Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Real-life effectiveness of indacaterol–glycopyrronium after switching from tiotropium or salmeterol/fluticasone therapy in patients with symptomatic COPD: the POWER study
Authors Kaplan A , Chapman KR , Anees SM, Mayers I, Rochdi D, Djandji M, Préfontaine D , McIvor A
Received 27 August 2018
Accepted for publication 29 November 2018
Published 18 January 2019 Volume 2019:14 Pages 249—260
DOI https://doi.org/10.2147/COPD.S185485
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Alan Kaplan,1 Kenneth R Chapman,2 Syed M Anees,3 Irvin Mayers,4 Driss Rochdi,5 Michel Djandji,5 David Préfontaine,5 Andrew McIvor6
1Family Physician Airways Group of Canada, University of Toronto, Toronto, ON, Canada; 2Division of Respiratory Medicine, Department of Medicine, University of Toronto, Toronto, ON, Canada; 3Schulich School of Medicine & Dentistry – Western University, University of Windsor, ON, Canada; 4Division of Pulmonary Medicine, Department of Medicine, University of Alberta, Edmonton, AB, Canada; 5Novartis Pharmaceuticals Canada Inc., Montreal, QC, Canada; 6Department of Medicine, McMaster University, Firestone Institute for Respiratory Health, Hamilton, ON, Canada
Purpose: In contrast to randomized controlled trials (RCTs), changes in maintenance pharmacotherapy in clinical practice occur without a washout period. The Prospective cohort study for the real-life effectiveness evaluation of glycOpyrronium With indacatERol combination in the management of COPD in Canada (POWER) study evaluated the real-life effectiveness of indacaterol/glycopyrronium (IND/GLY) following a direct switch from a long-acting muscarinic antagonist (LAMA, tiotropium) or long-acting β2-agonist (LABA)/inhaled corticosteroid (ICS) maintenance treatment (salmeterol/fluticasone [SFC]).
Methods: POWER was a single-cohort, prospective, multicenter, interventional study in which patients with moderate-to-severe COPD, who remained symptomatic on their current treatment of once-daily (od) tiotropium 18 µg or twice-daily (bid) SFC (any dose), were switched to treatment with open-label IND/GLY 110/50 µg od for 16 weeks. Effectiveness end points were change from baseline in trough FEV1, transition dyspnea index (TDI) total scores, and COPD assessment test (CAT) scores at 16 weeks.
Results: Trough FEV1 improved by 175 mL at Week 16 in patients who switched to IND/GLY. The change was 176 mL (95% CI: 135–217) when switched from tiotropium and 172 mL (95% CI: 85–258) when switched from SFC fixed-dose combination (FDC). At Week 16, significant improvements were observed in the mean TDI total scores (Δ=2.5) and CAT scores (Δ=-6.5) after the switch to IND/GLY treatment (both P<0.0001). Additionally, IND/GLY was well tolerated in patients with moderate-to-severe COPD, and no safety signal was observed.
Conclusion: In clinical practice settings, a direct switch from previous treatment with either tiotropium or SFC to IND/GLY was safe and provided superior clinically significant improvements in lung function and patient-related outcomes in patients with moderate-to-severe COPD.
Clinical trial registration: NCT02202616.
Keywords: COPD assessment test, dyspnea, FEV1, indacaterol/glycopyrronium, lung function, TDI
Introduction
COPD is a minimally reversible and progressive respiratory disease characterized by persistent or recurrent respiratory symptoms such as dyspnea, cough, and sputum production. It is considered one of the leading causes of morbidity and mortality worldwide.1 In Canada, COPD is projected to be the third most common cause of mortality by 2020.2 COPD has a major socioeconomic impact, contributing to an average total annual cost per patient ranging between CAN$2,444 from a patient perspective and CAN$6,693 from a social perspective, with cost increasing with severity of the disease.2
The GOLD strategy recommends long-acting muscarinic antagonists (LAMAs) and/or long-acting β2-agonists (LABAs) and LABA/inhaled corticosteroids (ICSs) as the maintenance treatment for patients with COPD, depending on the disease severity.3 In Canada, the Canadian Thoracic Society (CTS) has issued recommendations for the pharmacological management of COPD to reduce symptoms and prevent exacerbations. The recommended therapy is long-acting bronchodilator monotherapy for mild disease, dual bronchodilation (with LABA and LAMA) for more severe disease, and finally triple therapy (with LABA/ICS and LAMA), if increasing disease burden is characterized by frequent exacerbations, with elevated peripheral blood eosinophils, a history and/or concomitant asthma.4–6 However, real-life assessments of clinical practice have documented not only that a significant proportion of patients remain symptomatic despite bronchodilator monotherapy but also that ICS-containing maintenance medications are overprescribed in COPD patients, especially in those who are at low risk of exacerbations and mainly treated with LABA/ICS fixed-dose combinations (FDCs).7–10 The long-term use of ICS in COPD patients increases the risk of significant side effects such as pneumonia, osteoporosis, and mycobacterial disease.11 Considering the recurrent symptom burden despite treatment, the risk-to-benefit ratio associated with the chronic use of ICS in COPD,12 as well as the recent evidence that ICS withdrawal has limited effect on lung function and health status, maintenance treatment with an LABA/LAMA dual bronchodilator has become an optimal treatment approach for the majority of patients with symptomatic COPD, especially those at low risk of exacerbations and without a documented asthma–COPD overlap.11,13,14
The efficacy and tolerability of once-daily (od) indacaterol/glycopyrronium (IND/GLY; 110 μg/50 μg) vs placebo and/or active therapies are established in patients with moderate-to-very-severe COPD on the basis of pivotal randomized controlled trials (RCTs).15–18 Collectively, these studies demonstrated the superiority of IND/GLY compared with placebo and also compared with LAMA monotherapy and LABA/ICS combination therapy. However, real-world studies are needed to investigate LABA/LAMA effectiveness after a direct treatment switch in the clinical setting.19 Prospective cohort study for the real-life effectiveness evaluation of glycOpyrronium With indacatERol combination in the management of COPD in Canada (POWER) was a 16-week Canadian study, which aimed at evaluating the real-life effectiveness of a direct switch from usual treatment, either with od tiotropium 18 μg (LAMA) or with a twice-daily (bid) FDC of salmeterol/fluticasone (SFC, at any dose), to open-label IND/GLY in terms of lung function, dyspnea, and impact on health status by strictly enrolling symptomatic COPD patients with moderate-to-severe airflow limitation at low risk of exacerbation and not previously treated with a LAMA, plus a LABA and an ICS triple maintenance therapy. In this context, POWER assessed COPD patients’ benefits of escalating treatment from either LAMA or LABA/ICS to IND/GLY in the real-life setting.
Methods
Study design
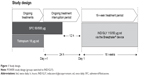
This was a real-life, multicenter, post-approval, prospective, 16-week interventional, open-label, single-arm study conducted in 45 primary (community general practitioners) and secondary (community specialists) centers from the provinces of Ontario and Quebec, Canada. Patients who consented and fulfilled all inclusion/exclusion criteria were instructed to interrupt their ongoing maintenance treatment regimen for 24 hours for patients on od tiotropium (18 μg via Handihaler device; Boehringer Ingelheim, Ingelheim, Germany), or 12 hours for patients on bid SFC FDC (any dose, any device; GlaxoSmithKline plc, London, UK), to allow baseline assessment. At randomization, all patients received open-label maintenance treatment with an FDC of IND/GLY 110/50 μg (Novartis Pharma AG, Basel, Switzerland) over a 16-week active treatment period. Clinical effectiveness and safety outcomes were collected at Weeks 4, 12, and 16. After the end of the 16-week active treatment period, a 30-day safety follow-up was completed for all patients (Figure 1). The study was sponsored by Novartis International AG and was performed according to the Declaration of Helsinki and the International Conference on Harmonization and Good Clinical Practice guidelines. The protocol was approved by an independent organization, ie, central ethics committee for all the participating sites (IRB Services, Aurora, Ontario, Canada). All patients provided written informed consent (ClinicalTrials.gov number: NCT02202616).
Patients
The study included patients aged >40 years, with physician-diagnosed COPD as per the GOLD 2011 criteria, a moderate-to-severe airflow limitation indicated by a pre-dose trough FEV1 ≥30 and <80% of predicted, a smoking history of >10 pack-years, an ongoing maintenance treatment with either tiotropium 18 μg od or SFC FDC bid (with no restriction on the prescribed dose) for a minimum of 6 weeks while demonstrating persistence of COPD, and impact on their health status/symptoms with a COPD assessment test (CAT) score of >10. Patients enrolled in POWER received treatment with IND/GLY as per the Canadian product monograph. Patients were excluded from the study if they formerly received maintenance triple therapy (with a LABA, a LAMA, and an ICS) for COPD, had a diagnosis/history of asthma, or had two or more moderate-to-severe exacerbations during the 12 months prior to study enrolment. A moderate COPD exacerbation was defined by requirement for the treatment with systemic corticosteroids and/or antibiotics, and a severe COPD exacerbation was defined by hospitalization, including an emergency room visit of longer than 24 hours.20
End points and outcomes measured
The primary effectiveness end point was the absolute change from baseline in pre-dose trough FEV1 after 16 weeks of treatment. Secondary effectiveness end points included change in pre-dose trough FEV1 between baseline and 4 weeks of treatment, change in the CAT score after 4 and 16 weeks of treatment vs baseline, and change from baseline in dyspnea index (transition dyspnea index [TDI]) at Weeks 4 and 16. Finally, safety was assessed by monitoring adverse events (AEs) and serious AEs (SAEs) during the study and the follow-up period.
Statistical analyses
Effectiveness end points were analyzed in the intention-to-treat (ITT) population, which included all patients who received the study treatment and had at least one post-baseline assessment. A confirmatory analysis of the primary effectiveness end point was performed in the per-protocol (PP) population, which comprised patients who completed the 16-week treatment period without any major protocol deviation. The 95% CIs of the change from baseline in primary and secondary effectiveness end points were used to assess the precision of the estimate and to make inferences to the target population. A subgroup analysis of the primary effectiveness analyses was conducted according to disease-relevant baseline characteristics (ie, age, gender, GOLD stage, smoking status, and exacerbation history in the prior year). Safety set comprised patients who received at least one dose of IND/GLY and had at least one post-baseline visit.
Results
Demographics and baseline characteristics
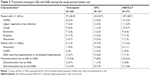
Of the 401 patients screened in this study, 377 patients switched to IND/GLY and 338 patients belonged to the intent-to-treat group (248 from tiotropium and 87 from SFC FDC; three with unreported former medication). A total of 301 patients (75.1%) completed the study. Patient disposition is presented in Figure 2. The most common reason for discontinuation was AEs. The majority of patients were men (55.9%), were Caucasian (97.6%), had a CAT score of moderate severity (11–20), and suffered from moderate COPD (66.9%). Demographic and baseline characteristics of patients are summarized in Table 1.
  | Figure 2 Patient disposition. |
Impact of a direct switch to IND/GLY on lung function
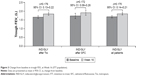
In the ITT population, IND/GLY demonstrated a clinically meaningful and statistically superior mean improvement of 175 mL in trough FEV1 at Week 16 after switching from tiotropium (change from baseline [Δ]=176 mL; 95% CI: 135–217; Figure 3) and SFC FDC (Δ=172 mL; 95% CI: 85–258). Results of pre-dose trough FEV1 for the PP population were consistent with those of the ITT population, showing a mean improvement of 202 mL (95% CI: 161–242) at Week 16.
At Week 4, the mean change from baseline in trough FEV1 with IND/GLY was 142 mL in patients who switched from tiotropium and 118 mL for patients who switched from SFC FDC. An overall change of 137 mL in trough FEV1 (Figure 4) was observed in patients after switching to IND/GLY at Week 4.
Impact of a direct switch to IND/GLY on dyspnea
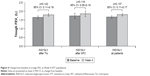
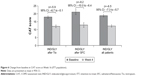
IND/GLY demonstrated significantly superior improvement in TDI total scores for patients who switched from tiotropium and SFC FDC, both at Weeks 4 and 16 (all P<0.0001). At Week 16, the mean change in TDI total scores by IND/GLY treatment was significant for the ITT patient population who switched from tiotropium (Δ=2.4 units; 95% CI: 2.05–2.76) and SFC FDC (Δ=2.9 units; 95% CI: 2.15–3.57; Figure 5). Similarly significant improvements were observed with IND/GLY treatment at Week 4 for both groups of patients previously treated with tiotropium and SFC FDC (data not shown).
Impact of a direct switch to IND/GLY on health status
Statistically significant improvements from baseline in the mean total CAT score were observed with IND/GLY treatment at both Weeks 4 and 16 for patients who switched from tiotropium and SFC FDC (all P<0.0001). At Week 16, a significant improvement in health status in terms of improvement in the CAT score was observed with IND/GLY treatment in patients who switched from tiotropium and SFC FDC (Figure 6). Similarly, a significant improvement in IND/GLY treatment for both groups of patients (tiotropium [Δ=−4.7 points, 95% CI: −5.4 to −3.9] and SFC FDC [Δ=−5.9 points, 95% CI: −7.6 to −4.2]) was observed at Week 4.
Impact of a direct switch to IND/GLY on lung function by subgroups
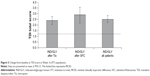
Improvement in lung function 16 weeks after switching to IND/GLY was unrelated to gender, age, severity of COPD (between GOLD 2 and 4 spirometric criteria), and exacerbation history in the previous year. Of note, patients in GOLD 1 category did not show a significant change in lung function, which may be related to the smaller sample size and a better preserved baseline lung function of patients in that group (Figure 7). Except for the smallest subgroup of GOLD 1, all other patient subgroups exhibited lung function improvements with effect sizes in the range of clinical significance (≥100 mL change from baseline trough FEV1). Men showed greater benefits than women; however, both genders presented with an average change in FEV1 from baseline to Week 16 of at least 100 mL. Although both current and former smokers showed benefit in mean FEV1 that exceeded 100 mL after switching, the benefit was greater in former smokers. Finally, comparisons between tiotropium and SFC (ie, previous COPD medication) subgroups in change from baseline to Week 16 in trough FEV1 demonstrated no statistically significant treatment difference (TD) in terms of gender, age category, smoking history, severity of COPD, and exacerbation history in the previous year (ITT population; data not shown).
  | Figure 7 Change from baseline in trough FEV1 at Week 16 by subgroups. |
Safety
IND/GLY was well tolerated in patients with moderate-to-severe COPD, who switched from tiotropium and SFC FDC. Treatment-emergent AEs were balanced between tiotropium and SFC starters (Table 2). The most frequently reported AE was COPD (3.5%). Patients who switched from SFC reported more pneumonia AEs and SAEs than those formerly treated with tiotropium (five AEs and three SAEs for SFC vs two and one for tiotropium starters, respectively). Twelve patients (3.2%) experienced at least one SAE during the study, with the main SAEs being COPD and pneumonia. Of the four cases of pneumonia SAEs (three from patients formerly on SFC), two cases were investigated by chest X-ray, but only one was confirmed. There was no imbalance between tiotropium and SFC starters in the proportion of patients who discontinued the study due to an AE or an SAE. There were no patient deaths during the study, and no new safety signals were identified with IND/GLY treatment (Table 2).
Discussion
POWER is a real-world study demonstrating the effectiveness of IND/GLY in the management of symptomatic patients previously treated with tiotropium or SFC and is therefore highly relevant to clinical practice. Patients from the POWER study were formerly treated either with od tiotropium or with bid SFC FDC prior to enrolment and switched directly to open-label IND/GLY, reflecting a typical clinical practice approach. This study acknowledges the fact that many COPD patients experience persistent symptoms despite long-acting bronchodilator monotherapy,21 as all patients initially presented with a CAT score of >10. Patients with moderate-to-severe COPD who remained symptomatic despite tiotropium or SFC FDC and who directly switched to IND/GLY showed significant improvements in lung function, dyspnea, and health-related quality of life. The effectiveness outcomes in the POWER study all exceeded the minimal clinically important difference (MCID) and were superior to those observed in published RCTs.
The primary objective of the POWER study was achieved by demonstrating an improvement in trough FEV1 by IND/GLY in patients who switched directly from either tiotropium or SFC to IND/GLY. A majority of patients reached the MCID of 100 mL for trough FEV1 after switching to IND/GLY from previous treatments. Clinically relevant lung function improvements from baseline were seen as early as 4 weeks after treatment inception. Regardless of the former maintenance treatment, mean lung function benefits from the switch to IND/GLY exceeded MCID in all but one patient subgroup, namely the subset of patients with mild airflow limitation for which limited sample size precludes any extrapolation. The effect of IND/GLY on lung function has been well established in many clinical trials.16,18 However, differences in study design, ie, former treatment washout and in study populations, prevent any direct comparison with this study. For example, studies such as FLAME16 and SPARK20 compared IND/GLY to SFC 50/500 μg bid and tiotropium, respectively, both in patients with more advanced disease, ie, moderate to very severe airflow limitation and a history of exacerbation in the previous year. In the SHINE study, patients discontinued long-acting bronchodilators at least 14 days prior to randomization, whereas patients in POWER only skipped one dose of the former maintenance regimen prior to starting IND/GLY treatment the next morning.18 As opposed to double-blind RCTs of IND/GLY vs SFC at a dose of 50/500 μg bid including ILLUMINATE, LANTERN, and FLAME,15,16,22 a majority of SFC patients who switched to IND/GLY in POWER were on a lower dose of 50/250 μg bid, which may have contributed to the greater effect size observed. Finally, the 12-week CRYSTAL study, which was also a direct switch but active-controlled study, reported improvements in trough FEV1 of 71 mL after switching to IND/GLY from LABA + ICS and 101 mL after switching from LABA or LAMA monotherapies.23 Whether a direct switch back from dual bronchodilation to LAMA monotherapy or LABA/ICS FDC would lead to worsening in the measured clinical outcomes remains a matter of debate. There is insufficient evidence in stable COPD to determine whether treatment step-down can be safe and/or without reducing patient benefits; treatment step-down should only be considered in patients who did not benefit from previous step-up.5 According to the GOLD 2017 strategy, escalation to long-acting dual bronchodilators may be considered if symptoms are not improved with existing monotherapy.1,22 However, LABA/ICS FDCs are not recommended as a preferred maintenance treatment choice for low-risk COPD patients with mild/moderate airflow limitations, as overuse of ICS is associated with AEs.11 Interestingly, COPD patients formerly on SFC enrolled in POWER were mostly treated with ICS doses lower than 500 μg bid, which may reflect a clinical trend toward reducing ICS doses in consideration of the long-term side effect in COPD patients; however, ICS overuse is still widespread even in low-risk COPD patients.9 A majority of patients (66.9%) in the POWER study had moderate airflow limitation. This study showed that IND/GLY was effective in improving dyspnea in patients who switched from tiotropium or SFC FDC. These findings support results from 26-week SHINE and ILLUMINATE studies where IND/GLY significantly improved the TDI vs tiotropium (TD=0.51 units) and SFC (TD=0.76 units).15,18 The average TDI improvement in POWER exceeded the MCID of ≥1 unit similar to that observed in the pragmatic, active-control CRYSTAL study.23
Improvements in lung function, symptoms, and quality of life represent the major needs for patients with COPD. CAT is one of the most commonly used questionnaires for assessing the health-related quality of life in COPD patients.24 As previously reported, IND/GLY treatment improves the quality of life in COPD patients.23 Consistent with previously published data, POWER further validates those results, by demonstrating clinically relevant improvement in the CAT score with IND/GLY treatment in patients who switched from tiotropium or SFC FDC, with average changes from baseline in the CAT score exceeding the MCID of two units.25,26 The POWER health status data are aligned with the DACCORD study, which also reported clinically meaningful benefits using the CAT total score in COPD patients who switched from monobronchodilation to dual bronchodilation.27
IND/GLY was well tolerated in patients with moderate-to-severe COPD, who switched from tiotropium and SFC FDC. Importantly, few discontinuations took place after the switch, and there was no imbalance between the rate of SFC or tiotropium patients who discontinued from the study due to AEs or SAEs; no significant imbalance in treatment-emergent AEs resulting from ICS withdrawal was observed. The most frequently reported AE was COPD, with no patient deaths reported and no new safety signals emerging from the study. The frequency of treatment-emergent SAEs and those requiring hospitalization or prolonged hospitalization was low but numerically greater among patients who switched to IND/GLY from SFC vs tiotropium (7.9% vs 1.5%, and 5% vs 0.7%, respectively). This signal may reflect the imbalance in COPD exacerbations and pneumonia, which occurred more frequently among SFC starters. Studies documented not only the risk of pneumonia associated with long-term ICS use but also time-dependent gradual waning of this risk after stopping ICS over approximately 6 months;28 whether patients formerly on SFC could have carried an increased risk of pneumonia after the IND/GLY switch remains unclear.
This study was designed to complement previous RCTs, by providing information on a direct switch to IND/GLY under routine clinical practice conditions, and some limitations should be noted. First, the study could not fully reflect real-world clinical practice as study subjects were enrolled based on a set of inclusion/exclusion criteria reported earlier. Nevertheless, the POWER inclusion/exclusion criteria reflected the Canadian product monograph and aimed at limiting confounding factors that could have influenced the study outcomes. Second, the open-label single-arm study design inherently includes the risk of response bias, especially applicable to self-reported patient-reported outcomes such as dyspnea and health status scores. However, the primary effectiveness outcome of change from baseline in trough FEV1 is less subject to bias. The short study duration also precludes extrapolation of the impact of this switch from LAMA (tiotropium) or especially from LABA/ICS (SFC) to IND/GLY, considering the potential withdrawal effect from the ICS component. A majority of patients enrolled in POWER were formerly on tiotropium monotherapy (73%), which limits our ability to draw conclusion for subjects formerly on SFC. Nevertheless, our results are consistent with the 6-month real-life OPTIMO switch study, which similarly suggested that low-risk COPD patients on LABA/ICS could be safely withdrawn from an ICS therapy and switched to maintenance bronchodilator therapy.13 Moreover, withdrawal of ICS in patients with severe COPD in the WISDOM study resulted in no impact on exacerbation within the 9-month period after complete ICS withdrawal.14 In line with the GOLD 2017 consensus document, the CTS COPD management guideline does not recommend LABA/ICS maintenance therapy in the absence of a LAMA.4 This contrasts with the GOLD 2017 report, which keeps LABA/ICS as an alternative choice to LABA/LAMA in GOLD group C patients not adequately controlled with LAMA monotherapy.3 Interestingly, in patients with moderate COPD and heightened cardiovascular risk, treatment with LABA/ICS FDC vilanterol/fluticasone furoate did not affect mortality or cardiovascular outcomes;29 in this study, LABA/ICS reduced lung function decline vs placebo, but results should be interpreted with caution given the primary and other secondary end points were not met. The common prescription of ICS-containing maintenance medications in low-risk COPD patients10 may be a result of inappropriate use of spirometry and lack of differential diagnosis of asthma and COPD, which may explain why some patients in POWER formerly received SFC at doses typically recommended for asthma.
The POWER study preceded the emergence of baseline blood eosinophils as a potential biomarker to assess the benefit-to-risk ratio of ICS-containing treatment regimen in patients with COPD;30,31 blood eosinophil data are not available. The FLAME study showed that there is no eosinophil cutoff at which IND/GLY was inferior to SFC in terms of exacerbation prevention.32,33 Post hoc and prospective data from ICS withdrawal studies,34,35 respectively, suggested that COPD patients with peripheral blood eosinophils >300 cells/μL and a former history of frequent exacerbation had more exacerbations when ICS was withdrawn in a stepwise fashion and that patients without a history of frequent exacerbation while on long-term triple therapy exacerbated more when abruptly de-escalated from their ICS if their blood eosinophils were >300 cells. In the SUNSET study, these patients represented about 20% of the patients formerly receiving a LAMA + LABA/ICS.35 Assessing the clinical value of blood eosinophil biomarker in the real-life setting and its potential association with pneumonias and/or exacerbations after ICS withdrawal is certainly desirable.
This study supports that a switch to dual bronchodilation is an appropriate strategy for the management of patients with moderate-to-severe COPD at low risk, but with persistent symptoms despite LAMA or LABA/ICS therapy.7,9 Studies have recently reported some benefits of triple therapy FDC in low-risk COPD patients vs LABA/ICS FDC.36–38 Besides, benefits of triple therapy FDC beyond LABA/LAMA FDC were mainly described in patients with a history of frequent exacerbations39 and those with one or more exacerbation and severe airflow limitation;40 however, designs (abrupt ICS withdrawal effects) and patient populations (with/without former asthma history) from these studies were suspected to influence results.41,42 ICS withdrawal should always be considered with caution and on a case-by-case basis: ICS as an add-on to LABA + LAMA benefited to a subgroup of COPD patients, especially those with frequent exacerbations despite dual bronchodilator use, particularly if blood eosinophils are >300 cells/μL and a history of and/or concomitant asthma.6 One should note that recent evidence on the benefits of ICS add-on or triple therapy beyond IND/GLY exceeds the scope of this study and is better addressed by SUNSET;35 POWER strictly excluded all patients formerly receiving LAMA plus LABA/ICS triple therapy. Patients with COPD and a history of frequent exacerbations were also excluded from this study; therefore, POWER was not designed to assess the benefits from the IND/GLY16,20 or other dual bronchodilators43 in exacerbation-prone patients. In line with the GOLD 2017 strategy and the CTS recommendations, the POWER results further support LAMA or LABA/ICS to IND/GLY step-up in bronchodilation in patients who remain symptomatic according to the CAT score.
Conclusion
In the POWER study, a real-life switch to IND/GLY demonstrated clinically relevant improvements in lung function, dyspnea, and health-related quality of life after 16 weeks of treatment in symptomatic patients with moderate-to-severe COPD formerly treated with tiotropium monotherapy or SFC FDC. IND/GLY switch was well tolerated, with no new safety signals emerging from the study. Given the clinical effectiveness outcomes seen in this single-arm study exceeded both the MCID and the results observed in previous RCTs, the POWER study further reinforces the choice of IND/GLY over LAMA monotherapy or SFC FDC for patients with COPD and persistent symptoms.
Data sharing statement
Novartis is committed to sharing with qualified external researchers, access to patient-level data, and supporting clinical documents from eligible studies. These requests are reviewed and approved by an independent review panel on the basis of scientific merit. All data provided are anonymized to respect the privacy of patients who have participated in the trial in line with applicable laws and regulations. Result summaries have been posted on the Novartis clinical trial database and other online public databases. More information on Novartis’ position on access to clinical trial results and patient-level data is available at: https://www.novartis.com/our-science/clinical-trials/clinical-trial-information-disclosure.
Acknowledgments
The authors thank all principal investigators and patients involved in the study. Writing and editorial assistance for this manuscript were provided by Chiranjit Ghosh and M Fahad Haroon (Novartis Healthcare Pvt. Ltd., India) and was funded by Novartis Pharmaceuticals Canada Inc., Montreal, Québec, Canada, in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3). The authors also acknowledge the contribution of Dr John Sampalis et al at JSS Medical Research (Saint-Laurent, Québec, Canada) for their assistance with study monitoring and interim analysis. The study was supported and funded by Novartis Pharmaceuticals Canada Inc. The abstract of this study was presented at the ATS conference 2018 as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” in American Journal of Respiratory and Critical Care Medicine 2018: https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2018.197.1_MeetingAbstracts.A3031.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
AK reports nonfinancial support from Novartis, during the conduct of the study; personal fees from Novartis, Boehringer Ingelheim, AstraZeneca, Teva, Pfizer, Sanofi, Purdue, and Paladdin; and grants and personal fees from Benton Dickinson, outside the submitted work. KRC reports grants and personal fees from AstraZeneca, grants and personal fees from Boehringer Ingelheim, grants from Baxter, grants and personal fees from CSL Behring, grants and personal fees from Grifols, grants from GlaxoSmithKline, grants and personal fees from Sanofi, grants and personal fees from Genentech, grants and personal fees from Kamada, grants from Amgen, grants and personal fees from Roche, grants and personal fees from Novartis, personal fees from Merck, and personal fees from CIHR-GSK Research Chair in Respiratory Health Care Deliveryat the University Health Network, during the conduct of the study. IM reports honoraria for continuing medical education related to COPD and asthma. DR is an employee of and reports personal fees from Novartis Pharmaceuticals Canada Inc. MD was a former employee of Novartis Pharmaceuticals Canada Inc. during this study. SMA reports clinical trial fees and speaking fees from Novartis. DP is an employee of and reports personal fees from Novartis Pharmaceuticals Canada Inc. DP also reports personal fees from Novartis Pharma AG, during the conduct of the study. AM reports honoraria for attending advisory boards and providing CME for AstraZeneca, Boehringer Ingelheim, Novartis, and Takeda. The authors report no other conflicts of interest in this work.
References
Tashkin DP, Ferguson GT. Combination bronchodilator therapy in the management of chronic obstructive pulmonary disease. Respir Res. 2013;14:49. | ||
Dang-Tan T, Ismaila A, Zhang S, Zarotsky V, Bernauer M. Clinical, humanistic, and economic burden of chronic obstructive pulmonary disease (COPD) in Canada: a systematic review. BMC Res Notes. 2015;8(1):464. | ||
Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease; 2017. | ||
O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease – 2007 update. Can Respir J. 2007;14(Suppl B):5B–32B. | ||
Bourbeau J, Bhutani M, Hernandez P, et al. CTS position statement: pharmacotherapy in patients with COPD – an update. Canadian Journal of Respiratory, Critical Care, and Sleep Medicine. 2017;1(4):222–241. | ||
Agusti A, Fabbri LM, Singh D, et al. Inhaled corticosteroids in COPD: Friend or foe? Eur Respir J. Epub 2018 Sep 6. | ||
Vestbo J, Vogelmeier C, Small M, Higgins V. Understanding the GOLD 2011 Strategy as applied to a real-world COPD population. Respir Med. 2014;108(5):729–736. | ||
Bourbeau J, Sebaldt RJ, Day A, et al. Practice patterns in the management of chronic obstructive pulmonary disease in primary practice: the CAGE study. Can Respir J. 2008;15(1):13–19. | ||
Price D, West D, Brusselle G, et al. Management of COPD in the UK primary-care setting: an analysis of real-life prescribing patterns. Int J Chron Obstruct Pulmon Dis. 2014;9:889–905. | ||
Hernandez P, Balter MS, Bourbeau J, Chan CK, Marciniuk DD, Walker SL. Canadian practice assessment in chronic obstructive pulmonary disease: respiratory specialist physician perception versus patient reality. Can Respir J. 2013;20(2):97–105. | ||
Rossi A, van der Molen T, del Olmo R, et al. INSTEAD: a randomised switch trial of indacaterol versus salmeterol/fluticasone in moderate COPD. Eur Respir J. 2014;44(6):1548–1556. | ||
Price D, Yawn B, Brusselle G, Rossi A. Risk-to-benefit ratio of inhaled corticosteroids in patients with COPD. Prim Care Respir J. 2013;22(1):92–100. | ||
Rossi A, Guerriero M, Corrado A; OPTIMO/AIPO Study Group. Withdrawal of inhaled corticosteroids can be safe in COPD patients at low risk of exacerbation: a real-life study on the appropriateness of treatment in moderate COPD patients (OPTIMO). Respir Res. 2014;15(1):77. | ||
Magnussen H, Disse B, Rodriguez-Roisin R, et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014;371(14):1285–1294. | ||
Vogelmeier CF, Bateman ED, Pallante J, et al. Efficacy and safety of once-daily QVA149 compared with twice-daily salmeterol-fluticasone in patients with chronic obstructive pulmonary disease (ILLUMINATE): a randomised, double-blind, parallel group study. Lancet Respir Med. 2013;1(1):51–60. | ||
Wedzicha JA, Banerji D, Chapman KR, et al. Indacaterol-Glycopyrronium versus Salmeterol-Fluticasone for COPD. N Engl J Med. 2016;374(23):2222–2234. | ||
Mahler DA, Decramer M, D’Urzo A, et al. Dual bronchodilation with QVA149 reduces patient-reported dyspnoea in COPD: the BLAZE study. Eur Respir J. 2014;43(6):1599–1609. | ||
Bateman ED, Ferguson GT, Barnes N, et al. Dual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE study. Eur Respir J. 2013;42(6):1484–1494. | ||
Ford I, Norrie J, Trials P. Pragmatic Trials. N Engl J Med. 2016;375(5):454–463. | ||
Wedzicha JA, Decramer M, Ficker JH, et al. Analysis of chronic obstructive pulmonary disease exacerbations with the dual bronchodilator QVA149 compared with glycopyrronium and tiotropium (SPARK): a randomised, double-blind, parallel-group study. Lancet Respir Med. 2013;1(3):199–209. | ||
Dransfield MT, Bailey W, Crater G, Emmett A, O’Dell DM, Yawn B. Disease severity and symptoms among patients receiving monotherapy for COPD. Prim Care Respir J. 2011;20(1):46–53. | ||
Zhong N, Wang C, Zhou X, et al. LANTERN: a randomized study of QVA149 versus salmeterol/fluticasone combination in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:1015–1026. | ||
Vogelmeier CF, Gaga M, Aalamian-Mattheis M, et al. Efficacy and safety of direct switch to indacaterol/glycopyrronium in patients with moderate COPD: the CRYSTAL open-label randomised trial. Respir Res. 2017;18(1):140. | ||
Jones PW, Brusselle G, dal Negro RW, et al. Properties of the COPD assessment test in a cross-sectional European study. Eur Respir J. 2011;38(1):29–35. | ||
Smid DE, Franssen FM, Houben-Wilke S, et al. Responsiveness and MCID Estimates for CAT, CCQ, and HADS in Patients With COPD Undergoing Pulmonary Rehabilitation: A Prospective Analysis. J Am Med Dir Assoc. 2017;18(1):53–58. | ||
Kon SS, Canavan JL, Jones SE, et al. Minimum clinically important difference for the COPD Assessment Test: a prospective analysis. Lancet Respir Med. 2014;2(3):195–203. | ||
Buhl R, Criée CP, Kardos P, et al. Dual bronchodilation vs triple therapy in the “real-life” COPD DACCORD study. Int J Chron Obstruct Pulmon Dis. 2018;13:2557–2568. | ||
Suissa S, Patenaude V, Lapi F, Ernst P. Inhaled corticosteroids in COPD and the risk of serious pneumonia. Thorax. 2013;68(11):1029–1036. | ||
Vestbo J, Anderson JA, Brook RD, et al. Fluticasone furoate and vilanterol and survival in chronic obstructive pulmonary disease with heightened cardiovascular risk (SUMMIT): a double-blind randomised controlled trial. Lancet. 2016;387(10030):1817–1826. | ||
Suissa S, Ernst P. Precision Medicine Urgency: The Case of Inhaled Corticosteroids in COPD. Chest. 2017;152(2):227–231. | ||
Pascoe S, Locantore N, Dransfield MT, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir Med. 2015;3(6):435–442. | ||
Roche N, Chapman KR, Vogelmeier CF, et al. Blood eosinophils and response to maintenance chronic obstructive pulmonary disease treatment. Data from the FLAME Trial. Am J Respir Crit Care Med. 2017;195(9):1189–1197. | ||
Papi A, Kostikas K, Wedzicha JA, et al. Dual bronchodilation response by exacerbation history and eosinophilia in the FLAME study. Am J Respir Crit Care Med. 2018;197(7):1223–1226. | ||
Watz H, Tetzlaff K, Wouters EF, et al. Blood eosinophil count and exacerbations in severe chronic obstructive pulmonary disease after withdrawal of inhaled corticosteroids: a post-hoc analysis of the WISDOM trial. Lancet Respir Med. 2016;4(5):390–398. | ||
Chapman KR, Hurst JR, Frent SM, et al. Long-term triple therapy de-escalation to indacaterol/glycopyrronium in patients with chronic obstructive pulmonary disease (SUNSET): a randomized, double-blind, triple-dummy clinical trial. Am J Respir Crit Care Med. 2018;198(3):329–339. | ||
Singh D, Papi A, Corradi M, et al. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting β2-agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388(10048):963–973. | ||
Lipson DA, Barnacle H, Birk R, et al. FULFIL Trial: Once-daily triple therapy for patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017;196(4):438–446. | ||
Ferguson GT, Rabe KF, Martinez FJ, et al. Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, phase 3 randomised controlled trial. Lancet Respir Med. 2018;6(10):747–758. | ||
Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–1680. | ||
Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–1084. | ||
Agusti A. Filling the gaps in COPD: the TRIBUTE study. Lancet. 2018;391(10125):1004–1006. | ||
Suissa S, Drazen JM. Making sense of triple inhaled therapy for COPD. N Engl J Med. 2018;378(18):1723–1724. | ||
Calverley PMA, Anzueto AR, Carter K, et al. Tiotropium and olodaterol in the prevention of chronic obstructive pulmonary disease exacerbations (DYNAGITO): a double-blind, randomised, parallel-group, active-controlled trial. Lancet Respir Med. 2018;6(5):337–344. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.