Back to Journals » Therapeutics and Clinical Risk Management » Volume 17
Real-Time Ultrasound Detection of Left Paratracheal Esophagus on Air Entry into the Gastric Antrum in the Induction Period of General Anesthesia: A Prospective, Randomized Study
Received 1 October 2020
Accepted for publication 11 January 2021
Published 28 January 2021 Volume 2021:17 Pages 103—109
DOI https://doi.org/10.2147/TCRM.S284322
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Zhengping Li,* Xiaozhong Yuan,* Wei Deng
Department of Anesthesiology and Pain Medicine, The Affiliated Hospital of Jiaxing University, Jiaxing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Wei Deng Email [email protected]
Background: Positive-pressure ventilation (PPV) delivered via a facemask during anesthesia induction can result in gastric content being inhaled into the lungs. We hypothesized that the real-time ultrasound left paratracheal esophagus monitoring could more effectively reduce air entry into the stomach than real-time ultrasound monitoring of the gastric antrum (GA).
Methods: Patients were divided into two groups: study (S; n=30) and control (C; n=30) groups. During the induction of general anesthesia, mask ventilation adopts a pressure control mode. The initial ventilation pressure of both groups was 15 cmH2O. Before anesthesia induction, an ultrasonic probe was used to monitor the cross-sectional area (CSA) of the GA and the presence of gas in the stomach. During and after anesthesia induction, group S used a high-frequency ultrasound probe to observe the entry of air from the left paratracheal esophagus into the GA. The ventilation pressure was gradually reduced over time until no esophageal air was found. In group C, the ventilatory pressure was set maintained at 15 cmH2O and the CSA of the GA and air intake were monitored using an ultrasonic probe.
Results: Before and after PPV, the CSA of the GA in group S decreased (P< 0.001), whereas the CSA in group C increased (P=0.002). The GA CSA in group C after PPV was larger than in group S after PPV (P=0.002). The proportion of patients who experienced intragastric air intake in group S (23.3%) was significantly lower than that in group C (66.7) (P=0.001).
Conclusion: Compared with ultrasound monitoring of the GA, real-time ultrasound detection of LPEOAE into the GA during anesthesia induction was more effective, more sensitive, significantly reduced the prevalence of intragastric air intake, and provided sufficient tidal volume and oxygen for patients.
Keywords: left paratracheal esophagus, anesthesia, ultrasonography, gastric antrum
Introduction
Pulmonary aspiration of gastric contents is a serious perioperative complication.1–3 Although understanding of lung aspiration-related problems has increased in recent decades, the incidence and related mortality of perioperative lung aspiration have not improved greatly, and lung inhalation of gastric contents continues to lead to high morbidity and mortality.4–7
During anesthesia induction, anesthesiologists use ultrasound to observe the area of the gastric antrum (GA). They search for the “comet tail” sign to determine whether there has been air intake into the stomach, but this method detects air once large amounts of gas have already entered the stomach.8 It is possible to detect intragastric air intake under ultrasound monitoring, which may increase the risk of reflux aspiration, particularly for some emergency patients presenting with a large quantity of gastric contents. Therefore, ultrasound can be used to monitor the air intake of the left paratracheal esophagus in real-time. If the left paratracheal esophagus is found to have air intake under ultrasound, then the left paratracheal esophagus is compressed immediately or the airway pressure is reduced, which can reduce the risk of air intake in the GA.
Although the cricoid pressure technique is still recognized as the standard of care, it has never been prospectively studied. Recently, Bouvet et al8 revealed that the permeability of the esophagus during ventilation can be assessed at the level of the antrum using an ultrasound device. The recent description of low left paratracheal compression as a method to prevent gastric insulation has demonstrated the efficacy of the maneuver. However, gastric assessment is still performed distally. In the present study, we propose an earlier more proximal assessment of the compression maneuver. Our main goal was to compare the real-time ultrasound monitoring of LPEOAE and real-time ultrasound monitoring of the GA as a more effective approach to reduce the amount of air entering the stomach. The second goal was to monitor whether left paratracheal esophageal intake (LPEOAE) can provide adequate tidal volume and oxygen to the patient in real time by ultrasound.
Methods
Ethical Approval of the Study Protocol
The study protocol was approved by the ethics committee of the Affiliated Hospital of Jiaxing Medical University (Jiaxing, China) and was registered in the Chinese Clinical Trial Register (ChiCTR-2,000,031,124) was registered before patient enrollment. All participants provided written informed consent before study enrollment. This trial was conducted in accordance with the Declaration of Helsinki 1975 and its later amendments.
Inclusion and Exclusion Criteria
From 9 March to 9 May 2020, sixty patients scheduled for a surgical procedure under general anesthesia were enrolled in the present study. The inclusion criteria were patients: (i) with an American Society of Anesthesiologists score of I or II; age between 18 years and 80 years; and (iii) with a minimal risk of pulmonary aspiration from gastroesophageal reflux. The exclusion criteria were patients: (i) with an indwelling gastric tube; (ii) at risk of inhalation of gastric contents (ie, patients suspected of having a full stomach and diagnosed with long-term gastrointestinal digestive diseases); (iii) with a body mass index (BMI) >26 kg/m2; (iv) suspected of having a difficult airway (anesthesiologists with more than five years of clinical anesthesia experience after professional training experienced difficulty in mask ventilation or intubation, or both.); (v) who had previously undergone gastric surgery.
Grouping
Using the envelope method for randomization, patients were assigned to two groups: the study (S) and control (C) groups. All participants stopped intake of solids for ≥6 h and liquids 2 h before surgery. Drugs were not given in advance before the study intervention.
Procedures
Patients were placed supine with their neck extended in the “sniffing” position. Electrocardiography, pulse oximetry, non-invasive arterial blood pressure, and monitoring of administration of muscle relaxants were undertaken. The cross-sectional area (CSA) of the GA at the visible level of the aorta and superior mesenteric artery was measured using a curvilinear transducer with a 5–8-MHz probe in the LOGIQ and Ultrasound System (GE Healthcare, Chicago, IL, USA).8,9 Before anesthesia induction, the left paratracheal esophagus of the patients in group S and group C was located with a linear ultrasound transducer with a 7–14-MHz probe. This was achieved by positioning the probe in the transverse (axial) orientation over the left paratracheal area (just above the clavicle).10,11 At the same time, an ultrasonic 5–8-MHz probe was used to monitor the CSA of the GA and the presence of gas in the stomach in groups S and C. An anesthesiologist measured the CSA of the GA before the induction of general anesthesia in the two groups. The antral CSA was assessed by measuring the anteroposterior diameter (D1) and longitudinal diameters (D2) of a single section of the GA in the sagittal plane passing through the aorta. The antral CSA was calculated using the formula:12 antral CSA=π × D1 × D2/4.
Anesthetic management followed a standard protocol. The induction of anesthesia was started with pre-oxygenation for 3 min and intravenous injection of midazolam (0.05 mg/kg bodyweight), sufentanil (0.5 µg/kg), propofol (2 mg/kg) and rocuronium (0.6 mg/kg). Upon TOF-Watch® SX (Organon, Dublin, Ireland) monitoring, when the reading showed the TOF value to be 0, pressure mask ventilation was performed using the two-handed “C” maneuver. Mask ventilation was undertaken in pressure-control mode (frequency 15 bpm; inspiratory:expiratory ratio=1:2; no positive end-expiratory pressure). Adequacy of ventilation was ensured by: chest rises; square, regular capnograph traces; end-tidal carbon dioxide of 3.9–5.3 kPa; tidal volume of 6–10 mL/kg. The initial value of the ventilation airway pressure in both groups was 15 cmH2O. In group S, the left paratracheal esophagus of patients in group S was located with a linear ultrasound transducer with a 7–14-MHz probe. This was achieved by positioning the probe in the transverse (axial) orientation over the left paratracheal area (just above the clavicle)10,11 (Figure 1). Air intake in the left paratracheal esophagus was monitored by another anesthesiologist in real-time. If obvious gas-like strong echoes were observed in the cross-section of the esophagus, gas was considered to have entered the esophagus. At this time, the anesthesiologist reduced the ventilation pressure until no obvious esophageal gas-like strong echoes were observed. At the same time, the ultrasonic probe was used to monitor the GA and to measure the CSA of the GA and intragastric air intake. In group C, the airway pressure was maintained at 15 cmH2O. An ultrasonic probe was used to monitor the CSA of the GA and air intake during and at the end of anesthesia induction. The duration of positive-pressure ventilation (PPV) delivered by a mask in both groups was 2 min. Tracheal intubation was undertaken after the end of mechanical ventilation. The presence of gastric air insufflation was defined as an increase in the CSA of the antrum and presence of air artifacts in the antrum (comet tail, posterior acoustic shadow).8
Primary Outcomes and Secondary Outcomes
The primary outcomes of this study were to compare the real-time ultrasound monitoring of LPEOAE and real-time ultrasound monitoring of the GA, to more effectively reduce the amount of air entering the stomach. The secondary outcomes were to monitor whether the left paratracheal esophageal intake (LPEOAE) could provide adequate tidal volume and oxygen to the patient in real-time by ultrasound.
Statistical Analyses
The sample size was calculated using PASS 15.0 (NCSS Statistical Software; www.ncss.com). Assuming a 20% probability of intragastric air intake in a pilot experiment S group and 60% of 10 patients of the C group, this sample size would give power of 0.9 at α of 0.05, using a two-sample, two-tailed Student’s t-test. A sample size of 27 was required for each group. Estimating that 10% of patients would drop out of the study, 30 cases were recruited for each group.
Data were evaluated by an independent analyst blinded to the allocation of the patient groups. Statistical analyses were performed using SPSS 25.0 (IBM, Armonk, NY, USA). Continuous variables are expressed as the mean ± SD. The Student’s t-test was employed for comparison of continuous variables with a normal distribution. The Mann–Whitney U-test was used to compare continuous variables with a non-normal distribution. The chi-square test was employed to compare intragastric air intake. The corrected P-value was obtained directly, and P<0.05 was considered significant.
Results
Sixty patients were screened for eligibility for study inclusion. The consort diagram is shown in Figure 2. Ultimately, 60 patients were included in the final analysis. The demographic features of patients in the two treatment groups are described in Table 1.
 |
Table 1 Basic Characteristics of Patients in the Two Groups (n=30 for Each Group) |
 |
Figure 2 Consort diagram for the study. |
Before and after PPV, the CSA of the GA in group S decreased (P<0.001), whereas that in group C increased (P=0.002) (Table 2). The CSA of the GA in group C after PPV was larger than that in group S after PPV (P=0.002) (Table 2). The proportion of patients who experienced intragastric air intake in group S was 23.3%, and the proportion in group C was 66.7%; this difference was significant (P=0.001) (Table 3). Compared with group S, group C had a higher tidal volume (P<0.001), lower end-expiratory carbon dioxide concentration (P=0.027), higher end-expiratory oxygen concentration (P<0.001), and higher end-expiratory airway pressure (P<0.001) (Table 1).
 |
Table 2 Cross-Sectional Area (CSA) of the Gastric Antrum Before and After Positive-Pressure Ventilation (cm2) |
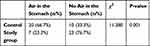 |
Table 3 Gastric Air Intake Was Observed in Both Groups |
Discussion
This was a prospective, randomized study evaluating the real-time ultrasound detection of LPEOAE into the GA during induction of general anesthesia. We found that real-time ultrasound monitoring of the left paratracheal esophagus can more effectively reduce air into the stomach than ultrasound real-time monitoring of the GA, and that real-time monitoring of LPEOAE by ultrasound can provide patients with sufficient tidal volume and oxygen.
Significantly fewer patients experienced intragastric air intake in group S than in group C. In addition, the CSA of the GA decreased after PPV in group S, which may have been associated to the induction of anesthesia using opioids. Some studies have shown that opioids can significantly contract the smooth muscle of the stomach.13–15 In addition, the CSA of the GA in group C increased after PPV, which may have been due to the entry of a large volume of gas into the stomach. Bouvet et al found that gastric air intake was measured at an inspiratory pressure of 10, 15, 20, and 25 cmH2O without use of neuromuscular blockers.8 Under these inspiratory pressures, the proportion of individuals undergoing gastric insufflation ranged from 20% to 60%. Our study was based on use of neuromuscular blockers, but our data are similar to the results reported by Bouvet et al12 However, in our study, during PPV delivered by a mask in the early stage of general-anesthesia induction, high-frequency ultrasound was used to monitor the left paratracheal esophagus. When a strong echo gas shadow entered the esophagus in the inspiratory phase, the mechanical ventilation pressure was reduced over time. This action can prevent excessive gas from entering the stomach, and the results showed that it could also significantly reduce the prevalence of intragastric air intake. Hence, real-time ultrasound monitoring of the left paratracheal esophagus may be more sensitive than that of ultrasound monitoring of the GA, and it can also allow early clinical intervention to avoid flatulence. Simultaneously, we found that, following real-time ultrasound monitoring of LPEOAE into the GA and timely adjustment of ventilation pressure, the CSA of the GA decreased or did not increase significantly compared with the CSA before ventilation, suggesting an obvious effect of early intervention.
The end-tidal volume, end-expiratory partial pressure of carbon dioxide, and the end-expiratory oxygen concentration were also observed at the end of the PPV delivered by a mask in both groups. The average tidal volume and exhaled oxygen concentration were significantly increased in patients with PPV at 15 cmH2O. However, according to ultrasound monitoring of the left paratracheal esophagus, the average value of the end-expiratory tidal volume and end-expiratory oxygen concentration in patients with timely adjustment of ventilation pressure was 8.5 mL/kg and 85.4%, respectively, indicating that the effect of denitrification, oxygen supply and ventilation was good. During PPV delivered by a mask, real-time ultrasound monitoring of LPEOAE into the GA revealed that the average airway pressure was 12.3 cmH2O. At this peak pressure level, esophageal intake was not obvious, thereby suggesting that airway pressure should be maintained at 12.3 cmH2O during PPV delivered by a mask. The prevalence of intragastric air intake in group S was 23.3%, which may have been associated with early high-pressure ventilation.
This study had four main limitations. First, the cohort size was relatively small. Second, we studied PPV only at 15 cmH2O. Third, passive esophageal dilatation during PPV can also lead to false-positive results of esophageal intake caused by gas entering the esophagus. Fourth, the BMI of all patients in our cohort was 26 kg/m2. Hence, our method may not be suitable for obese patients or patients with a difficult airway.
Conclusions
Compared with ultrasound monitoring of the GA, real-time ultrasound detection of LPEOAE into the GA during anesthesia induction was more effective, more sensitive, could reduce the prevalence of intragastric air intake significantly, and could provide sufficient tidal volume and oxygen for patients during the intervention.
Data-Sharing Statement
The authors agree to share individual deidentified participant data. All data are published in the China Clinical Trial Registration Center. No additional unpublished data are available. You can log into the China Clinical Trial Registration Center to obtain the available data. Once the article is published, it can be used permanently.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
This manuscript was handled by Wei Deng, MD.
Funding
This study was supported by Key Discipline Established by Zhejiang Province and Jiaxing City Jointly–Pain Medicine(2019-ss-ttyx), Key Discipline of Anesthesiology of Jiaxing City (2019-zc-06) and Key Laboratory of Neurology and Pain Medicine of Jiaxing.
Disclosure
Zhengping Li and Xiaozhong Yuan are co-first authors for this study. The authors report no conflicts of interest for this work.
References
1. Bouvet L, Barnoud S, Desgranges FP, Chassard D. Effect of body position on qualitative and quantitative ultrasound assessment of gastric fluid contents. Anaesthesia. 2019;74(7):862–867. doi:10.1111/anae.14664
2. Desgranges FP, Gagey Riegel AC, Aubergy C, de Queiroz Siqueira M, Chassard D, Bouvet L. Ultrasound assessment of gastric contents in children undergoing elective ear, nose and throat surgery: a prospective cohort study. Anaesthesia. 2017;72(11):1351–1356. doi:10.1111/anae.14010
3. Kaydu A, Gokcek E. Preoperative assessment of ultrasonographic measurement of antral area for gastric content. Med Sci Monit. 2018;24:5542–5548. doi:10.12659/MSM.908520
4. Van de Putte P, Perlas A. Gastric sonography in the severely obese surgical patient: a feasibility study. Anesth Analg. 2014;119(5):1105–1110. doi:10.1213/ANE.0000000000000373
5. Smith ANAG, Smith G. Gastroesophageal reflux and aspiration of gastric contents in anesthetic practice. Anesth Analg. 2001;93:494–513. doi:10.1097/00000539-200108000-00050
6. Sakai T, Planinsic RM, Quinlan JJ, Handley LJ, Kim TY, Hilmi IA. The incidence and outcome of perioperative pulmonary aspiration in a university hospital: a 4-year retrospective analysis. Anesth Analg. 2006;103(4):941–947. doi:10.1213/01.ane.0000237296.57941.e7
7. Neilipovitz DT, Crosby ET. No evidence for decreased incidence of aspiration after rapid sequence induction. Can J Anesth. 2007;54:9. doi:10.1007/BF03026872
8. Bouvet L, Albert ML, Augris C, et al. Real-time detection of gastric insufflation related to facemask pressure-controlled ventilation using ultrasonography of the antrum and epigastric auscultation in nonparalyzed patients a prospective, randomized, double-blind study. Anesthesiology. 2014;120:326–334. doi:10.1097/ALN.0000000000000094
9. Bolondi L, Bortolotti M, Santi V, Calletti T, Gaiani S, Labò G. Measurement of gastric emptying time by real-time ultrasonography. Gastroenterology. 1985;89(4):752–759. doi:10.1016/0016-5085(85)90569-4
10. Kim H, Chang JE, Won D, et al. The effect of cricoid and paralaryngeal force on upper oesophageal occlusion during induction of anaesthesia: a randomised, crossover study. Anaesthesia. 2020;75(2):179–186. doi:10.1111/anae.14873
11. Gautier N, Danklou J, Brichant JF, et al. The effect of force applied to the left paratracheal oesophagus on air entry into the gastric antrum during positive-pressure ventilation using a facemask. Anaesthesia. 2019;74(1):22–28. doi:10.1111/anae.14442
12. Bouvet L, Miquel A, Chassard D, Boselli E, Allaouchiche B, Benhamou D. Could a single standardized ultrasonographic measurement of antral area be of interest for assessing gastric contents? A preliminary report. Eur J Anaesthesiol. 2009;26(12):1015–1019. doi:10.1097/EJA.0b013e32833161fd
13. Ahlstrand R, Thorn SE, Dahlkvist A, Wattwil M, Magnuson A. Barrier pressure of the oesophagogastric junction during propofol induction with and without alfentanil: a double-blind, randomised, crossover study in volunteers. Eur J Anaesthesiol. 2012;29(1):28–34. doi:10.1097/EJA.0b013e328349a036
14. Cock C, Doeltgen SH, Omari T, Savilampi J. Effects of remifentanil on esophageal and esophagogastric junction (EGJ) bolus transit in healthy volunteers using novel pressure-flow analysis. Neurogastroenterol Motil. 2018;30(2):e13191. doi:10.1111/nmo.13191
15. Sáez-González E, Díaz-Jaime FC, García-Morales N, et al. Opioid-induced functional esophagogastric junction obstruction. Gastroenterología y Hepatología. 2017;40(4):296–298. doi:10.1016/j.gastrohep.2015.12.014
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

