 and 2012, 84 patients fulfilled the inclusion criteria. Reasons for exclusion were a follow-up period of <2 months (n=15) and incomplete procedure or lack of data in medical records (n=3). There were 52 men and 32 women with a mean age of 60.25±11.82 years (median, 60.50 years; range, 34–87) who were followed for a mean duration of 11.8±9.1 months (median, 9.5 months; range, 2–58 months). The mean interval between appearance of visual symptoms and patient arrival was 5±7.9 days (median, 3 days; range, 0–60 days). In 56% of the patients, the right eye was involved. All retinal tears were located in the superior half of the retina, while 61.9% were located specifically in the superotemporal quadrant. Retinal tears were limited to ≤1 hour in 90.5% of the patients, and the size of the retinal detachment was limited to one quadrant or less in 56% of the patients with macular sparing detected in 56% as well. Vitreous hemorrhage at the time of PR was documented in 11.9% of the cases. The follow-up time lasted >3 months in 82% of the patients, >12 months in 39%, and >24 months in 9.5%.
Single operation success
Out of 84 eyes, 50 reached single operation success (59.5%; 95% confidence interval [CI], 48.81–70.24), while 82 obtained final anatomical success (97.6%; 95% CI, 94.33–100.87). Out of the 34 patients from the single operation failure group, 79.4% underwent a single additional reattachment procedure. The mean interval between the primary PR and additional reattachment procedure was 15.4 days (median, 17 days; range, 1–570 days). An overall average of 0.702±1.095 additional retinal detachment operations was necessary to achieve final anatomical success.
Table 1 depicts the clinical characteristics at baseline and after follow-up of the 50 (59.5%) single operation success patients versus the 34 (40.5%) single operation failure patients. Briefly, patients from both groups did not differ significantly in any of the variables examined.
We used stepwise backward multivariate analysis to determine the effect of the variables that were associated with single operation success at a P-value of <0.3 (age, preoperative logMAR, time after cataract surgery, and clock-hours detached). When examining the subgroup of pseudophakic patients (n=22), 52.65% of the variation in single operation outcome was explained by the number of clock-hours detached (partial R2=43.76%, P=0.001) and to a lesser extent by time after cataract surgery (partial R2=8.89%, P=0.074).
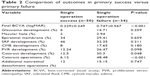
Table 2 depicts the outcomes of the single operation success group versus the single operation failure group. There was a significant difference between both groups in terms of final BCVA (logMAR 0.229±0.249 and logMAR 0.747±0.567, P<0.001). The difference in delta (final BCVA preoperative BCVA), however, was not significant (logMAR 0.544±0.816 and logMAR 0.31±1.15, P=0.314). The single operation failure group had higher rates of cataract development and cataract surgery than the single operation success group (12.5% vs 30.3%, P=0.048, and 6.12% vs 48.48%, P<0.001, respectively). The single operation success group required less additional retinal detachment operations to achieve final anatomical success (0.2±0.5 vs 1.4±1.3, P<0.001).
No intraoperative complications occurred. Table 3 lists the rates of post-PR complications.
  | Table 3 Post-PR complication rates in the entire cohort in descending order |
Discussion
In this retrospective study, single operation success via PR was achieved in 59.5% of the cases. These rates are consistent with the lower part of the wide spectrum of rates reported in the literature with reported success rates ranging from 44% to 94%.16 The relatively low single operation success rate may be the result of including RRD cases that have, by classic definition, lower primary success rates (multiple breaks in multiple quadrants). Vitreous hemorrhage, which coexisted in 11.9% of the RRD cases, may have prevented full identification of all the retinal tears. It is worth mentioning that the nine initial studies between 1986 and 1988 reported single operation success rates that ranged from 84% to 93.55%.16 This is in sharp contrast to the findings of this study and the lower rates reported by three recent studies that demonstrated a range of 60.7%–69.6%.13,14,17
No statistically significant differences were found when comparing the baseline characteristics of the single operation success versus single operation failure groups. Previous studies have reported substantially higher success rates for phakic RRDs in comparison to pseudophakic or aphakic RRDs.16 Our findings are similar to those of a recent study by Fabian et al13 who came to the conclusion that the anatomical outcome is similar in both groups. The main theory for the reported lower success rate is the presence of multiple missed breaks in pseudophakic and aphakic eyes. Therefore, before performing PR in pseudophakic RRD, an in-depth examination of the peripheral retina is warranted.15
Multivariate analysis of the subgroup of pseudophakic patients revealed that 43.76% of the variation in single operation outcome was explained by the number of clock-hours detached (R2=43.76%, P=0.001). The odds ratio for each clock-hour detached in this group was 3.83 (95% CI, 1.04–14.12). This in fact means that the size of detachment in pseudophakic patients predicted an increased risk of single operation failure. A study by Tornambe et al4 on 302 eyes concluded that more extensive detachments are associated with lower single operation success. We speculate that larger detachments could potentially harbor numerous breaks that are more likely to go undetected in pseudophakic patients.
The mean BCVA at the final follow-up for single operation success was statistically significantly better for single operation success patients when compared to single operation failure (logMAR 0.229±0.249 and logMAR 0.747±0.567, P<0.001, respectively). These findings are supported by previous studies that reported better visual outcomes in the single operation success groups.13,14,16 In this study, the difference in delta (final BCVA – preoperative BCVA) between both groups was not statistically significant. We speculate that this may be a result of a relatively low amount of additional retinal detachment procedures required in the single operation failure group (1.4±1.3). These findings are supported by those of Ambler et al18 who demonstrated that initial failure of PR does not adversely affect the visual outcome. As there was a substantial difference in the final BCVA of both groups, perhaps the initial BCVA should be considered when deciding which procedure to perform.
Cataract is one of the leading causes of blindness in Israel.19 In this study, the single operation failure group had higher rates of cataract development and cataract surgery than the single operation success group (12.5% vs 30.3%, P=0.048, and 6.12% vs 48.48%, P<0.001, respectively). No statistically significant differences in rates were found for all other complications. The higher rate of cataract development and cataract surgery in the single operation failure group may have been the result of additional retinal detachment operations performed, such as PPV, which increase the likelihood of developing clinically significant cataract.20,21 Therefore, combined surgery by phacoemulsification and vitrectomy in one session may be considered in cases with a significant cataract.22 The retrospective nature of this study in itself is a limitation as there may be several additional factors that were not studied, which may influence the outcomes. As part of the methodology of this study, a relatively large number of parameters that may have affected the outcomes were collected and studied in order to minimize the influence of such factors.
Conclusion
In summary, PR as demonstrated in this study carries a lower single operation success rate than initially published 3 decades ago. Careful patient selection is warranted before performing PR in RRD, particularly in pseudophakic patients with large detachments. Ultimately 60% of the cases will attach after the procedure. Those in which the procedure does not succeed the first time will require on average 1.4 additional procedures to achieve final anatomical success.
Funding
All authors declare that no grant support or research funding was received for the purpose of this study.
Disclosure
The authors report no conflicts of interest in this work.
References
Mitry D, Charteris DG, Fleck BW, Campbell H, Singh J. The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol. 2010;94(6):678–684. | ||
Fraser S, Steel D. Retinal detachment. Clin Evid. 2010;2010:0710. | ||
Sodhi A, Leung LS, Do DV, Gower EW, Schein OD, Handa JT. Recent trends in the management of rhegmatogenous retinal detachment. Surv Ophthalmol. 2008;53(1):50–67. | ||
Tornambe PE, Hilton GF, Brinton DA, et al. Pneumatic retinopexy. A two-year follow-up study of the multicenter clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology. 1991;98(7):1115–1123. | ||
Goldman DR, Shah CP, Heier JS. Expanded criteria for pneumatic retinopexy and potential cost savings. Ophthalmology. 2014;121(1):318–326. | ||
Hwang JC. Regional practice patterns for retinal detachment repair in the United States. Am J Ophthalmol. 2012;153(6):1125–1128. | ||
Kleinmann G, Rechtman E, Pollack A, Schechtman E, Bukelman A. Pneumatic retinopexy: results in eyes with classic vs relative indications. Arch Ophthalmol. 2002;120(11):1455–1459. | ||
Schaal S, Sherman MP, Barr CC, Kaplan HJ. Primary retinal detachment repair: comparison of 1-year outcomes of four surgical techniques. Retina. 2011;31(8):1500–1504. | ||
Saw SM, Gazzard G, Wagle AM, Lim J, Au Eong KG. An evidence-based analysis of surgical interventions for uncomplicated rhegmatogenous retinal detachment. Acta Ophthalmol Scand. 2006;84(5):606–612. | ||
Han DP, Mohsin NC, Guse CE, Hartz A, Tarkanian CN. Comparison of pneumatic retinopexy and scleral buckling in the management of primary rhegmatogenous retinal detachment. Southern Wisconsin Pneumatic Retinopexy Study Group. Am J Ophthalmol. 1998;126(5):658–668. | ||
Thomas EL. Pneumatic retinopexy. West J Med. 1988;148(6):695. | ||
Zaidi AA, Alvarado R, Irvine A. Pneumatic retinopexy: success rate and complications. Br J Ophthalmol. 2006;90(4):427–428. | ||
Fabian ID, Kinori M, Efrati M, et al. Pneumatic retinopexy for the repair of primary rhegmatogenous retinal detachment: a 10-year retrospective analysis. JAMA Ophthalmol. 2013;131(2):166–171. | ||
Gilca M, Duval R, Goodyear E, Olivier S, Cordahi G. Factors associated with outcomes of pneumatic retinopexy for rhegmatogenous retinal detachments: a retrospective review of 422 cases. Retina. 2014;34(4):693–699. | ||
Hilton GF, Das T, Majji AB, Jalali S. Pneumatic retinopexy: principles and practice. Indian J Ophthalmol. 1996;44(3):131–143. | ||
Chan CK, Lin SG, Nuthi AS, Salib DM. Pneumatic retinopexy for the repair of retinal detachments: a comprehensive review (1986–2007). Surv Ophthalmol. 2008;53(5):443–478. | ||
Rootman DB, Luu S, Conti MS, et al. Predictors of treatment failure for pneumatic retinopexy. Can J Ophthalmol. 2013;48(6):549–552. | ||
Ambler JS, Meyers SM, Zegarra H, Paranandi L. Reoperations and visual results after failed pneumatic retinopexy. Opthalmology. 1990;97(6):786–790. | ||
Avisar R, Friling R, Snir M, Avisar I, Weinberger D. Estimation of prevalence and incidence rates and causes of blindness in Israel, 1998–2003. Isr Med Assoc J. 2006;8(12):880–881. | ||
Melberg NS, Thomas MA. Nuclear sclerotic cataract after vitrectomy in patients younger than 50 years of age. Ophthalmology. 1995;102(10):1466–1471. | ||
Hsuan JD, Brown NA, Bron AJ, Patel CK, Rosen PH. Posterior subcapsular and nuclear cataract after vitrectomy. J Cataract Refract Surg. 2001;27(3):437–444. | ||
Pollack A, Landa G, Kleinman G, Katz H, Hauzer D, Bukelman A. Results of combined surgery by phacoemulsification and vitrectomy. Isr Med Assoc J. 2004;6(3):143–146. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.