Back to Journals » Pragmatic and Observational Research » Volume 14
Real-Life Effectiveness of MP-AzeFlu (Dymista®) in Swedish Patients with Persistent Allergic Rhinitis, Assessed by the Visual Analogue Scale
Authors Stjärne P, Nguyen DT, Kuhl HC
Received 2 June 2022
Accepted for publication 14 September 2022
Published 4 January 2023 Volume 2023:14 Pages 1—11
DOI https://doi.org/10.2147/POR.S375403
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor David Price
Pär Stjärne,1 Duc Tung Nguyen,2 Hans Christian Kuhl2
1Department of Otorhinolaryngology, Karolinska Institute, Stockholm, Sweden; 2Global Clinical Sciences, Meda Pharma GmbH & Co. KG (A Mylan Company, Now Viatris), Bad Homburg, Germany
Correspondence: Pär Stjärne, Karolinska University Hospital, Department of Otorhinolaryngology, Rhinology, Stockholm, 17176, Sweden, Tel +46707250749, Fax +46 8 774 7907, Email [email protected]
Background: Many allergic rhinitis (AR) patients have moderate/severe persistent disease. MP-AzeFlu (Dymista®) comprises intranasal azelastine hydrochloride and fluticasone propionate in a novel formulation delivered in a single device.
Objective: This prospective, noninterventional study assessed the effectiveness of MP-AzeFlu (one spray/nostril twice daily; azelastine hydrochloride = 548 μg; fluticasone propionate = 200 μg) on relieving AR symptom severity.
Methods: A visual analogue scale (VAS; 0 mm [not at all bothersome] to 100 mm [very bothersome]) was used during a 42-day MP-AzeFlu treatment period by 161 persistent AR (PER) patients in routine clinical practice in Sweden. Patients also assessed their sleep quality.
Results: VAS scores decreased from baseline during the treatment period and patients achieved a clinically relevant VAS score cutoff before Day 7, with 89.3% reporting well or partly controlled symptoms on Day 1. VAS score decreased from 61.4 ± 22.4 mm (baseline) to 32.1 ± 24.6 mm on Day 28 and 26.1 ± 24.3 mm on Day 42 (both p < 0.0001), an overall reduction from baseline on Day 42 of 38.1 ± 28.2 mm. The percentage of patients with very good/good sleep quality increased from 3.7%/28.6% on Day 0 to 16.5%/51.5% on Day 42.
Conclusion: MP-AzeFlu provides effective, rapid control of PER assessed by VAS in a real-world clinical setting in Sweden. Symptom improvement was observed at Day 1, sustained for 42 days, and associated with improved sleep quality. MP-AzeFlu significantly improved the QoL of the patients and was well tolerated.
Keywords: azelastine, Dymista®, effectiveness, fluticasone propionate, MP29-02, MP-AzeFlu, perennial allergic rhinitis, persistent allergic rhinitis, seasonal allergic rhinitis
Introduction
Allergic rhinitis (AR) is a highly prevalent allergic respiratory disease affecting approximately 24% of the European population,1 and includes symptoms of sneezing, nasal obstruction, itchy nose and rhinorrhoea.2 AR is a long-term condition that can bother patients for two or more seasons of the year.1 Persistent symptoms often lead to sleep deprivation, which can negatively impact patients’ daily activities, as well as continually interfere with their work and social lives.1,2
The severity of AR can be classified as mild or moderate/severe. The Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines have classified “intermittent” allergic rhinitis as symptoms that are present less than 4 days per week or for less than 4 consecutive weeks, and “persistent” allergic rhinitis as symptoms that are present more than 4 days/week and for more than 4 consecutive weeks.2 A recent guideline from MACVIA-ARIA (Contre les Maladies Chroniques pour un Vieillissement Actif-Allergic Rhinitis and its Impact on Asthma) endorses a simple visual analogue scale (VAS; range, 0 to 100 mm), with a 50-mm cut-off to assess AR control and guide treatment decisions.3 Previous studies have indicated that changes in VAS scores greater than 10 mm are clinically meaningful.4,5
MACVIA-ARIA recommends that treated PER patients with VAS scores ≥5 to 10 mm escalate their treatment to intranasal corticosteroids or intranasal corticosteroids plus azelastine hydrochloride.3 MP-AzeFlu (Dymista®) is an intranasal AR treatment that comprises an intranasal antihistamine (azelastine hydrochloride) and an intranasal corticosteroid (fluticasone propionate) in a novel patented formulation provided in a single device.6 MP-AzeFlu is indicated for the relief of symptoms of moderate or severe seasonal and perennial AR (SAR and PAR) if monotherapy with either intranasal antihistamine or glucocorticoid is not considered sufficient.3,6
The real-life effectiveness of MP-AzeFlu has been studied in Swedish patients with SAR and/or PAR,7 and those patients recorded significant improvement in VAS scores over approximately 14 days. However, effectiveness in Swedish patients with PER over the longer term remains to be determined.
Although a lot of studies already exist for MP-AzeFlu, there is a lack of local data for Swedish patients. This non-interventional study (NIS) was designed to capture data about the background, symptoms, previous treatments and treatment effectiveness of patients suffering from persistent allergic rhinitis. This, in turn, would help better AR management among Swedish patients by the physicians. This study was conducted to characterize the type of patient with PER who is prescribed MP-AzeFlu in real-life in Sweden and physicians’ reasons for prescribing it.
Materials and Methods
Study Design
This was a prospective, multicenter, noninterventional study (NIS) conducted in Sweden from November 2014 to July 2016. The study was performed in accordance with European regulations (EU 2001; ICH E2E 2004; EMA 2012), and the study documents were approved by a central ethics committee.
The study consisted of an inclusion visit (Day 0, baseline) and an optional follow-up visit at a participating site. At the inclusion visit, the physician documented patient demographics, AR phenotype, allergen sensitization, symptomatology, and previous AR treatments since the past year (including current immunotherapy; prior to MP-AzeFlu prescription) in the electronic case report form (eCRF). Physicians also recorded their reason for prescribing MP-AzeFlu. Data on symptom severity, level of disease control, and assessment of sleep were recorded by the patient on a diary card, which was returned to the physician after 6 weeks at an optional follow-up visit. Patients were permitted to return the diary card to the physician by mail at the conclusion of the study in lieu of a follow-up visit. After receipt of the diary card, the data were transcribed into the patient’s eCRF. The intended study duration was 42 days.
Physicians
Physicians from Sweden who were involved in the management of AR, such as general practitioners; allergists; and ear, nose and throat specialists, were invited to participate in this prospective NIS. Each physician was asked to document MP-AzeFlu treatment in six patients.
Patients
Eligible patients were aged ≥12 years with moderate or severe PER (ie, symptoms >4 days/week for >4 consecutive weeks) and were prescribed MP-AzeFlu (one spray/nostril twice a day; daily doses: azelastine hydrochloride 548 μg; fluticasone propionate 200 μg) according to the summary of product characteristics.6 AR diagnosis was verified by local standard practice (eg, skin prick test or serum immunoglobulin E measures) as in the real-world clinical practice. The decision to include a patient in the study was made independently from and after the decision to prescribe MP-AzeFlu nasal spray. Treatment for at least 6 weeks was considered necessary. All patients (and caregivers, for those aged <18 years) were required to provide written informed consent prior to participation in the study.
Data Collection and Assessments
Severity of Symptoms
During the inclusion visit, patients used a VAS from 0 mm (not at all bothersome) to 100 mm (very bothersome) to evaluate the severity of their symptoms during the preceding >4 weeks. Thereafter, patients assessed symptom severity experienced during the previous 24 hours using the VAS in the morning prior to MP-AzeFlu use on Days 0, 1, 3, 7, 14, 21, 28, 35, and 42.
Disease Control
On Day 1, patients recorded the level of disease control within the previous 24 hours using a four-category scale provided on the diary card (symptoms well controlled, symptoms partly controlled, symptoms uncontrolled, unknown).
Quality of Sleep
During the inclusion visit (Day 0) and on Days 7, 14, 21, 28, 35, and 42 after the start of treatment, patients assessed their sleep for the previous 7 nights on a five-category rating scale (very good, good, fair, bad, very bad).
Safety
All suspected adverse drug reactions (ADRs) and special situations (defined as pregnancy, breastfeeding, adverse reaction related to occupational exposure, lack of efficacy or any overdose, abuse, off-label use, misuse or medication error) were documented by the physician in the eCRF. All suspected ADRs were coded using the Medical Dictionary for Regulatory Activities (MedDRA) coding system (version 19.0). An ADR was defined as a noxious and unintended response to MP-AzeFlu. Other adverse events (AEs) were also recorded and included any untoward medical occurrence in a patient taking MP-AzeFlu that was not necessarily directly related to the treatment. In addition, serious AEs, such as death, life-threatening event, birth defect, an event requiring hospitalization, or other event resulting in a significant medically important condition, were captured in the eCRF.
Statistics
All analyses were based on the safety population, which included all patients who had been treated with MP-AzeFlu and in which the physician had confirmed the validity of the data. Statistical analysis was computed using SAS (version 9.4; Cary, NC, US). Analysis of covariance (ANCOVA) for repeated measurement was used to analyse the change of AR symptom severity from baseline to Days 1, 3, 7, 14, 21, 28, 35, and 42 using baseline as covariate, and the VAS measurements at the respective postbaseline time points and baseline as dependent variables repeated in time. Only patients from the safety population with at least one valid postbaseline assessment recorded in their diary card were analyzed via ANCOVA.
Nonparametric Wilcoxon signed-rank test was performed for difference in sleep quality from baseline to each following time point.
Results
Patient Characteristics
For this NIS, 24 physicians in Sweden enrolled 161 adults/adolescents (mean [standard deviation {SD}] age, 37.5 [15.7] years; range, 12 to 77 years) with documented moderate/severe PER (Table 1). Most patients had both SAR and PAR (69.6%; n = 112), with 30.4% (n = 49) having PAR alone. Among all enrolled patients, sensitization to animal dander predominated (cat: 59.0%; dog: 51.6%; other pet: 22.4%), followed by dust mite (42.9%) and mould (10.6%). All patients met ARIA criteria for having moderate/severe AR. Prior to MP-AzeFlu prescription, 55.3% of patients reported troublesome symptoms, 50.9% reported both impairment of daily activities and disturbance of sleep, and 34.2% reported impairment of school work.
 |
Table 1 Baseline Characteristics of per Patients in Sweden (Safety Population) |
The most frequent AR symptoms reported by patients were nasal congestion (84.5%; n = 136), followed by runny nose (59.6%; n = 96), sneezing (49.7%; n = 80), nasal itching (43.5%; n = 70), and allergic rhinoconjunctivitis (36.6%; n = 59). In particular, 68.3% of patients reported that congestion was the most bothersome symptom. Prior to the study, the majority of PER patients had been previously treated with intranasal corticosteroids (83.2%) or oral antihistamines (67.1%), with 73.9% reporting the use of two or more AR therapies since the past year. The most common reason for MP-AzeFlu prescription was insufficiency of past therapies (79.5%), or alternative therapies were not considered sufficient to treat acute symptoms (16.1%).
Assessments
Severity of Symptoms
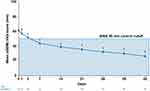
At baseline (Day 0, assessment of symptoms experienced during the past 24 hours prior to start of treatment), the mean ± SD VAS score in the total population was 61.4 ± 22.4 mm (N = 161). The mean VAS scores decreased during the treatment period, with the most rapid decrease occurring during the first week of treatment (Figure 1). On average, patients achieved the ARIA-defined VAS score cutoff of 50 mm for controlled symptoms before Day 7. Moreover, MP-AzeFlu patients continued to experience a rapid VAS score reduction from baseline to 32.1 ± 24.6 mm on Day 28 and 26.1 ± 24.3 mm on Day 42 (both p < 0.0001), corresponding to an overall reduction from baseline on Day 42 of 38.1 ± 28.2 mm (n = 98). Based on the change from baseline VAS scores, symptoms were significantly improved from Day 1 onward (p ≤ 0.0011).
VAS results were consistent irrespective of age (ie, 12 to 17 y and 18 to 65 y; Figure 2A), sex (Figure 2B), baseline disease severity (ie, less severe: baseline VAS score 50 to 74 mm; more severe: baseline VAS score 75 to 100 mm; Figure 2C), or traditional AR phenotype classification (ie, PAR only or SAR and PAR; Figure 2D).
Disease Control
One day after the start of MP-AzeFlu treatment among patients with available data (n = 112), 20.5% (n = 23) rated their AR symptoms during the last 24 hours as “well controlled”, 68.8% (n = 77) rated their symptoms as “partly controlled”, and only 10.7% (n = 12) rated their symptoms as “uncontrolled.” Thus, 89.3% (n = 100) patients had well or partly controlled symptoms on Day 1.
Quality of Sleep
Patient-assessed sleep quality consistently improved from baseline through Day 42 (Figure 3A). The percentage of patients with very good/good sleep quality increased from 3.7%/28.6% on Day 0 (n = 161) to 16.5%/51.5% on Day 42 (n = 97). The Wilcoxon signed-rank test demonstrated statistically significant postbaseline improvements from Day 7 through Day 42 (p < 0.001). Similar patterns in sleep quality improvements were reflected in both AR phenotype subgroups (PAR and SAR+PAR; Figure 3B).
Safety
Two ADRs, lip pain and epistaxis, were reported in one patient in the safety population (0.6%). The physician assessed both events as probably related to MP-AzeFlu treatment, which led to drug withdrawal. Both events started on the same day and were noted for 2 weeks but were resolved through the end of the observation period. No serious ADRs occurred in this study.
Discussion
This NIS was designed to capture data about the background, symptoms, previous treatments, and treatment effectiveness of patients suffering from PER. Although this study has been conducted in several European countries, including Austria and Ireland, this report describes the results of the data analysis for Sweden. The sample size of 161 patients was considered sufficient to draw general conclusions from the descriptive analysis on patient background and MP-AzeFlu treatment effectiveness and safety in routine clinical practice. The primary objective of this prospective NIS was to gather knowledge on the effectiveness of MP-AzeFlu nasal spray in routine clinical practice in patients with persistent allergic rhinitis, therefore patients with only SAR did not qualify to investigate the study objective. The study was also started in the non-pollen season (November). As SAR symptoms are relieved quickly upon medication, there were no patients with SAR as per the inclusion criteria.
The study population corresponded well with the label with respect to indication and target population.6 Nearly all patients were prescribed MP-AzeFlu because alternative therapies had not been sufficient in the past or were considered insufficient to treat acute symptoms. All patients met ARIA criteria for having moderate or severe AR. Approximately two-thirds (69.6%) of the patients suffered from SAR and PAR, and the remaining patients were diagnosed with PAR only (30.4%). Compared with the populations of patients with moderate or severe SAR in clinical studies with MP-AzeFlu, the patients in this study generally had a shorter history of AR (ie, 16 vs 20 to 22 years) and a higher proportion of male participants (47.8% vs 31% to 38%).8
Treatment guidelines for AR recommend intranasal corticosteroid as first-line therapy.3 Therefore, it was not surprising that intranasal corticosteroid was the most frequently used symptomatic treatment of AR prior to MP-AzeFlu; 83.2% of the patients had used one or more intranasal corticosteroids during the preceding year. Oral antihistamine was used by 67.1% of patients, intranasal decongestant by 18.0%, and ocular antihistamine by 11.2%. A majority of patients (73.9%) had previously used two or more allergy medications. This number and that of patients who had previously used intranasal corticosteroid are higher than those reported in earlier NIS studies with MP-AzeFlu (68% and 51%, respectively) in six European countries,7 which may be explained by the persistent character of AR symptoms in this study. Approximately 10% of the patients had undergone or were undergoing immunotherapy at the start of the current study, which is not dissimilar to a previous MP-AzeFlu study in which 14.2% of patients had previously undergone immunotherapy and 9.5% of patients were currently receiving immunotherapy.7
The lag between Day 0 to last day of treatment or diary card documentation was a mean ± SD of 37.6 ± 9.7 days, suggesting that, of those patients with one or more documented postbaseline effectiveness measurements (n =122), most adhered to the 42-day treatment period. Between the start of treatment with MP-AzeFlu nasal spray to the last day of the observational period, AR symptom severity decreased by a mean of 34.9 mm on a VAS ranging from 0 (not at all bothersome) to 100 mm (very bothersome). This reduction is similar to that observed among patients with diary documentation through Day 42 (mean decrease, 38.1 mm). In previous real-world studies of MP-AzeFlu for patients with moderate-to-severe AR, the mean reduction in VAS score ranged from 30.8 to more than 60 over 14 days.7,9–11
Previous studies have suggested that a >10-mm difference in AR symptom severity VAS scores is a clinically meaningful change.4,5 By Day 3 of the present study, 50% of patients had VAS symptom severity score decreases from baseline that centered around the median value of 9.5 mm (interquartile range, ‒21.0 to 0.0), with 25% of patients (ie, those in the highest quartile of the data set) demonstrating clinically significant improvements of ≥21.0 mm in AR symptom severity. On Day 42, 75% of the patients (ie, the three highest quartiles of the data set) had a clinically significant decrease from baseline VAS score of ≥19.0 mm. These improvement rates are slightly lower than those presented by the earlier pan-European NIS7 in SAR patients, which might be because of the broader use of intranasal corticosteroids and use of more medications by PER patients prior to their enrolment in the present study.
On Day 1, approximately 89% of patients with available symptom-control data assessed their symptoms as “well controlled” or “partly controlled”, while 11% assessed their symptoms as uncontrolled. These results indicate that most patients experienced symptom control after only 1 day of MP-AzeFlu treatment, consistent with a previous report that symptoms improved significantly within 5 minutes12 and 30 minutes13 of MP-AzeFlu treatment. Symptom improvement was seen in all subpopulations, irrespective of AR type (PAR only, SAR and PAR), age (adolescent, adult, elderly patients), baseline symptom severity (VAS score 55 to 74 mm, VAS score 75 to 100 mm), and sex.
Sleep quality improved continuously throughout this NIS, as reflected by increasing rates over time for very good/good sleep quality; comparable results were obtained for the PAR only and SAR and PAR subpopulations. Overall, the results of this NIS conducted in Sweden are consistent with those of the same NIS conducted in Ireland, despite some differences with respect to missing data and baseline characteristics.14 Taken together, these studies demonstrate real-world improvement in sleep quality with MP-AzeFlu treatment. Because sleep impairment (and associated daytime sleepiness) are debilitating symptoms of AR,15–20 improvement in sleep quality should be seen as an important benefit of MP-AzeFlu treatment.
These data also indicated that MP-AzeFlu nasal spray was well tolerated. The safety results of this study were generally consistent with the safety profile of MP-AzeFlu.6 In this study, two ADRs (lip pain and epistaxis) were reported in one patient (0.6%), neither of which was serious. Both ADRs started on the same day, lasted for 2 weeks, and resolved by the end of the observation. Bitter taste has been reported by patients in the Phase III trials of MP-AzeFlu.13,22,23 However, as this is a non-interventional study, included patients were already on other therapies (Aze or Flu). The patients were required to send their respective cards along with occurrence of adverse events (if any). However, the patients may not have found the bitter taste to be significant to be reported in the patient card.
In analyzing data from this NIS, missing data could be a source of bias. The data were complete for most baseline variables, except the duration of AR (data were missing in 17.4% [28 of 161] of patients). About one-fourth of patients (24.2%; 39 of 161) were missing data from Day 1 onward, indicating that their diary cards had not been completed and/or returned after the baseline visit; thus, these patients did not contribute to the effectiveness analysis. An additional 24 patients (14.9%) with postbaseline data discontinued MP-AzeFlu treatment, stopped documentation, and/or did not return all diary card(s) during the course of the study. However, analyses of VAS severity score for “completers” (those with documentation through Day 42) and “drop-outs” (those with documentation after Day 1 but not completed to Day 42) revealed similar results over the observation period (up to Day 28 for drop-outs). Finally, values obtained for Day 42 and for the last day of treatment/documentation were very similar. Thus, the time course seems not biased by selective loss of patients due to, for example, lack of effectiveness. This study was also limited by its noninterventional and observational character, including the lack of a control group and the lack of random assignment. Since this is a real-world study, it is difficult to have comparable baseline for control and treatment group. Patients were prescribed MP-AzeFlu according to the summary of product characteristics as in the real-world clinical practice. Similar design was done by Klimek et al in a non-interventional study in Germany.11 The sample size was targeted to allow for scientific value and evaluation of sub-populations.
PER is a distinct category of AR that merits special attention in the clinic, especially because of the potential for development of comorbidities, including asthma.2,21 Because long-term treatment may be required for PER, topical (intranasal) agents are favored over systemic treatments.2 MP-AzeFlu has previously been found safe and effective over 1-year of treatment.22,23 Results of our study demonstrate the benefits of MP-AzeFlu for patients with PER in the real world.
Limitations
The main limitations of this study were those typically associated with noninterventional, observational studies (ie, the lack of placebo or active comparator and random assignment). As it is a real world observational study, interventions like randomization were not possible. Data were complete for most variables at baseline besides of duration of allergic rhinitis (missing data in 17.4% of the patients) as well as number and duration of symptom flares (missing data 83.9% and 83.2% of the patients) but without impact on effectiveness results. About one-fourth (24.2%) of the patients had missing data from Day 1 on. This was because the diary card was not completed and/or returned at all after the baseline visit. Thus, these patients did not contribute to the effectiveness analysis. Even though there was a high dropout rate, patients were enrolled by 24 different sites, which ensures reduction in enrollment bias and also to get a representative population of Swedish AR patients. Recruited patients were majorly moderate-severe AR patients which represents the label of MP-AzeFlu.
Conclusion
The results of this prospective NIS showed that the patients who were prescribed MP-AzeFlu nasal spray in a real-life setting met the requirements of the prescribing information,6 including a diagnosis of moderate/severe AR. The results also indicated that patients with PER received fast symptom relief and achieved early symptom control after treatment with MP-AzeFlu nasal spray. After 1 day of treatment, 89% of patients had already rated their AR symptoms as “well controlled” or “partly controlled.” Although one patient reported two ADRs (lip pain and epistaxis), MP-AzeFlu nasal spray was considered to be well tolerated in this large patient population in a real-life setting in Sweden. Furthermore, the beneficial treatment effects of MP-AzeFlu nasal spray were observed in all subpopulations, irrespective of allergen type/type of AR, age, and sex. In addition, MP-AzeFlu also statistically significantly improved patients’ sleep quality. Due to the limitations of the study, it is difficult to conclude that the benefits seen are due to the medication or clinical improvement that would have happened spontaneously. The results will include regression to the mean due to missing data.
Statement of Ethics
Subjects (or their parents or guardians) have given their written informed consent. This investigation represented a NIS as defined by European regulations [European Union Directive 2001/20/EC, ICH E2E, European Medicines Agency Guideline on good pharmacovigilance practices (GVP)], ie, the rules imposed for this observational plan did not interfere with the physician’s common therapy. The study was carried out in accordance with the national laws and guidelines current at that time: LVFS 2003:6, LIF policy 2010:1. The study documents were submitted to the Ethics Committee (EC) in Stockholm for review. This EC provided a positive opinion during the session on 22 Oct 2014.
Acknowledgment
The authors acknowledge Arghya Bhattacharya and Aswin Kumar A, for medical writing support (Viatris). Data included in this manuscript have been previously presented at the European Academy of Allergy and Clinical Immunology Congress (P0653, P0655, and P1177) held June 17‒21, 2017, in Helsinki, Finland.
Funding
This study and medical writing support were funded by Mylan Inc., Canonsburg, PA, US (now Viatris).
Disclosure
P.S. reports being on the advisory board for Meda. J.S. has nothing to disclose. D.T.N. and H.C.K. are employees of Meda Pharma GmbH & Co. KG (A Mylan Company, now Viatris). The authors report no other conflicts of interest in this work.
References
1. Valovirta E, Myrseth SE, Palkonen S. The voice of the patients: allergic rhinitis is not a trivial disease. Curr Opin Allergy Clin Immunol. 2008;8(1):1–9. doi:10.1097/ACI.0b013e3282f3f42f
2. Bousquet J, Khaltaev N, Cruz AA, et al. Allergic rhinitis and its impact on asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and allergen). Allergy. 2008;63(Suppl 86):8–160. doi:10.1111/j.1398-9995.2007.01620.x
3. Bousquet J, Schünemann HJ, Hellings PW, et al. Macvia clinical decision algorithm in adolescents and adults with allergic rhinitis. J Allergy Clin Immunol. 2016;138(2):367–74. e2. doi:10.1016/j.jaci.2016.03.025
4. Bousquet PJ, Combescure C, Klossek JM, Daures JP, Bousquet J. Change in visual analog scale score in a pragmatic randomized cluster trial of allergic rhinitis. J Allergy Clin Immunol. 2009;123(6):1349–1354.
5. Demoly P, Bousquet PJ, Mesbah K, Bousquet J, Devillier P. Visual analogue scale in patients treated for allergic rhinitis: an observational prospective study in primary care: asthma and rhinitis. Clin Exp Allergy. 2013;43(8):881–888.
6. Spc dymista nasal spray; 2015. Available from: https://www.medicines.org.uk/emc/medicine/27579.
7. Klimek L, Bachert C, Stjarne P, et al. Mp-AzeFlu provides rapid and effective allergic rhinitis control in real life: a pan-European study. Allergy Asthma Proc. 2016;37(5):376–386.
8. Carr W, Bernstein J, Lieberman P, et al. A novel intranasal therapy of azelastine with fluticasone for the treatment of allergic rhinitis. J Allergy Clin Immunol. 2012;129(5):1282–9. e10.
9. Agache I, Doros IC, Leru PM, Bucur I, Poenaru M, Sarafoleanu C. Mp-AzeFlu provides rapid and effective allergic rhinitis control: results of a non-interventional study in Romania. Rhinology. 2018;56(1):33–41.
10. Dollner R, Lorentz Larsen P, Dheyauldeen S, Steinsvag S. A multicenter, prospective, noninterventional study in a Norwegian cohort of patients with moderate-to-severe allergic rhinitis treated with Mp-AzeFlu. Allergy Rhinol. 2017;8(3):148–156. doi:10.2500/ar.2017.8.0216
11. Klimek L, Bachert C, Mosges R, et al. Effectiveness of MP29-02 for the treatment of allergic rhinitis in real-life: results from a noninterventional study. Allergy Asthma Proc. 2015;36(1):40–47. doi:10.2500/aap.2015.36.3823
12. Bousquet J, Price D, Meltzer EO, et al. Onset of action for intranasal azelastine–fluticasone propionate versus oral loratadine with intranasal fluticasone propionate.
13. Meltzer EO, LaForce C, Ratner P, Price D, Ginsberg D, Carr W. MP29-02 (a novel intranasal formulation of azelastine hydrochloride and fluticasone propionate) in the treatment of seasonal allergic rhinitis: a randomized, double-blind, placebo-controlled trial of efficacy and safety. Allergy Asthma Proc. 2012;33(4):324–332. doi:10.2500/aap.2012.33.3587
14. Stjärne P, Pohl W, Kaulsay R. Mp-AzeFlu®* improves sleep quality in patients with persistent allergic rhinitis: data from Austria, Ireland and Sweden.
15. Benninger MS, Benninger RM. The impact of allergic rhinitis on sexual activity, sleep, and fatigue. Allergy Asthma Proc. 2009;30(4):358–365. doi:10.2500/aap.2009.30.3244
16. Craig TJ, Sherkat A, Safaee S. Congestion and sleep impairment in allergic rhinitis. Curr Allergy Asthma Rep. 2010;10(2):113–121. doi:10.1007/s11882-010-0091-5
17. Ferguson BJ. Influences of allergic rhinitis on sleep. Otolaryngol Head Neck Surg. 2004;130(5):617–629. doi:10.1016/j.otohns.2004.02.001
18. Storms W. Allergic rhinitis-induced nasal congestion: its impact on sleep quality. Prim Care Respir J. 2008;17(1):7–18. doi:10.3132/pcrj.2008.00001
19. Stull DE, Roberts L, Frank L, Heithoff K. Relationship of nasal congestion with sleep, mood, and productivity. Curr Med Res Opin. 2007;23(4):811–819. doi:10.1185/030079907X178793
20. Thompson A, Sardana N, Craig TJ. Sleep impairment and daytime sleepiness in patients with allergic rhinitis: the role of congestion and inflammation. Ann Allergy Asthma Immunol. 2013;111(6):446–451. doi:10.1016/j.anai.2013.05.020
21. Bousquet J, Annesi-Maesano I, Carat F, et al. Characteristics of intermittent and persistent allergic rhinitis: DREAMS study group. Clin Exp Allergy. 2005;35(6):728–732. doi:10.1111/j.1365-2222.2005.02274.x
22. Berger WE, Shah S, Lieberman P, et al. Long-term, randomized safety study of MP29-02 (a novel intranasal formulation of azelastine hydrochloride and fluticasone propionate in an advanced delivery system) in subjects with chronic rhinitis. J Allergy Clin Immunol Pract. 2014;2(2):179–185. doi:10.1016/j.jaip.2013.09.019
23. Price D, Shah S, Bhatia S, et al. A new therapy (MP29-02) is effective for the long-term treatment of chronic rhinitis. J Investig Allergol Clin Immunol. 2013;23(7):495–503.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.