Back to Journals » Clinical Ophthalmology » Volume 9
Real-world assessment of diquafosol in dry eye patients with risk factors such as contact lens, meibomian gland dysfunction, and conjunctivochalasis: subgroup analysis from a prospective observational study
Authors Yamaguchi M, Nishijima T, Shimazaki J, Takamura E, Yokoi N , Watanabe H, Ohashi Y
Received 17 September 2015
Accepted for publication 27 October 2015
Published 1 December 2015 Volume 2015:9 Pages 2251—2256
DOI https://doi.org/10.2147/OPTH.S96540
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Masahiko Yamaguchi,1 Takeshi Nishijima,2 Jun Shimazaki,3 Etsuko Takamura,4 Norihiko Yokoi,5 Hitoshi Watanabe,6 Yuichi Ohashi1
1Department of Ophthalmology, Ehime University School of Medicine, Ehime, 2Department of Safety Vigilance Group, Santen Pharmaceutical Co., Ltd., Osaka, 3Department of Ophthalmology, Tokyo Dental College, Ichikawa General Hospital, Chiba, 4Department of Ophthalmology, School of Medicine, Tokyo Women’s Medical University, Tokyo, 5Department of Ophthalmology, Kyoto Prefectural University of Medicine, Kyoto, 6Department of Ophthalmology, Kansai Rosai Hospital, Hyogo, Japan
Purpose: To evaluate the efficacy and safety of diquafosol (DQS) ophthalmic solution in dry eye (DE) patients wearing contact lenses (CLs) or with concomitant meibomian gland dysfunction (MGD) or conjunctivochalasis in a real-world setting.
Patients and methods: From a cohort of patients enrolled in a prospective observational study, DE patients who met the Japanese diagnostic criteria and who received DQS as a monotherapy were extracted and stratified according to the presence or absence of CL use, MGD, and conjunctivochalasis. Corneal and conjunctival fluorescein staining score, tear film break-up time, total symptom score (12 DE-related subjective symptoms), patient-reported outcomes, and adverse reactions were investigated.
Results: DQS treatment resulted in significant improvement in total symptom score, corneal and conjunctival fluorescein staining score, and tear film break-up time without significant differences between patient subgroups with versus without CL use, MGD, or conjunctivochalasis. Comparable proportions of patients perceived symptomatic improvements in all subgroups. There were no adverse reactions specifically associated with the CL use or any comorbidity of MGD or conjunctivochalasis.
Conclusion: DQS can be used effectively and safely as a monotherapy for the treatment of DE patients wearing CLs or with concomitant MGD or conjunctivochalasis.
Keywords: clinical practice, dry eye syndrome, patient-reported outcome, Diquas®
Introduction
Dry eye (DE) is a common eye disorder characterized by insufficiency of the effective tear volume, which makes the eye surface more vulnerable to damage, causing discomfort and irritation.1 Tear insufficiency develops through either decreased tear production or excessive evaporation of secreted tear. Various risk factors underlie the development of DE, including advanced age, the use of a visual display terminal, wearing of contact lenses (CLs), and some diseases (allergic conjunctivitis, conjunctivochalasis, and meibomian gland dysfunction [MGD]). Although DE does not directly cause severe problems in general, serious complications may occur if DE is left untreated, including eye inflammation, scarring of the cornea, and visual impairment.
Mild to moderate DE is commonly treated using artificial tears or lubricating eye drops in conjunction with anti-inflammatory agents as required. Recently, a more etiology-oriented approach has been developed by the introduction of diquafosol (DQS) ophthalmic solution,2–5 which promotes secretion of the tear fluid, rather than supplementing it, increases secretion of soluble mucins, and upregulates expression of membrane-associated mucins.6–8 DQS is an agonist of purinergic receptor P2Y, G-protein coupled, 2 (P2Y2 receptor), which is a type of nucleotide receptor found on the surface of various cells, such as epithelial cells and goblet cells in the conjunctiva, that play important roles in aqueous and mucin secretion to the tear fluid.9,10
Since 2010 when it was first released in Japan, the DQS ophthalmic solution has been used and proven effective for treating DE of various types, including aqueous-deficient, short tear film break-up time, and post-laser in situ keratomileusis types.11 However, its use has been less extensively studied in DE patients with risk factors such as use of CLs, MGD, and conjunctivochalasis. We previously evaluated the efficacy and safety of DQS in over 3,000 DE patients in a real-world setting by a prospective, open-label, non-interventional, observational study.12 In the present study, we focused on and analyzed the efficacy and safety of DQS for the treatment of DE occurring in CL wearers or in patients with MGD or conjunctivochalasis as a comorbidity.
Patients and methods
Patients
Of 3,196 patients analyzed in a prospective observational study of the DQS ophthalmic solution (DIQUAS®; Santen Pharmaceutical Co., Ltd., Osaka, Japan), 965 patients who met the Japanese criteria for DE diagnosis13 and who received DQS as a monotherapy were included in this analysis. Monotherapy indicates the absence of both pretreatment and concomitant therapy for DE. In three groups with or without each risk factor, 64 patients were CL wearers, 32 had MGD, and 50 had conjunctivochalasis (Table 1). This study was conducted on the basis of a request from a regulatory agency in Japan. The study protocol was reviewed and approved in advance by the Pharmaceuticals and Medical Devices Agency, Japan. For this reason, no ethical review by the individual facilities participating in the study was conducted. Patient consent was not obtained as it was not deemed necessary by the Japanese regulatory agency.
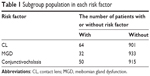  | Table 1 Subgroup population in each risk factor |
Outcome assessment
Efficacy was evaluated according to subjective symptoms, objective findings, and patient-reported outcomes (PROs). Information about subjective symptoms and objective findings was obtained at baseline and 1 and 2 months after the initiation of the DQS treatment. Subjective symptoms included 12 DE-related symptoms (foreign body sensation, photophobia, itchiness, eye pain, dryness, heavy sensation, blurred vision, eye strain, eye discomfort, eye discharge, tearing, and red eye). Each symptom was scored as follows: no symptoms (0 points), mild symptoms (1 point), moderate symptoms (2 points), and severe symptoms (3 points). Objective findings included corneal and conjunctival fluorescein (FL) staining score and tear film break-up time (BUT). For corneal and conjunctival FL staining scores, the cornea was divided into the following three sections: superior, middle, and inferior; and the conjunctiva was divided into the nasal and temporal sides. Each of the five areas was scored as follows:4 no staining (0 points), mild staining (1 point), moderate staining (2 points), and severe staining (3 points). BUT was the time for a dry spot to appear in the tear film after opening the eyes after normal blinking. PROs were investigated 2 months after the initiation of the DQS treatment with a five-point scale from 1 to 5 as follows: much better (1 point), better (2 points), unchanged (3 points), worse (4 points), and much worse (5 points). These were compared with PROs recorded prior to the DQS treatment. The safety of DQS treatment was assessed based on the adverse reactions occurring during the treatment period. Any adverse events for which a causal relationship with the treatment could not be ruled out were considered to be adverse reactions of DQS.
Statistical analysis
Tabulation and analysis were performed using SAS (Version 9.2, SAS institute, Cary, NC, USA). The eye (left or right) used for determining the drug efficacy was selected according to the following rules: 1) the eye affected by the DE condition and being administered DQS was used; 2) if both eyes conformed to rule 1, the eye with the higher baseline corneal and conjunctival FL staining score was used; and 3) if an eye was ineligible according to rules 1 and 2, the right eye was used. Corneal and conjunctival FL staining scores, subjective symptoms, and BUT at baseline and after 1 and 2 months were compared using the paired t-test. The level of significance was set at 5% for both sides.
Results
Subjective symptoms, objective findings, and PROs
Compared with baseline, total symptom scores and corneal and conjunctival FL staining scores significantly decreased, and BUT was significantly prolonged after 1 and 2 months, regardless of the presence or absence of any of the risk factors. Furthermore, regarding the PROs in the CL+, MGD+, and conjunctivochalasis+ groups, a majority of the patients perceived an overall improvement in their conditions (83.6%, 82.7%, and 73.5%, respectively). These were comparable with each group independent of the risk factor (Figures 1–3).
Safety evaluation
Adverse reactions appeared in 47 (4.9%) of the 965 patients surveyed. The main adverse reactions were eye irritation, lacrimation, and eye discharge. Table 2 categorizes the incidence of adverse reactions by each group. There were no notable differences among CL+/-, MGD+/-, or conjunctivochalasis +/- patients. No adverse reactions were considered serious.
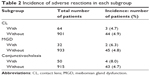  | Table 2 Incidence of adverse reactions in each subgroup |
Discussion
Use of CLs or presence of MGD or conjunctivochalasis as a comorbidity is a DE risk factor and may exacerbate DE. The present retrospective analysis demonstrated that DQS used as a monotherapy was effective for DE, regardless of the presence or absence of CL use, MGD, or conjunctivochalasis. When a CL is worn, the tear film is segmentalized and the tear meniscus height is reduced.14 In addition, the CL surface is inferior to the keratoconjunctival epithelium in terms of water-retentive properties; thus, the tear film on a CL is very unstable. Moreover, use of CLs has been reported to accelerate tear film evaporation.15 Thus, subjective symptoms in CL wearers, such as dryness of eyes or a foreign body sensation, probably arise from mechanisms similar to those in aqueous-deficient DE. Unlike artificial tear formulations that supplement water temporarily, DQS has been reported to promote tear secretion on a continuous basis6 and increase the tear meniscus height up to over 60 minutes in CL users, following the instillation.16 Taken together, the result from the present study demonstrating that DQS is also effective for CL-related DE appears reasonable, as DQS has been shown to be effective for aqueous-deficient DE.17
In the elderly, MGD is frequently encountered and has been reported to be linked to DE.18,19 In obstructive MGD, DE accompanied by increased tear evaporation is likely to occur because the supply of the tear film lipid layer is reduced.20 DE of such type is mainly treated with supportive measures on the lid margin, such as lid hygiene and warm compress therapy, and eye-drop treatment is rarely used.21 The P2Y2 receptor is known to be expressed in the meibomian gland,22 and DQS, a P2Y2 receptor agonist, has been shown to increase lipid production in meibomian gland cells.23 Previously, Arita et al24 reported that long-term administration of DQS to DE patients with concomitant MGD leads to an increased meibomian gland area as measured by non-contact meibography. The present study demonstrated comparative improvements of subjective symptoms and objective findings of DE in patient subpopulations with and without MGD, suggesting that DQS is effective for DE accompanied by MGD. However, it was unknown how severe MGD was or whether MGD was the cause of DE in our patients. Therefore, a more thorough prospective study would be necessary to conclusively prove the effectiveness of DQS monotherapy for DE accompanied by MGD.
Conjunctivochalasis is frequently encountered in the elderly and CL wearers,25,26 is usually caused by an increase in conjunctival laxity and/or by high tension in the lower eyelid, and is characterized by a redundant loose conjunctiva interposed between the globe and the lower, central, and lateral parts of the eyelid. This condition is often associated with tear fluid dysfunction. Also, conjunctivochalasis frequently produces ocular irritation, dryness of eyes, foreign body sensation, and tearing in addition to other symptoms. Although surgical removal of the excess bulbar conjunctiva is known to be an effective treatment option for severe conjunctivochalasis,27 deciding whether or not to use supportive eye-drop treatment for moderate to severe conjunctivochalasis is a challenge. In the present study, DQS was shown to be effective for DE even in patients with concomitant conjunctivochalasis. Previously, DQS was demonstrated to promote aqueous and soluble mucin secretion and thereby increase tear film stability.6,7,9,10 The effectiveness of DQS for DE with concomitant conjunctivochalasis found in the present study may be explained by an increased tear meniscus height resulting from the increased aqueous secretion, which can compensate for ectopic meniscuses in the flaccid conjunctiva. Moreover, increased water and mucin may contribute to reduce the friction between the eyeball and lower eyelid caused by conjunctival laxity. However, no information on conjunctivochalasis severity was available for the patients in this study, and we cannot rule out the possibility that the effectiveness was detectable because the subgroup population in this retrospective analysis comprised mainly patients with mild conjunctivochalasis. Thus, the potential dependence of DQS efficacy on conjunctivochalasis severity needs to be studied in detail to address this issue conclusively. Nevertheless, the result from the present study suggests that DQS is an effective treatment option for DE accompanied by mild conjunctivochalasis.
Regarding the safety, no adverse reactions unique to CL+, MGD+, or conjunctivochalasis+ patients were noted, suggesting that there are no additional safety concerns regarding the use of DQS in patients with these conditions.
Conclusion
Although some additional studies may be necessary on possible relationships between the efficacy and severity, the results from the present study suggest that DQS can be effectively used as a monotherapy for the treatment of DE in CL users and DE accompanied by MGD or conjunctivochalasis with no known specific safety concerns.
Acknowledgment
This analysis and article processing charges for this manuscript were funded by Santen Pharmaceutical Co., Ltd., Osaka, Japan.
Disclosure
TN is an employee of Santen. JS has received consulting fees from Otsuka and honoraria for lectures from Abbot, Alcon, Novartis, Otsuka, and Santen. ET has received honoraria for lectures from Alcon, Astellas, GlaxoSmithKline, Kissei, Kyowa Hakko Kirin, Maruho, MSD, Nippon Boehringer Ingelheim, Novartis, Otsuka, Pfizer, Senju, and Wakamoto. NY has received consulting fees from Kissei and Rohto. YO has received consulting fees from HOYA, Johnson and Johnson, Otsuka, Santen, and Senju. MY and HW report no conflicts of interest in this work.
References
The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5(2):75–92. | ||
Nakamura M, Imanaka T, Sakamoto A. Diquafosol ophthalmic solution for dry eye treatment. Adv Ther. 2012;29(7):579–589. | ||
Matsumoto Y, Ohashi Y, Watanabe H, Tsubota K; Diquafosol Ophthalmic Solution Phase 2 Study Group. Efficacy and safety of diquafosol ophthalmic solution in patients with dry eye syndrome: a Japanese phase 2 clinical trial. Ophthalmology. 2012;119(10):1954–1960. | ||
Takamura E, Tsubota K, Watanabe H, Ohashi Y; Diquafosol Ophthalmic Solution Phase 3 Study Group. A randomised, double-masked comparison study of diquafosol versus sodium hyaluronate ophthalmic solutions in dry eye patients. Br J Ophthalmol. 2012;96(10):1310–1315. | ||
Yamaguchi M, Tsubota K, Watanabe H, Ohashi Y. The safety and efficacy of long-term treatment with 3% diquafosol ophthalmic solution for dry eye. Atarashii Ganka (J Eye). 2012;29(4):527–535. | ||
Yokoi N, Kato H, Kinoshita S. Facilitation of tear fluid secretion by 3% diquafosol ophthalmic solution in normal human eyes. Am J Ophthalmol. 2014;157(1):85–92. | ||
Takaoka-Shichijo Y, Sakamoto A, Nakamura M. Effect of diquafosol tetrasodium on MUC5AC secretion by rabbit conjunctival tissues. Atarashii Ganka (J Eye). 2011;28(2):261–265. | ||
Takaoka-Shichijyo Y, Nakamura M. Stimulatory effect of diquafosol tetrasodium on the expression of membrane-binding mucin genes in cultured human corneal epithelial cells. Atarashii Ganka (J Eye). 2011;28(3):425–429. | ||
Li Y, Kuang K, Yerxa B, Wen Q, Rosskothen H, Fischbarg J. Rabbit conjunctival epithelium transports fluid, and P2Y2 receptor agonists stimulate Cl2 and fluid secretion. Am J Physiol Cell Physiol. 2001;281(2):C595–C602. | ||
Jumbkatt JE, Jumblatt MM. Regulation of ocular mucin secretion by P2Y2 nucleotide receptors in rabbit and human conjunctiva. Exp Eye Res. 1998;67(3):341–346. | ||
Koh S. Clinical utility of 3% diquafosol ophthalmic solution in the treatment of dry eyes. Clin Ophthalmol. 2015;9:865–872. | ||
Yamaguchi M, Nishijima T, Shimazaki J, et al. Clinical usefulness of diquafosol for real-world dry eye patients: a prospective, open-label, non-interventional, observational study. Adv Ther. 2014;31(11):1169–1181. | ||
Shimazaki J; Dry Eye Research Group. Diagnostic criteria of dry eye 2006 [in Japanese]. Atarashii Ganaka (J Eye). 2007;24:181–184. | ||
Nagahara Y, Koh S, Maeda N, Nishida K, Watanabe H. Prominent decrease of tear meniscus height with contact lens wear and efficacy of eye drop instillation. Eye Contact Lens. 2015;41(5):318–322. | ||
Guillon M, Maissa C. Contact lens wear affects tear film evaporation. Eye Contact Lens. 2008;34(6):326–330. | ||
Nagahara Y, Koh S, Nishida K, Watanabe H. Prolonged increase in tear meniscus height by 3% diquafosol ophthalmic solution in eyes with contact lenses. Clin Ophthalmol. 2015;9:1029–1031. | ||
Koh S, Ikeda C, Takai Y, Watanabe H, Maeda N, Nishida K. Long-term results of treatment with diquafosol ophthalmic solution for aqueous-deficient dry eye. Jpn J Ophthalmol. 2013;57(5):440–446. | ||
Uchino M, Dogru M, Yagi Y, et al. The features of dry eye disease in a Japanese elderly population. Optom Vis Sci. 2006;83(11):797–802. | ||
Viso E, Rodríguez-Ares MT, Abelenda D, Oubiña B, Gude F. Prevalence of asymptomatic and symptomatic meibomian gland dysfunction in the general population of Spain. Invest Ophthalmol Vis Sci. 2012;53(6):2601–2606. | ||
Goto E, Endo K, Suzuki A, Fujikura Y, Matsumoto Y, Tsubota K. Tear evaporation dynamics in normal subjects and subjects with obstructive meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2003;44(2):533–539. | ||
Matsumoto Y, Dogru M, Goto E, et al. Efficacy of a new warm moist air device on tear functions of patients with simple meibomian gland dysfunction. Cornea. 2006;25(6):644–650. | ||
Cowlen MS, Zhang VZ, Warnock L, Moyer CF, Peterson WM, Yerxa BR. Localization of ocular P2Y2 receptor gene expression by in situ hybridization. Exp Eye Res. 2003;77(1):77–84. | ||
Wen Q, Li Y, Kuang K, Yerxa B, Fischbarg J. Effect of P2Y2 agonists on lipid secretion by cultured rabbit meibocytes. Invest Ophthalmol Vis Sci. 2002;43(suppl):Abstr 3146. | ||
Arita R, Suehiro J, Haraguchi T, et al. Topical diquafosol for patients with obstructive meibomian gland dysfunction. Br J Ophthalmol. 2013;97(6):725–729. | ||
Mimura T, Yamagami S, Usui T, et al. Changes of conjunctivochalasis with age in a hospital-based study. Am J Ophthalmol. 2009;147(1):171–177. | ||
Mimura T, Usui T, Yamamoto H, et al. Conjunctivochalasis and contact lenses. Am J Ophthalmol. 2009;148(1):20–25. | ||
Yokoi N, Komuro A, Maruyama K, Tsuzuki M, Miyajima S, Kinoshita S. New surgical treatment for superior limbic keratoconjunctivitis and its association with conjunctivochalasis. Am J Ophthalmol. 2003;135(3):303–308. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



