Back to Journals » ClinicoEconomics and Outcomes Research » Volume 13
Real-World Six-Year National Cost-Minimization Analysis of IncobotulinumtoxinA and OnabotulinumtoxinA in the VA/DoD Healthcare Systems
Authors Kazerooni R , Howard IM, Keener AM, Bounthavong M
Received 14 May 2021
Accepted for publication 15 June 2021
Published 30 June 2021 Volume 2021:13 Pages 603—609
DOI https://doi.org/10.2147/CEOR.S320212
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Dean Smith
Rashid Kazerooni, 1 Ileana M Howard, 2, 3 Adrienne M Keener, 4, 5 Mark Bounthavong 6, 7
1Merz Pharmaceuticals, LLC, Raleigh, NC, 27615, USA; 2Rehabilitation Care Services, VA Puget Sound, Seattle, WA, USA; 3Department of Rehabilitation Medicine, University of Washington, Seattle, WA, USA; 4Department of Neurology, David Geffen School of Medicine, Los Angeles, CA, USA; 5Parkinson's Disease Research, Education, and Clinical Center, Greater Los Angeles Veterans Affairs Medical Center, Los Angeles, CA, USA; 6VA Health Economics Resource Center, VA Palo Alto Health Care System, Menlo Park, CA, USA; 7Department of Clinical Pharmacy, UCSD Skaggs School of Pharmacy & Pharmaceutical Sciences, San
Diego, CA, USA
Correspondence: Rashid Kazerooni
Associate Director, Health Economics and Outcomes Research, Merz Pharmaceuticals, LLC, 6601 Six Forks Road, Suite 430, Raleigh, NC, 27615, USA
Tel +1.785.249.3233
Email [email protected]
Purpose: This study sought to perform a real-world, long-term cost-minimization analysis for incobotulinumtoxinA (Xeomin®) versus onabotulinumtoxinA (Botox®), given the established non-inferiority when utilized at similar doses.
Methods: The Department of Veterans Affairs (VA) and Department of Defense (DoD) national healthcare systems were included in this analysis. Real-world purchase data for incobotulinumtoxinA were used to estimate the direct drug costs between calendar years 2014 and 2019. Publicly available federal pharmaceutical prices (Federal Supply Schedule and Big 4) were used. The primary outcome was the difference in total direct costs nationally for incobotulinumtoxinA (real-world) versus having hypothetically utilized onabotulinumtoxinA (projected) for similar utilization. Sites utilizing ≥ 100 vials (of 100 Unit equivalents) of incobotulinumtoxinA annually were categorized as “major adopters”. IncobotulinumtoxinA 50 Unit vials were assumed to be an alternative to a 100 Unit vial of onabotulinumtoxinA for 50% of such vial purchases in the base case scenario to account for differences in wastage.
Results: Over the six-year study time frame, 156 sites (76.8%) utilized incobotulinumtoxinA of the 203 total VA healthcare systems and DoD medical centers. Of these sites, 67 were major adopters for at least one year, with a mean of 3.4 years spent as a major adopter over the study period. Average annual savings per major adopter was $105,782. IncobotulinumtoxinA costs for all VA/DoD sites was $46.39 million for the six-year period versus a projected $71.92 million onabotulinumtoxinA cost—a total savings of $25.53 million (35.5% relative reduction). Approximately, 82.8% of savings stemmed from lower drug acquisition cost ($21.14 million) and 17.2% of savings ($4.39 million) was related to reduced wastage. It was estimated that a total of 9958 extra onabotulinumtoxinA 100 Unit vials would have been wasted during the six-year period, translating to the need for a 5.9% increase in vial purchases versus incobotulinumtoxinA.
Conclusion: Meaningful cost savings were realized related to incobotulinumtoxinA adoption over a long-term time frame in the VA/DoD healthcare systems.
Keywords: Xeomin, Botox, cost, federal, savings
Introduction
Prescription drug spending in the United States was estimated to be $476 billion in 2018, representing a 5.5% annual increase from the previous year.1 However, the drug spend for in-clinic drugs has increased more dramatically over the same time frame at 13.0% annual growth.1 Payers will find this information vital to their operation since infusible and injectable in-clinic drugs make up over 15% of all drug spending.1–3 Botulinum toxin (BoNT) agents are costly biologic in-clinic medications used to treat a large variety of therapeutic indications covered by most payers. Broadly speaking, the United States has not developed or implemented policies to control high prescription drug costs.1 However, there is evidence to support that large integrated healthcare systems like the US Department of Veterans Affairs (VA) and US Department of Defense (DoD) have efficiently provided pharmacy benefit management while maintaining a quality at or above private sector care.4,5 With a large patient population (VA provides services for 9 million enrolled veterans nationally, and DoD provides service for 9.6 million people including both active-duty personnel and their families), decision makers will need to be more sensitive to pharmaceutical costs, particularly with high-cost agents such as BoNTs.6,7
Annual reductions in annual spend and drug waste are possible when alternative botulinum toxins are adopted on a healthcare system level. Medicare data, which contains the largest open-access data repository of injectable drug wastage, has reported that a significant portion of botulinum toxin total spend was attributable to waste, with $24 million (6.3% of drug class spend) paid for discarded units in 2017, outpacing rates of wastage payments on other Medicare Part B drugs (2.1%).8 IncobotulinumtoxinA (Xeomin®) has demonstrated comparable efficacy and safety to onabotulinumtoxinA (Botox®) at similar dosing in head-to-head studies for blepharospasm and cervical dystonia; however, incobotulinumtoxinA is currently available at a lower drug acquisition cost.2,9,10 Additionally, the availability of incobotulinumtoxinA in smaller 50 Unit vial sizes allows for flexibility in dosing, reduced wastage and decreased spending for its approved indications.11–13
The goal of this analysis was to perform a cost-minimization analysis comparing real-world incobotulinumtoxinA purchase data versus having hypothetically utilized onabotulinumtoxinA for all associated procedures from the VA/DoD payers’ perspectives over a long-term time period.
Methods
Cost-minimization analysis was performed to compare the total direct costs of using incobotulinumtoxinA to onabotulinumtoxinA from the perspective of two integrated federal healthcare systems (VA and DoD). Real-world purchase data for incobotulinumtoxinA were acquired from Merz Pharmaceuticals, LLC’s data warehouse for the study time-period, which was defined as calendar years 2014–2019.14 Total incobotulinumtoxinA cost was calculated by multiplying the total number of incobotulinumtoxinA vials purchased by the respective price of the vial size for the given calendar year. Projected total costs for onabotulinumtoxinA was generated using data from the incobotulinumtoxinA purchases. The total projected costs were calculated by multiplying the number of incobotulinumtoxinA vials purchased and assuming that the same total number of units would have been purchased. This investigation was undertaken as a cost-minimization analysis given availability of high-quality double-blind randomized control trials establishing non-inferiority between the agents for treatment of adults with cervical dystonia and blepharospasm when utilized at similar doses.9,10
Cost Inputs and Assumptions
Pharmaceutical costs were based on the Federal Supply Schedule (FSS) or Big 4 data which are publicly available for each respective product and vial size (see Table 1).15 The FSS price reflects the negotiated pharmaceutical price that VA pays based on the manufacturer’s price for their “most favored” non-federal customers.16 The Big 4 consists of the VA, DoD, Public Health Service and Coast Guard; the prices associated with Big 4 are defined by Veterans Health Care Act of 1992 (P.L. 102–585) and are set at a maximum of 76% of the non-federal average manufacturers price.17 If there was both an FSS and Big 4 price listed for a drug in a given year, the lower price was used in our analysis. Utilization of FSS pricing is in line with the Second Panel on Cost-Effectiveness in Health and Medicine recommendations for economic analysis.18 The price of each respective product from July 1st of each calendar year was utilized as the reference price point for that year, which was then used for cost calculations. Since incobotulinumtoxinA did not have a 200 Unit vial size available for multiple years within the study time frame, the following assumptions were made for onabotulinumtoxinA pricing: projected onabotulinumtoxinA utilization (by total Units) was assumed to be evenly split between 100 and 200 Unit vial purchases. This assumption was made to account for the fact that the 200 Unit vial of onabotulinumtoxinA had a lower per unit cost (versus their 100 Unit vial size) for most years of the analysis and could have led to a different vial purchase mix if it were to be utilized as an alternative.
 |
Table 1 Cost Inputs |
The units of the various FDA-approved botulinum toxins are not interchangeable with one another. However, there are two high-quality, double-blind, randomized control trials that demonstrated non-inferiority between incobotulinumtoxinA and onabotulinumtoxinA when used at similar doses for blepharospasm and cervical dystonia.9,10 Therefore, for the purposes of this cost-minimization analysis it was assumed that each 100 Unit incobotulinumtoxinA vial was utilized as an alternative to a 100 Unit onabotulinumtoxinA vial. For each purchased 100 or 200 Unit incobotulinumtoxinA vial, it was assumed that a 100 or 200 Unit onabotulinumtoxinA vial at the blended cost would have been the alternative. The onabotulinumtoxinA blended cost was calculated by averaging the cost per unit for both the 100 and 200 Unit vial sizes for that product in the given calendar year.
Wastage Assumptions
With regard to 50 Unit vial purchases of incobotulinumtoxinA, it was assumed that this vial size was utilized as an alternative to a 100 Unit vial of onabotulinumtoxinA for 50% of the 50 Unit vial purchases. This assumption was made given that onabotulinumtoxinA is not available in this smaller vial size and both products are single-use vials.11,19 OnabotulinumtoxinA is manufactured in a 50 Unit vial size only for cosmetic treatment; however, it is not reimbursable by payers for therapeutic indications. The price utilized for onabotulinumtoxinA in these situations was the 100 Unit vial size price for the given calendar year. The extra onabotulinumtoxinA units purchased as a part of replacing the 50 Unit incobotulinumtoxinA vials were additionally utilized for wastage calculations. A sensitivity analysis was conducted to test the impact of this assumption. Total wastage differences for incobotulinumtoxinA versus onabotulinumtoxinA were varied across the plausible range, from 0% to 100%, as a part of a sensitivity analysis. An assumption of no improvement in wastage reduction with incobotulinumtoxinA 50 Unit vials (versus onabotulinumtoxinA) was the lower limit of the sensitivity analysis (0%). Assuming all incobotulinumtoxinA 50 Unit vials were alternatives to onabotulinumtoxinA 100 Unit vials was utilized as the upper limit (100%). For the base case scenario, 50% was utilized.
Outcomes Measures
The primary outcome of this analysis was the total direct costs nationally across the aforementioned integrated federal healthcare systems from utilizing incobotulinumtoxinA versus having hypothetically utilized an equivalent number of units of onabotulinumtoxinA. Other secondary outcome measures assessed included savings per year, relative savings, average savings per major adopting site (defined as sites utilizing at least 100 vials of 100 Unit incobotulinumtoxinA equivalent size in a given calendar year), extra wastage avoided, wastage cost, percentage of total sites adopting any use over time, as well as per member per month (PMPM) cost comparisons at an anonymized sample institution that had been a major adopter across the entire six-year study period. PMPM was defined as the total cost divided by total beneficiaries served that calendar year and then further divided by 12 (for months). It should be noted that all the institutions in this analysis will remain anonymized. All costs were adjusted for inflation to 2020 US dollars ($) as per the US Bureau of Labor Statistic Consumer Price Index.20 All analyses were conducted in Microsoft Excel, 2016 (Microsoft, Redmond, WA, USA).
Results
Overview
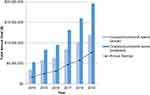
Over the six-year study time frame, 156 VA/DoD sites utilized incobotulinumtoxinA, representing 76.8% of the 203 total VA healthcare systems and DoD medical centers. Of these, 67 sites were major adopting sites for at least one year, with an average of 3.4 years spent as a major adopting site over the study period. Average annual savings per major adopting site was $105,782 (range of savings by a site during a major adoption year: $13,980 to $637,270). IncobotulinumtoxinA cost for all VA/DoD sites was $46.39 million for the six-year period versus a projected cost of $71.92 million for onabotulinumtoxinA, an incremental difference of $25.53 million (35.5% relative savings). Average annual nationwide incobotulinumtoxinA-related savings for the VA/DoD was $4.25 million over the study time frame (range: $1.70 million in 2014 to $7.69 million in 2019). Full results from this can be found in Figure 1.
Wastage
It was estimated that 17.2% of incremental cost reductions stemmed from reduced wastage secondary to purchases of 50 Unit incobotulinumtoxinA vials ($4.39 million) whereas 82.8% ($21.14 million) was related to lower drug acquisition cost. It was estimated that a total of 9958 extra onabotulinumtoxinA 100 Unit vials would have been wasted during the six-year period, translating to the need for a 5.9% increase in vial purchases versus incobotulinumtoxinA. Amongst major adopting sites, relative cost savings varied from 27.7% to 40.9%, depending on usage of 50 Unit incobotulinumtoxinA vials to minimize waste. The proportion of total savings attributed to wastage reduction amongst major adopting sites ranged from 0.0% to 34.9%, again based on usage of 50 Unit incobotulinumtoxinA vials.
Subgroup Analysis of Single Institution
Projected savings were analyzed from an anonymized site in the Southeast region of the United States. At this institution, total utilization of 100 Unit vial equivalents of incobotulinumtoxinA increased gradually from 412.5 vials in 2014 to 1298 vials in 2019. Total incobotulinumtoxinA costs over the six-year time frame totaled $1,685,237 versus a projected $2,580,014 onabotulinumtoxinA cost for the same time frame. This resulted in a projected total savings of $894,777 (34.7% relative reduction) over the six-year study period. More detailed results from this subgroup single institution analysis can be found in Figure 2.
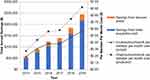 |
Figure 2 IncobotulinumtoxinA versus onabotulinumtoxinA cost outcomes at an anonymized institution. |
Sensitivity Analysis
Total incremental differences nationally related to 50 Unit incobotulinumtoxinA vial purchases were varied from 0% to 100% as a part of a sensitivity analysis. Assuming no national improvement in wastage reduction with incobotulinumtoxinA 50 Unit vials as the lower limit (0%), this translates to $21.14 million minimum savings. This savings was solely from lower drug acquisition cost. Assuming all incobotulinumtoxinA 50 Unit vials were alternatives to onabotulinumtoxinA 100 Unit vials as the upper limit (100%), this translates to $29.92 million in nationwide savings over the study time frame. Both upper and lower limit estimates assume the same amount of total unit utilization over the study time frame.
Discussion
The present analysis found meaningful cost savings related to incobotulinumtoxinA adoption over a six-year time frame in VA/DoD healthcare systems. These two key federal healthcare systems in aggregate provide care for over 18 million people in the United States.4,5 The VA/DoD represent two of the best examples of integrated health care within the United States, providing care equal to or better than private sector care, while maintaining lower costs.4
Results of the present study are supported by other recent related publications. This includes a recently published analysis of a large private neurology practice converting over 100 patients from onabotulinumtoxinA to incobotulinumtoxinA across a multitude of indications.13 The authors noted that, when possible, they selected doses to minimize wastage in their practice, and as a result they saw an 87% reduction in wastage in the first year after conversion.13 Additionally, that analysis noted 52% of total conversion-related savings to be from lower drug acquisition cost, with the other 48% being related to reduced drug wastage.13 Those findings support the results of the present analysis which found that institutions that most widely adopted 50 Unit incobotulinumtoxinA vials nationwide had the highest relative cost savings.
A separate recent national analysis of Medicare data, the largest real-world data comparison of these agents to date, showed an average dosing ratio of 0.94 incobotulinumtoxinA to 1.0 onabotulinumtoxinA across nearly 30,000 patients and 891 physicians that inject predominantly for movement disorders.21 This ratio was even closer for the 338 neurologists (1.01 vs 1.00) and 406 ophthalmologists (0.98 vs 1.00) included in the analysis.21 Similar to findings in the present analysis, total costs were 32.6% lower for incobotulinumtoxinA, while wastage was found to be 64% higher for onabotulinumtoxinA when comparing the agents via national Medicare fee for service data.21 The differences seen in wastage from this large real-world data study of 34 million Medicare fee for service beneficiaries were thought to be related to the availability of a 50 Unit vial with incobotulinumtoxinA (but not available with onabotulinumtoxinA), given that both drugs are available only in single-use vials.21 Additionally, injections per patient per year were not shown to be clinically meaningfully different for incobotulinumtoxinA versus onabotulinumtoxinA.21 Those findings support the assumptions made in the present analysis regarding dosing and wastage of the respective products.
Between 2004 and 2014, the VA Pharmacy Benefits Management Services (PBM) managed to keep the average 1 month cost of prescriptions between $13 and $15.50. This was accomplished using strategies such as having a single national formulary, offering national clinical guidance documents, maintaining strong national pharmacy data domains and investing heavily in having pharmacoeconomics program managers at most sites as well as nationally.5 The VA PBM has also reported that they are able to drive large changes in market share within a market basket in short time frames. One such example is a 2016 study showing an 87% of market share shift in one calendar year from one phosphodiesterase-5 inhibitor to another.22 The VA’s integrated healthcare capabilities and strong national formulary infrastructure make it well suited to be a national leader in balancing cost containment alongside strong clinical care.
There are several limitations to this analysis. First, no clinical outcomes were available as a part of this analysis. This study was meant to serve as a real-world cost-minimization analysis secondary to literature supporting equivalent outcomes at similar doses between these agents. Second, the indications for which incobotulinumtoxinA was utilized by these two federal healthcare systems were unavailable and therefore not assessed. Therefore, some data assessed in this independent analysis may be more expansive than the FDA-approved uses for incobotulinumtoxinA. Third, costs were based on publicly available FSS/Big 4 pricing. Although utilization of those prices is common for purposes of federal cost analyses, it should be noted that any further contracts (such as temporary price reductions) for either drug were not publicly available and therefore could not be accounted for. Fourth, the studied BoNT agents are non-interchangeable and have varying therapeutic indications. IncobotulinumtoxinA is FDA-approved for treatment of adults with blepharospasm, upper limb spasticity, cervical dystonia and chronic sialorrhea. It is FDA-approved for pediatric patients with chronic sialorrhea and upper limb spasticity, excluding spasticity caused by cerebral palsy. Fifth, onabotulinumtoxinA costs in this analysis were the projected costs of having been hypothetically used in place of incobotulinumtoxinA. Although the authors consider the assumptions in the present analysis to be evidence-based and fairly represented as a real-world cost-minimization because real-world purchase data for incobotulinumtoxinA were used, it is still a limitation that should be noted.
Conclusion
Real-world cost savings were found in this analysis related to incobotulinumtoxinA utilization in the VA/DoD healthcare systems. These two key federal healthcare systems have a track record of providing high-quality care while balancing costs. Looking to these fundamental healthcare systems for cost and quality initiatives may be beneficial for other health systems.
Disclosure
Dr. Kazerooni is an employee of Merz Pharmaceuticals, LLC and was formerly a Pharmacoeconomics Program Manager for the Department of Veterans Affairs prior to the conduct of the study. Dr. Howard declares no conflict of interest and received no compensation or funding for this research project. Dr. Keener declares no conflict of interest and received no compensation or funding for this research project. Dr. Bounthavong declares no conflict of interest and received no compensation or funding for this research project.
References
1. Wiest MD, Suda KJ, Rim MH, et al. National trends in prescription drug expenditures and projections for 2019. Am J Health Syst Pharm. 2019;76(15):1105–1121. doi:10.1093/ajhp/zxz109
2. Centers for Medicare & Medicaid Services, Medicare Part B Drug Spending Dashboard & Data. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Information-on-Prescription-Drugs/MedicarePartB.
3. Centers for Medicare & Medicaid Services, Medicare Part D Drug Spending Dashboard & Data. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Information-on-Prescription-Drugs/MedicarePartD.
4. Anhang Price R, Sloss EM, Cefalu M, Farmer CM, Hussey PS. Comparing Quality of Care in Veterans Affairs and Non-Veterans Affairs Settings. J Gen Intern Med. 2018;33(10):1631–1638. doi:10.1007/s11606-018-4433-7
5. Aspinall SL, Sales MM, Good CB, et al. Pharmacy Benefits Management in the Veterans Health Administration Revisited: a Decade of Advancements, 2004–2014. J Manag Care Spec Pharm. 2016;22(9):1058–1063. doi:10.18553/jmcp.2016.22.9.1058
6. United States Department of Veterans Affairs, Veterans Health Administration. Available from: https://www.va.gov/health/aboutvha.asp#:~:text=The%20Veterans%20Health%20Administration%20(VHA,Veterans%20enrolled%20in%20the%20VA).
7. Military Health System. Available from: https://www.health.mil/I-Am-A/Media/Media-Center/Patient-Population-Statistics/Patients-by-Beneficiary-Category.
8. Centers for Medicare & Medicaid Services, Medicare Part B Discarded Drug Units Report. Available from: https://www.cms.gov/research-statistics-data-systems/cms-drug-spending/medicare-part-b-discarded-drug-units-report.
9. Benecke R, Jost WH, Kanovsky P, Ruzicka E, Comes G, Grafe S. A new botulinum toxin type A free of complexing proteins for treatment of cervical dystonia. Neurology. 2005;64(11):1949–1951. doi:10.1212/01.WNL.0000163767.99354.C3
10. Roggenkämper P, Jost WH, Bihari K, Comes G, Grafe S. NT 201 Blepharospasm Study Team. Efficacy and safety of a new botulinum toxin type A free of complexing proteins in the treatment of blepharospasm. J Neural Transm. 2006;113(3):303–312. doi:10.1007/s00702-005-0323-3
11. Merz Pharmaceuticals, LLC. Prescribing Information: xeomin®. Available from: https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=ccdc3aae-6e2d-4cd0-a51c-8375bfee9458&type=display.
12. Kazerooni R, Broadhead C. Cost-utility analysis of botulinum toxin type A products for the treatment of cervical dystonia. Am J Health Syst Pharm. 2015;72(4):301–307. doi:10.2146/ajhp140276
13. Karschney VK, Greeley DR, Retrospective Cost A. Analysis of Patients Who Switched from OnabotulinumtoxinA to IncobotulinumtoxinA in a Private Neurology Practice. Am Health Drug Benefits. 2020;13:5.
14. Merz Pharmaceuticals, LLC Data Warehouse. Federal purchase data 2014-2019. [Data file]. Raleigh: Data Analytics;2020.
15. Office of Acquisition, Logistics, and Construction. Accessed from: https://www.va.gov/oalc/foia/library.asp.
16. Department of Veterans Affairs, Pharmacy Benefits Management (PBM) Services. Available from: https://www.va.gov/opal/docs/nac/fss/pl102585-2021pbmDearMfrLetter.pdf.
17. Congressional Research Service. Available from: https://www.everycrsreport.com/files/20070413_RL33802_b2eae76c0e50dfeda595e4b627298b326046453b.pdf.
18. Carias C, Chesson HW, Grosse SD, et al. Recommendations of the Second Panel on Cost Effectiveness in Health and Medicine: a Reference, Not a Rule Book. Am J Prev Med. 2018;54(4):600–602. doi:10.1016/j.amepre.2017.11.013
19. Allergan, Inc. Prescribing Information: botox®. Available from: https://media.allergan.com/actavis/actavis/media/allergan-pdf-documents/product-prescribing/20190620-BOTOX-100-and-200-Units-v3-0USPI1145-v2-0MG1145.pdf.
20. U.S. Bureau of Labor Statistic Consumer Price Index. Available from: https://www.bls.gov/data/inflation_calculator.htm.
21. Kazerooni R, Watanabe JH. Comparison of botulinum toxins for treatment of movement disorders: real-world utilization and cost analysis in a national Medicare population. J Manag Care Spec Pharm. 2021;27(4):478–487. doi:10.18553/jmcp.2021.20346
22. Spencer SH, Suda KJ, Smith BM, Huo Z, L Jr B, Stroupe KT. Erectile Dysfunction Medication Use in Veterans Eligible for Medicare Part D. J Manag Care Spec Pharm. 2016;22(7):818–824. doi:10.18553/jmcp.2016.22.7.818
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.